[1]
Kwon DI, Miles BA, Education Committee of the American Head and Neck Society (AHNS). Hypopharyngeal carcinoma: Do you know your guidelines? Head & neck. 2019 Mar:41(3):569-576. doi: 10.1002/hed.24752. Epub 2018 Dec 20
[PubMed PMID: 30570183]
[2]
Hoffman HT, Karnell LH, Shah JP, Ariyan S, Brown GS, Fee WE, Glass AG, Goepfert H, Ossoff RH, Fremgen AM. Hypopharyngeal cancer patient care evaluation. The Laryngoscope. 1997 Aug:107(8):1005-17
[PubMed PMID: 9260999]
[3]
Hall SF, Groome PA, Irish J, O'Sullivan B. The natural history of patients with squamous cell carcinoma of the hypopharynx. The Laryngoscope. 2008 Aug:118(8):1362-71. doi: 10.1097/MLG.0b013e318173dc4a. Epub
[PubMed PMID: 18496152]
[4]
Pracy P, Loughran S, Good J, Parmar S, Goranova R. Hypopharyngeal cancer: United Kingdom National Multidisciplinary Guidelines. The Journal of laryngology and otology. 2016 May:130(S2):S104-S110
[PubMed PMID: 27841124]
[5]
Kuo P, Chen MM, Decker RH, Yarbrough WG, Judson BL. Hypopharyngeal cancer incidence, treatment, and survival: temporal trends in the United States. The Laryngoscope. 2014 Sep:124(9):2064-9
[PubMed PMID: 25295351]
[6]
Simard EP, Torre LA, Jemal A. International trends in head and neck cancer incidence rates: differences by country, sex and anatomic site. Oral oncology. 2014 May:50(5):387-403. doi: 10.1016/j.oraloncology.2014.01.016. Epub 2014 Feb 13
[PubMed PMID: 24530208]
[7]
Bakshi SS. PLUMMER VINSON SYNDROME--is it common in males? Arquivos de gastroenterologia. 2015 Jul-Sep:52(3):250-2. doi: 10.1590/S0004-28032015000300018. Epub
[PubMed PMID: 26486296]
[8]
Marchand JL, Luce D, Leclerc A, Goldberg P, Orlowski E, Bugel I, Brugère J. Laryngeal and hypopharyngeal cancer and occupational exposure to asbestos and man-made vitreous fibers: results of a case-control study. American journal of industrial medicine. 2000 Jun:37(6):581-9
[PubMed PMID: 10797501]
Level 2 (mid-level) evidence
[9]
Riley CA, Wu EL, Hsieh MC, Marino MJ, Wu XC, McCoul ED. Association of Gastroesophageal Reflux With Malignancy of the Upper Aerodigestive Tract in Elderly Patients. JAMA otolaryngology-- head & neck surgery. 2018 Feb 1:144(2):140-148. doi: 10.1001/jamaoto.2017.2561. Epub
[PubMed PMID: 29270624]
[10]
Secretan B, Straif K, Baan R, Grosse Y, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V, WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens--Part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. The Lancet. Oncology. 2009 Nov:10(11):1033-4
[PubMed PMID: 19891056]
[11]
Combes JD, Franceschi S. Role of human papillomavirus in non-oropharyngeal head and neck cancers. Oral oncology. 2014 May:50(5):370-9. doi: 10.1016/j.oraloncology.2013.11.004. Epub 2013 Dec 9
[PubMed PMID: 24331868]
[12]
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018 Nov:68(6):394-424. doi: 10.3322/caac.21492. Epub 2018 Sep 12
[PubMed PMID: 30207593]
[13]
Shield KD, Ferlay J, Jemal A, Sankaranarayanan R, Chaturvedi AK, Bray F, Soerjomataram I. The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA: a cancer journal for clinicians. 2017 Jan:67(1):51-64. doi: 10.3322/caac.21384. Epub 2016 Oct 19
[PubMed PMID: 28076666]
[14]
Perdomo S, Martin Roa G, Brennan P, Forman D, Sierra MS. Head and neck cancer burden and preventive measures in Central and South America. Cancer epidemiology. 2016 Sep:44 Suppl 1():S43-S52. doi: 10.1016/j.canep.2016.03.012. Epub
[PubMed PMID: 27678322]
[15]
PDQ Adult Treatment Editorial Board. Hypopharyngeal Cancer Treatment (PDQ®): Health Professional Version. PDQ Cancer Information Summaries. 2002:():
[PubMed PMID: 26389199]
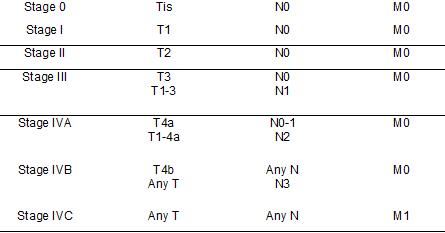
[16]
Pignon JP, Bourhis J, Domenge C, Designé L. Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC Collaborative Group. Meta-Analysis of Chemotherapy on Head and Neck Cancer. Lancet (London, England). 2000 Mar 18:355(9208):949-55
[PubMed PMID: 10768432]
Level 1 (high-level) evidence
[17]
Krstevska V. Early stage squamous cell carcinoma of the pyriform sinus: a review of treatment options. Indian journal of cancer. 2012 Apr-Jun:49(2):236-44. doi: 10.4103/0019-509X.102920. Epub
[PubMed PMID: 23107977]
[18]
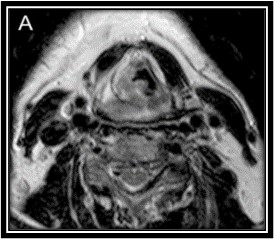
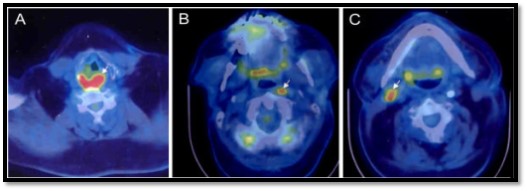
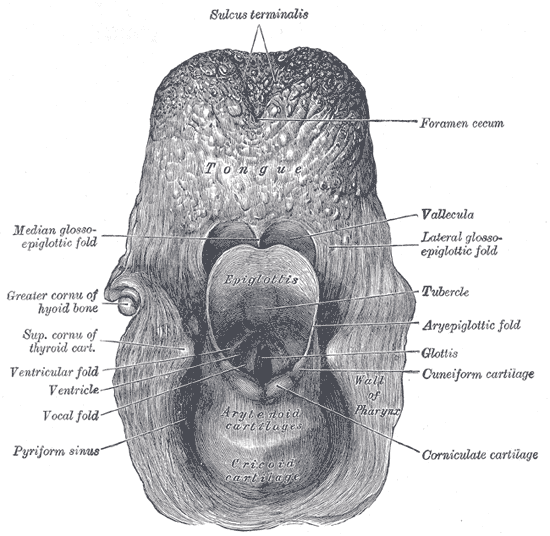
Wycliffe ND, Grover RS, Kim PD, Simental A Jr. Hypopharyngeal cancer. Topics in magnetic resonance imaging : TMRI. 2007 Aug:18(4):243-58
[PubMed PMID: 17893590]
[19]
Lefebvre JL, Castelain B, De la Torre JC, Delobelle-Deroide A, Vankemmel B. Lymph node invasion in hypopharynx and lateral epilarynx carcinoma: a prognostic factor. Head & neck surgery. 1987 Sep-Oct:10(1):14-8
[PubMed PMID: 3449476]
[20]
Garneau JC, Bakst RL, Miles BA. Hypopharyngeal cancer: A state of the art review. Oral oncology. 2018 Nov:86():244-250. doi: 10.1016/j.oraloncology.2018.09.025. Epub 2018 Oct 4
[PubMed PMID: 30409307]
[21]
Schmalfuss IM. Imaging of the hypopharynx and cervical esophagus. Magnetic resonance imaging clinics of North America. 2002 Aug:10(3):495-509, vi
[PubMed PMID: 12530231]
[22]
Adelstein D, Gillison ML, Pfister DG, Spencer S, Adkins D, Brizel DM, Burtness B, Busse PM, Caudell JJ, Cmelak AJ, Colevas AD, Eisele DW, Fenton M, Foote RL, Gilbert J, Haddad RI, Hicks WL, Hitchcock YJ, Jimeno A, Leizman D, Lydiatt WM, Maghami E, Mell LK, Mittal BB, Pinto HA, Ridge JA, Rocco J, Rodriguez CP, Shah JP, Weber RS, Witek M, Worden F, Yom SS, Zhen W, Burns JL, Darlow SD. NCCN Guidelines Insights: Head and Neck Cancers, Version 2.2017. Journal of the National Comprehensive Cancer Network : JNCCN. 2017 Jun:15(6):761-770. doi: 10.6004/jnccn.2017.0101. Epub
[PubMed PMID: 28596256]
[23]
Takes RP, Strojan P, Silver CE, Bradley PJ, Haigentz M Jr, Wolf GT, Shaha AR, Hartl DM, Olofsson J, Langendijk JA, Rinaldo A, Ferlito A, International Head and Neck Scientific Group. Current trends in initial management of hypopharyngeal cancer: the declining use of open surgery. Head & neck. 2012 Feb:34(2):270-81. doi: 10.1002/hed.21613. Epub 2010 Nov 10
[PubMed PMID: 22228621]
[24]
Posner M. Evolving strategies for combined-modality therapy for locally advanced head and neck cancer. The oncologist. 2007 Aug:12(8):967-74
[PubMed PMID: 17766656]
[25]
Lin H, Wang T, Heng Y, Zhu X, Zhou L, Zhang M, Shi Y, Cao P, Tao L. Risk stratification of postoperative recurrence in hypopharyngeal squamous-cell carcinoma patients with nodal metastasis. Journal of cancer research and clinical oncology. 2021 Mar:147(3):803-811. doi: 10.1007/s00432-020-03337-0. Epub 2020 Jul 29
[PubMed PMID: 32728810]
[26]
Forastiere AA, Ismaila N, Lewin JS, Nathan CA, Adelstein DJ, Eisbruch A, Fass G, Fisher SG, Laurie SA, Le QT, O'Malley B, Mendenhall WM, Patel S, Pfister DG, Provenzano AF, Weber R, Weinstein GS, Wolf GT. Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2018 Apr 10:36(11):1143-1169. doi: 10.1200/JCO.2017.75.7385. Epub 2017 Nov 27
[PubMed PMID: 29172863]
[27]
Lefebvre JL, Chevalier D, Luboinski B, Kirkpatrick A, Collette L, Sahmoud T. Larynx preservation in pyriform sinus cancer: preliminary results of a European Organization for Research and Treatment of Cancer phase III trial. EORTC Head and Neck Cancer Cooperative Group. Journal of the National Cancer Institute. 1996 Jul 3:88(13):890-9
[PubMed PMID: 8656441]
[28]
Holsinger FC, Motamed M, Garcia D, Brasnu D, Ménard M, Laccourreye O. Resection of selected invasive squamous cell carcinoma of the pyriform sinus by means of the lateral pharyngotomy approach: the partial lateral pharyngectomy. Head & neck. 2006 Aug:28(8):705-11
[PubMed PMID: 16786602]
[29]
Nouraei SA, Dias A, Kanona H, Vokes D, O'Flynn P, Clarke PM, Middleton SE, Darzi A, Aylin P, Jallali N. Impact of the method and success of pharyngeal reconstruction on the outcome of treating laryngeal and hypopharyngeal cancers with pharyngolaryngectomy: A national analysis. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2017 May:70(5):628-638. doi: 10.1016/j.bjps.2016.12.009. Epub 2017 Jan 9
[PubMed PMID: 28325565]
[30]
Steiner W, Ambrosch P, Hess CF, Kron M. Organ preservation by transoral laser microsurgery in piriform sinus carcinoma. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2001 Jan:124(1):58-67
[PubMed PMID: 11228455]
[31]
Casanueva R, López F, García-Cabo P, Álvarez-Marcos C, Llorente JL, Rodrigo JP. Oncological and functional outcomes of transoral laser surgery for hypopharyngeal carcinoma. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2023 Feb:280(2):829-837. doi: 10.1007/s00405-022-07622-1. Epub 2022 Sep 3
[PubMed PMID: 36056169]
[32]
Kuo CL, Lee TL, Chu PY. Conservation surgery for hypopharyngeal cancer: changing paradigm from open to endoscopic. Acta oto-laryngologica. 2013 Oct:133(10):1096-103. doi: 10.3109/00016489.2013.805341. Epub 2013 Jul 22
[PubMed PMID: 23869670]
[33]
Park YM, Kim WS, De Virgilio A, Lee SY, Seol JH, Kim SH. Transoral robotic surgery for hypopharyngeal squamous cell carcinoma: 3-year oncologic and functional analysis. Oral oncology. 2012 Jun:48(6):560-6. doi: 10.1016/j.oraloncology.2011.12.011. Epub 2012 Jan 20
[PubMed PMID: 22265334]
[34]
Shah JP. Patterns of cervical lymph node metastasis from squamous carcinomas of the upper aerodigestive tract. American journal of surgery. 1990 Oct:160(4):405-9
[PubMed PMID: 2221244]
[35]
Biau J, Lapeyre M, Troussier I, Budach W, Giralt J, Grau C, Kazmierska J, Langendijk JA, Ozsahin M, O'Sullivan B, Bourhis J, Grégoire V. Selection of lymph node target volumes for definitive head and neck radiation therapy: a 2019 Update. Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology. 2019 May:134():1-9. doi: 10.1016/j.radonc.2019.01.018. Epub 2019 Jan 30
[PubMed PMID: 31005201]
[36]
Johnson JT, Bacon GW, Myers EN, Wagner RL. Medial vs lateral wall pyriform sinus carcinoma: implications for management of regional lymphatics. Head & neck. 1994 Sep-Oct:16(5):401-5
[PubMed PMID: 7960736]
[37]
Bourhis J, Guigay J, Temam S, Pignon JP. Chemo-radiotherapy in head and neck cancer. Annals of oncology : official journal of the European Society for Medical Oncology. 2006 Sep:17 Suppl 10():x39-41
[PubMed PMID: 17018748]
[38]
Vermorken JB, Remenar E, van Herpen C, Gorlia T, Mesia R, Degardin M, Stewart JS, Jelic S, Betka J, Preiss JH, van den Weyngaert D, Awada A, Cupissol D, Kienzer HR, Rey A, Desaunois I, Bernier J, Lefebvre JL, EORTC 24971/TAX 323 Study Group. Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer. The New England journal of medicine. 2007 Oct 25:357(17):1695-704
[PubMed PMID: 17960012]
[39]
Cooke PV, Wu MP, Rathi VK, Chen S, Kappauf C, Roof SA, Lin DT, Deschler DG. Salvage surgery for recurrent or residual hypopharyngeal squamous cell carcinoma: A systematic review. Head & neck. 2024 Nov:46(11):2725-2736. doi: 10.1002/hed.27794. Epub 2024 May 8
[PubMed PMID: 38716810]
Level 1 (high-level) evidence
[40]
Harrington KJ, Burtness B, Greil R, Soulières D, Tahara M, de Castro G Jr, Psyrri A, Brana I, Basté N, Neupane P, Bratland Å, Fuereder T, Hughes BGM, Mesia R, Ngamphaiboon N, Rordorf T, Wan Ishak WZ, Lin J, Gumuscu B, Swaby RF, Rischin D. Pembrolizumab With or Without Chemotherapy in Recurrent or Metastatic Head and Neck Squamous Cell Carcinoma: Updated Results of the Phase III KEYNOTE-048 Study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2023 Feb 1:41(4):790-802. doi: 10.1200/JCO.21.02508. Epub 2022 Oct 11
[PubMed PMID: 36219809]
[41]
Oliveira G, Egloff AM, Afeyan AB, Wolff JO, Zeng Z, Chernock RD, Zhou L, Messier C, Lizotte P, Pfaff KL, Stromhaug K, Penter L, Haddad RI, Hanna GJ, Schoenfeld JD, Goguen LA, Annino DJ, Jo V, Oppelt P, Pipkorn P, Jackson R, Puram SV, Paniello RC, Rich JT, Webb J, Zevallos JP, Mansour M, Fu J, Dunn GP, Rodig SJ, Ley J, Morris LGT, Dunn L, Paweletz CP, Kallogjeri D, Piccirillo JF, Adkins DR, Wu CJ, Uppaluri R. Preexisting tumor-resident T cells with cytotoxic potential associate with response to neoadjuvant anti-PD-1 in head and neck cancer. Science immunology. 2023 Sep 8:8(87):eadf4968. doi: 10.1126/sciimmunol.adf4968. Epub 2023 Sep 8
[PubMed PMID: 37683037]
[42]
Fang Q, Li X, Xu P, Cao F, Wu D, Zhang X, Chen C, Gao J, Su Y, Liu X. PD-1 inhibitor combined with paclitaxel and cisplatin in the treatment of recurrent and metastatic hypopharyngeal/laryngeal squamous cell carcinoma: efficacy and survival outcomes. Frontiers in immunology. 2024:15():1353435. doi: 10.3389/fimmu.2024.1353435. Epub 2024 May 17
[PubMed PMID: 38827739]
[43]
Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G Jr, Psyrri A, Basté N, Neupane P, Bratland Å, Fuereder T, Hughes BGM, Mesía R, Ngamphaiboon N, Rordorf T, Wan Ishak WZ, Hong RL, González Mendoza R, Roy A, Zhang Y, Gumuscu B, Cheng JD, Jin F, Rischin D, KEYNOTE-048 Investigators. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet (London, England). 2019 Nov 23:394(10212):1915-1928. doi: 10.1016/S0140-6736(19)32591-7. Epub 2019 Nov 1
[PubMed PMID: 31679945]
Level 1 (high-level) evidence
[44]
Konuthula N, Do OA, Gobillot T, Rodriguez CP, Futran ND, Houlton J, Barber BR. Oncologic outcomes of salvage surgery and immune checkpoint inhibitor therapy in recurrent head and neck squamous cell carcinoma: A single-institution retrospective study. Head & neck. 2022 Nov:44(11):2465-2472. doi: 10.1002/hed.27162. Epub 2022 Aug 5
[PubMed PMID: 35930296]
Level 2 (mid-level) evidence
[45]
Fang Q, Xu P, Cao F, Wu D, Liu X. PD-1 Inhibitors combined with paclitaxel (Albumin-bound) and cisplatin for larynx preservation in locally advanced laryngeal and hypopharyngeal squamous cell carcinoma: a retrospective study. Cancer immunology, immunotherapy : CII. 2023 Dec:72(12):4161-4168. doi: 10.1007/s00262-023-03550-z. Epub 2023 Oct 7
[PubMed PMID: 37804437]
Level 2 (mid-level) evidence
[46]
Zanoni DK, Patel SG, Shah JP. Changes in the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging of Head and Neck Cancer: Rationale and Implications. Current oncology reports. 2019 Apr 17:21(6):52. doi: 10.1007/s11912-019-0799-x. Epub 2019 Apr 17
[PubMed PMID: 30997577]
[47]
Martin SA, Marks JE, Lee JY, Bauer WC, Ogura JH. Carcinoma of the pyriform sinus: predictors of TNM relapse and survival. Cancer. 1980 Nov 1:46(9):1974-81
[PubMed PMID: 7427903]
[48]
Gang G, Xinwei C, LiXiao C, Yu Z, Cheng Z, Pin D. Risk factors of lymphovascular invasion in hypopharyngeal squamous cell carcinoma and its influence on prognosis. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2022 Mar:279(3):1473-1479. doi: 10.1007/s00405-021-06906-2. Epub 2021 Jun 2
[PubMed PMID: 34076727]
[49]
Siddiqui F, Movsas B. Management of Radiation Toxicity in Head and Neck Cancers. Seminars in radiation oncology. 2017 Oct:27(4):340-349. doi: 10.1016/j.semradonc.2017.04.008. Epub
[PubMed PMID: 28865517]
[50]
Iglesias Docampo LC, Arrazubi Arrula V, Baste Rotllan N, Carral Maseda A, Cirauqui Cirauqui B, Escobar Y, Lambea Sorrosal JJ, Pastor Borgoñón M, Rueda A, Cruz Hernández JJ. SEOM clinical guidelines for the treatment of head and neck cancer (2017). Clinical & translational oncology : official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico. 2018 Jan:20(1):75-83. doi: 10.1007/s12094-017-1776-1. Epub 2017 Nov 20
[PubMed PMID: 29159792]
[51]
Lechner M, Breeze CE, Vaz F, Lund VJ, Kotecha B. Betel nut chewing in high-income countries-lack of awareness and regulation. The Lancet. Oncology. 2019 Feb:20(2):181-183. doi: 10.1016/S1470-2045(18)30911-2. Epub
[PubMed PMID: 30723038]
[52]
Petersen PE. Oral cancer prevention and control--the approach of the World Health Organization. Oral oncology. 2009 Apr-May:45(4-5):454-60. doi: 10.1016/j.oraloncology.2008.05.023. Epub 2008 Sep 18
[PubMed PMID: 18804412]