[1]
Clemens JQ, Erickson DR, Varela NP, Lai HH. Diagnosis and Treatment of Interstitial Cystitis/Bladder Pain Syndrome. The Journal of urology. 2022 Jul:208(1):34-42. doi: 10.1097/JU.0000000000002756. Epub 2022 May 10
[PubMed PMID: 35536143]
[2]
Hanno P, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourology and urodynamics. 2009:28(4):274-86. doi: 10.1002/nau.20687. Epub
[PubMed PMID: 19260081]
Level 3 (low-level) evidence
[3]
Berger RE, Miller JE, Rothman I, Krieger JN, Muller CH. Bladder petechiae after cystoscopy and hydrodistension in men diagnosed with prostate pain. The Journal of urology. 1998 Jan:159(1):83-5
[PubMed PMID: 9400442]
[4]
Forrest JB, Schmidt S. Interstitial cystitis, chronic nonbacterial prostatitis and chronic pelvic pain syndrome in men: a common and frequently identical clinical entity. The Journal of urology. 2004 Dec:172(6 Pt 2):2561-2
[PubMed PMID: 15538208]
[5]
Forrest JB, Vo Q. Observations on the presentation, diagnosis, and treatment of interstitial cystitis in men. Urology. 2001 Jun:57(6 Suppl 1):26-9
[PubMed PMID: 11378046]
[6]
Clemens JQ, Clauw DJ, Kreder K, Krieger JN, Kusek JW, Lai HH, Rodriguez L, Williams DA, Hou X, Stephens A, Landis JR, MAPP Research Network. Comparison of baseline urological symptoms in men and women in the MAPP research cohort. The Journal of urology. 2015 May:193(5):1554-8. doi: 10.1016/j.juro.2014.11.016. Epub 2014 Nov 13
[PubMed PMID: 25463989]
[7]
Arora HC, Shoskes DA. The enigma of men with interstitial cystitis/bladder pain syndrome. Translational andrology and urology. 2015 Dec:4(6):668-76. doi: 10.3978/j.issn.2223-4683.2015.10.01. Epub
[PubMed PMID: 26813678]
[8]
Bogart LM, Berry SH, Clemens JQ. Symptoms of interstitial cystitis, painful bladder syndrome and similar diseases in women: a systematic review. The Journal of urology. 2007 Feb:177(2):450-6
[PubMed PMID: 17222607]
Level 1 (high-level) evidence
[10]
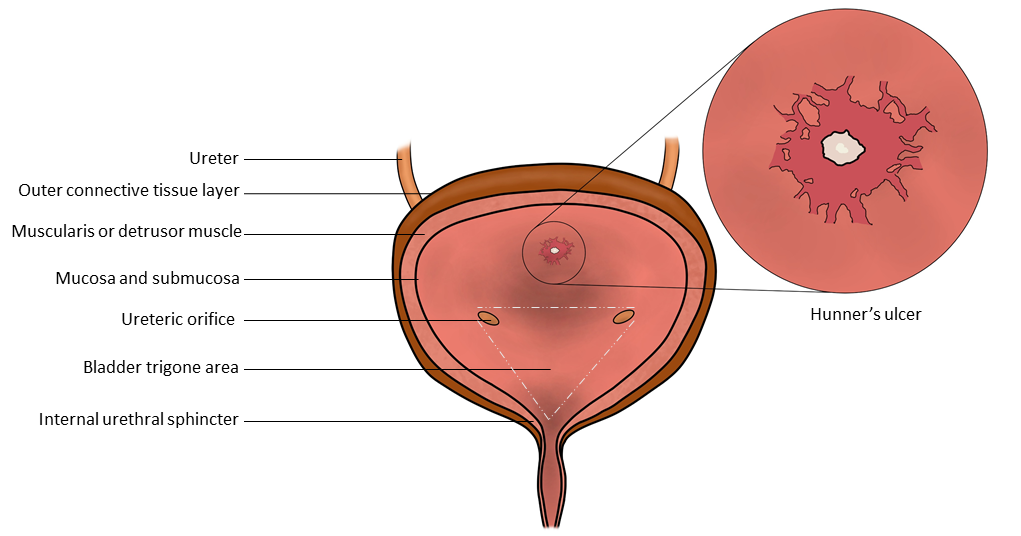
Sam P, Jiang J, Leslie SW, LaGrange CA. Anatomy, Abdomen and Pelvis, Sphincter Urethrae. StatPearls. 2024 Jan:():
[PubMed PMID: 29494045]
[11]
Sam P, Nassereddin A, LaGrange CA. Anatomy, Abdomen and Pelvis: Bladder Detrusor Muscle. StatPearls. 2024 Jan:():
[PubMed PMID: 29489195]
[13]
Jhang JF, Jiang YH, Kuo HC. Current Understanding of the Pathophysiology and Novel Treatments of Interstitial Cystitis/Bladder Pain Syndrome. Biomedicines. 2022 Sep 23:10(10):. doi: 10.3390/biomedicines10102380. Epub 2022 Sep 23
[PubMed PMID: 36289642]
Level 3 (low-level) evidence
[14]
Shie JH, Kuo HC. Higher levels of cell apoptosis and abnormal E-cadherin expression in the urothelium are associated with inflammation in patients with interstitial cystitis/painful bladder syndrome. BJU international. 2011 Jul:108(2 Pt 2):E136-41. doi: 10.1111/j.1464-410X.2010.09911.x. Epub 2010 Dec 16
[PubMed PMID: 21166752]
[15]
Jiang YH, Peng CH, Liu HT, Kuo HC. Increased pro-inflammatory cytokines, C-reactive protein and nerve growth factor expressions in serum of patients with interstitial cystitis/bladder pain syndrome. PloS one. 2013:8(10):e76779. doi: 10.1371/journal.pone.0076779. Epub 2013 Oct 17
[PubMed PMID: 24146927]
[16]
Tyagi P, Moon CH, Janicki J, Kaufman J, Chancellor M, Yoshimura N, Chermansky C. Recent advances in imaging and understanding interstitial cystitis. F1000Research. 2018:7():. pii: F1000 Faculty Rev-1771. doi: 10.12688/f1000research.16096.1. Epub 2018 Nov 9
[PubMed PMID: 30473772]
Level 3 (low-level) evidence
[17]
Kairys AE, Schmidt-Wilcke T, Puiu T, Ichesco E, Labus JS, Martucci K, Farmer MA, Ness TJ, Deutsch G, Mayer EA, Mackey S, Apkarian AV, Maravilla K, Clauw DJ, Harris RE. Increased brain gray matter in the primary somatosensory cortex is associated with increased pain and mood disturbance in patients with interstitial cystitis/painful bladder syndrome. The Journal of urology. 2015 Jan:193(1):131-7. doi: 10.1016/j.juro.2014.08.042. Epub 2014 Aug 14
[PubMed PMID: 25132239]
[18]
Kilpatrick LA, Kutch JJ, Tillisch K, Naliboff BD, Labus JS, Jiang Z, Farmer MA, Apkarian AV, Mackey S, Martucci KT, Clauw DJ, Harris RE, Deutsch G, Ness TJ, Yang CC, Maravilla K, Mullins C, Mayer EA. Alterations in resting state oscillations and connectivity in sensory and motor networks in women with interstitial cystitis/painful bladder syndrome. The Journal of urology. 2014 Sep:192(3):947-55. doi: 10.1016/j.juro.2014.03.093. Epub 2014 Mar 26
[PubMed PMID: 24681331]
[19]
Misra S, Chetwood A, Coker C, Thomas P. Ketamine cystitis: practical considerations in management. Scandinavian journal of urology. 2014 Oct:48(5):482-8. doi: 10.3109/21681805.2014.909530. Epub 2014 Apr 30
[PubMed PMID: 24779452]
[20]
Argade S, Chermansky C, Tyagi P. Biomarkers for interstitial cystitis/painful bladder syndrome. Women's health (London, England). 2016 Jan:12(1):87-90. doi: 10.2217/whe.15.93. Epub 2015 Dec 23
[PubMed PMID: 26696241]
[21]
Dinis S, de Oliveira JT, Pinto R, Cruz F, Buffington CT, Dinis P. From bladder to systemic syndrome: concept and treatment evolution of interstitial cystitis. International journal of women's health. 2015:7():735-44. doi: 10.2147/IJWH.S60798. Epub 2015 Jul 23
[PubMed PMID: 26229509]
[22]
Gamper M, Regauer S, Welter J, Eberhard J, Viereck V. Are mast cells still good biomarkers for bladder pain syndrome/interstitial cystitis? The Journal of urology. 2015 Jun:193(6):1994-2000. doi: 10.1016/j.juro.2015.01.036. Epub 2015 Jan 14
[PubMed PMID: 25596361]
[23]
Ackerman AL, Lee UJ, Jellison FC, Tan N, Patel M, Raman SS, Rodriguez LV. MRI suggests increased tonicity of the levator ani in women with interstitial cystitis/bladder pain syndrome. International urogynecology journal. 2016 Jan:27(1):77-83. doi: 10.1007/s00192-015-2794-6. Epub 2015 Aug 1
[PubMed PMID: 26231233]
[24]
Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, Nyberg L, Clemens JQ. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. The Journal of urology. 2011 Aug:186(2):540-4. doi: 10.1016/j.juro.2011.03.132. Epub 2011 Jun 16
[PubMed PMID: 21683389]
[25]
Suskind AM, Berry SH, Ewing BA, Elliott MN, Suttorp MJ, Clemens JQ. The prevalence and overlap of interstitial cystitis/bladder pain syndrome and chronic prostatitis/chronic pelvic pain syndrome in men: results of the RAND Interstitial Cystitis Epidemiology male study. The Journal of urology. 2013 Jan:189(1):141-5. doi: 10.1016/j.juro.2012.08.088. Epub 2012 Nov 16
[PubMed PMID: 23164386]
[26]
Curhan GC, Speizer FE, Hunter DJ, Curhan SG, Stampfer MJ. Epidemiology of interstitial cystitis: a population based study. The Journal of urology. 1999 Feb:161(2):549-52
[PubMed PMID: 9915446]
[27]
Konkle KS, Berry SH, Elliott MN, Hilton L, Suttorp MJ, Clauw DJ, Clemens JQ. Comparison of an interstitial cystitis/bladder pain syndrome clinical cohort with symptomatic community women from the RAND Interstitial Cystitis Epidemiology study. The Journal of urology. 2012 Feb:187(2):508-12. doi: 10.1016/j.juro.2011.10.040. Epub 2011 Dec 15
[PubMed PMID: 22177158]
[28]
Clemens JQ, Meenan RT, O'Keeffe Rosetti MC, Brown SO, Gao SY, Calhoun EA. Prevalence of interstitial cystitis symptoms in a managed care population. The Journal of urology. 2005 Aug:174(2):576-80
[PubMed PMID: 16006901]
[29]
Bade JJ, Rijcken B, Mensink HJ. Interstitial cystitis in The Netherlands: prevalence, diagnostic criteria and therapeutic preferences. The Journal of urology. 1995 Dec:154(6):2035-7; discussion 2037-8
[PubMed PMID: 7500452]
[30]
Chung KJ, Han AN, Kim KH. Recommendations to the primary care practitioners and the patients for managing pelvic pain, especially in painful bladder syndrome for early and better prognosis. Journal of exercise rehabilitation. 2015 Oct:11(5):251-4. doi: 10.12965/jer.150226. Epub 2015 Oct 30
[PubMed PMID: 26535214]
[31]
Jiang YH, Jhang JF, Kuo HC. The clinical application of intravesical botulinum toxin A injection in patients with overactive bladder and interstitial cystitis. Tzu chi medical journal. 2023 Jan-Mar:35(1):31-37. doi: 10.4103/tcmj.tcmj_313_21. Epub 2022 Mar 11
[PubMed PMID: 36866354]
[32]
Lopez SR, Mangır N. Current standard of care in treatment of bladder pain syndrome/interstitial cystitis. Therapeutic advances in urology. 2021 Jan-Dec:13():17562872211022478. doi: 10.1177/17562872211022478. Epub 2021 Jun 12
[PubMed PMID: 34178118]
Level 3 (low-level) evidence
[33]
Johansson SL, Fall M. Clinical features and spectrum of light microscopic changes in interstitial cystitis. The Journal of urology. 1990 Jun:143(6):1118-24
[PubMed PMID: 2342171]
[34]
Shie JH, Liu HT, Kuo HC. Increased cell apoptosis of urothelium mediated by inflammation in interstitial cystitis/painful bladder syndrome. Urology. 2012 Feb:79(2):484.e7-13. doi: 10.1016/j.urology.2011.09.049. Epub
[PubMed PMID: 22310775]
[35]
Jiang YH, Jhang JF, Hsu YH, Kuo HC. Usefulness of Urinary Biomarkers for Assessing Bladder Condition and Histopathology in Patients with Interstitial Cystitis/Bladder Pain Syndrome. International journal of molecular sciences. 2022 Oct 10:23(19):. doi: 10.3390/ijms231912044. Epub 2022 Oct 10
[PubMed PMID: 36233356]
[36]
Birder LA. Pathophysiology of interstitial cystitis. International journal of urology : official journal of the Japanese Urological Association. 2019 Jun:26 Suppl 1():12-15. doi: 10.1111/iju.13985. Epub
[PubMed PMID: 31144735]
[37]
Wen JY, Lo TS, Chuang YC, Ho CH, Long CY, Law KS, Tong YC, Wu MP. Risks of interstitial cystitis among patients with systemic lupus erythematosus: A population-based cohort study. International journal of urology : official journal of the Japanese Urological Association. 2019 Sep:26(9):897-902. doi: 10.1111/iju.14065. Epub 2019 Jul 16
[PubMed PMID: 31311067]
[38]
Yueh HZ, Yang MH, Huang JY, Wei JC. Risk of Autoimmune Diseases in Patients With Interstitial Cystitis/Bladder Pain Syndrome: A Nationwide Population-Based Study in Taiwan. Frontiers in medicine. 2021:8():747098. doi: 10.3389/fmed.2021.747098. Epub 2021 Sep 20
[PubMed PMID: 34616760]
[39]
Darrieutort-Laffite C, André V, Hayem G, Saraux A, Le Guern V, Le Jeunne C, Puéchal X. Sjögren's syndrome complicated by interstitial cystitis: A case series and literature review. Joint bone spine. 2015 Jul:82(4):245-50. doi: 10.1016/j.jbspin.2014.12.007. Epub 2015 Feb 10
[PubMed PMID: 25680227]
Level 2 (mid-level) evidence
[40]
Nickel JC, Tripp DA, Pontari M, Moldwin R, Mayer R, Carr LK, Doggweiler R, Yang CC, Mishra N, Nordling J. Interstitial cystitis/painful bladder syndrome and associated medical conditions with an emphasis on irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome. The Journal of urology. 2010 Oct:184(4):1358-63. doi: 10.1016/j.juro.2010.06.005. Epub 2010 Aug 17
[PubMed PMID: 20719340]
[41]
Pereira E Silva R, Romão VC, Neves M, Garcia R, Oliveira S, Brites J, Ramos FO, Canhão H, Palma Dos Reis J, Pereira da Silva JA, Lopes T. Overactive bladder symptom bother and health-related quality of life in patients with systemic lupus erythematosus and primary Sjögren syndrome. Lupus. 2019 Jan:28(1):27-33. doi: 10.1177/0961203318811605. Epub 2018 Nov 12
[PubMed PMID: 30419773]
Level 2 (mid-level) evidence
[42]
Kanter G, Komesu YM, Qaedan F, Jeppson PC, Dunivan GC, Cichowski SB, Rogers RG. Mindfulness-based stress reduction as a novel treatment for interstitial cystitis/bladder pain syndrome: a randomized controlled trial. International urogynecology journal. 2016 Nov:27(11):1705-1711
[PubMed PMID: 27116196]
Level 1 (high-level) evidence
[43]
Ho NJ, Koziol JA, Parsons CL, Barlow W, Weiss NS. Natural history of interstitial cystitis in 274 patients receiving sulfated polysaccharide therapy. Urology. 1999 Jun:53(6):1133-9
[PubMed PMID: 10367841]
[44]
Lutgendorf SK, Kreder KJ, Rothrock NE, Ratliff TL, Zimmerman B. Stress and symptomatology in patients with interstitial cystitis: a laboratory stress model. The Journal of urology. 2000 Oct:164(4):1265-9
[PubMed PMID: 10992377]
[45]
Pierce AN, Christianson JA. Stress and chronic pelvic pain. Progress in molecular biology and translational science. 2015:131():509-35. doi: 10.1016/bs.pmbts.2014.11.009. Epub 2015 Feb 2
[PubMed PMID: 25744684]
[46]
Lovick TA. Central control of visceral pain and urinary tract function. Autonomic neuroscience : basic & clinical. 2016 Oct:200():35-42. doi: 10.1016/j.autneu.2016.02.001. Epub 2016 Feb 6
[PubMed PMID: 26905459]
[47]
Dupont MC, Spitsbergen JM, Kim KB, Tuttle JB, Steers WD. Histological and neurotrophic changes triggered by varying models of bladder inflammation. The Journal of urology. 2001 Sep:166(3):1111-8
[PubMed PMID: 11490308]
[48]
Lynes WL, Flynn SD, Shortliffe LD, Stamey TA. The histology of interstitial cystitis. The American journal of surgical pathology. 1990 Oct:14(10):969-76
[PubMed PMID: 2403198]
[49]
Jhang JF, Hsu YH, Jiang YH, Ho HC, Kuo HC. Clinical Relevance of Bladder Histopathological Findings and Their Impact on Treatment Outcomes among Patients with Interstitial Cystitis/Bladder Pain Syndrome: An Investigation of the European Society for the Study of Interstitial Cystitis Histopathological Classification. The Journal of urology. 2021 Jan:205(1):226-235. doi: 10.1097/JU.0000000000001334. Epub 2020 Aug 28
[PubMed PMID: 32856961]
[50]
Kim HJ. Update on the Pathology and Diagnosis of Interstitial Cystitis/Bladder Pain Syndrome: A Review. International neurourology journal. 2016 Mar:20(1):13-7. doi: 10.5213/inj.1632522.261. Epub 2016 Mar 23
[PubMed PMID: 27032552]
[51]
Natale F, Campagna G, Marturano M, Caramazza D, Panico G, Vacca L, Torcia E, Cervigni M, Scambia G, Ercoli A. Is There a Role for Bladder Biopsy in the Diagnosis of Non-Hunner Lesions Interstitial Cystitis? Urologia internationalis. 2023:107(3):257-262. doi: 10.1159/000525849. Epub 2022 Jul 27
[PubMed PMID: 35896088]
[52]
Diggs C, Meyer WA, Langenberg P, Greenberg P, Horne L, Warren JW. Assessing urgency in interstitial cystitis/painful bladder syndrome. Urology. 2007 Feb:69(2):210-4
[PubMed PMID: 17275075]
[53]
Clemens JQ, Calhoun EA, Litwin MS, McNaughton-Collins M, Kusek JW, Crowley EM, Landis JR, Urologic Pelvic Pain Collaborative Research Network. Validation of a modified National Institutes of Health chronic prostatitis symptom index to assess genitourinary pain in both men and women. Urology. 2009 Nov:74(5):983-7, quiz 987.e1-3. doi: 10.1016/j.urology.2009.06.078. Epub 2009 Oct 2
[PubMed PMID: 19800663]
Level 1 (high-level) evidence
[55]
Siltberg H, Larsson G, Victor A. Frequency/volume chart: the basic tool for investigating urinary symptoms. Acta obstetricia et gynecologica Scandinavica. Supplement. 1997:166():24-7
[PubMed PMID: 9253374]
[56]
Abrams P, Klevmark B. Frequency volume charts: an indispensable part of lower urinary tract assessment. Scandinavian journal of urology and nephrology. Supplementum. 1996:179():47-53
[PubMed PMID: 8908664]
[57]
Clemens JQ, Brown SO, Calhoun EA. Mental health diagnoses in patients with interstitial cystitis/painful bladder syndrome and chronic prostatitis/chronic pelvic pain syndrome: a case/control study. The Journal of urology. 2008 Oct:180(4):1378-82. doi: 10.1016/j.juro.2008.06.032. Epub 2008 Aug 15
[PubMed PMID: 18707716]
Level 3 (low-level) evidence
[58]
Barocas DA, Boorjian SA, Alvarez RD, Downs TM, Gross CP, Hamilton BD, Kobashi KC, Lipman RR, Lotan Y, Ng CK, Nielsen ME, Peterson AC, Raman JD, Smith-Bindman R, Souter LH. Microhematuria: AUA/SUFU Guideline. The Journal of urology. 2020 Oct:204(4):778-786. doi: 10.1097/JU.0000000000001297. Epub 2020 Jul 23
[PubMed PMID: 32698717]
[59]
Erickson DR, Kunselman AR, Bentley CM, Peters KM, Rovner ES, Demers LM, Wheeler MA, Keay SK. Changes in urine markers and symptoms after bladder distention for interstitial cystitis. The Journal of urology. 2007 Feb:177(2):556-60
[PubMed PMID: 17222633]
[61]
Forrest JB, Nickel JC, Moldwin RM. Chronic prostatitis/chronic pelvic pain syndrome and male interstitial cystitis: enigmas and opportunities. Urology. 2007 Apr:69(4 Suppl):60-3
[PubMed PMID: 17462482]
[63]
Parsons CL, Zupkas P, Parsons JK. Intravesical potassium sensitivity in patients with interstitial cystitis and urethral syndrome. Urology. 2001 Mar:57(3):428-32; discussion 432-3
[PubMed PMID: 11248610]
[65]
Watanabe D, Akiyama Y, Niimi A, Nomiya A, Yamada Y, Sato Y, Nakamura M, Kawai T, Yamada D, Suzuki M, Igawa Y, Kume H, Homma Y. Clinical characterization of interstitial cystitis/bladder pain syndrome in women based on the presence or absence of Hunner lesions and glomerulations. Lower urinary tract symptoms. 2021 Jan:13(1):139-143. doi: 10.1111/luts.12344. Epub 2020 Aug 23
[PubMed PMID: 32830459]
[66]
Chen YC, Jiang YH, Jhang JF, Kuo HC. Using Urine Biomarkers to Differentiate Bladder Dysfunctions in Women with Sensory Bladder Disorders. International journal of molecular sciences. 2024 Aug 29:25(17):. doi: 10.3390/ijms25179359. Epub 2024 Aug 29
[PubMed PMID: 39273307]
[67]
Gross J, Vetter J, Lai HH. Clinical Presentation of Urologic Chronic Pelvic Pain Syndrome (UCPPS) Varies With Presenting Age - Implication on Patient Evaluation. Urology. 2021 Dec:158():66-73. doi: 10.1016/j.urology.2021.07.007. Epub 2021 Jul 22
[PubMed PMID: 34302833]
[68]
Wennevik GE, Meijlink JM, Hanno P, Nordling J. The Role of Glomerulations in Bladder Pain Syndrome: A Review. The Journal of urology. 2016 Jan:195(1):19-25. doi: 10.1016/j.juro.2015.06.112. Epub 2015 Aug 28
[PubMed PMID: 26318984]
[69]
Ronstrom C, Lai HH. Presenting an atlas of Hunner lesions in interstitial cystitis which can be identified with office cystoscopy. Neurourology and urodynamics. 2020 Nov:39(8):2394-2400. doi: 10.1002/nau.24500. Epub 2020 Sep 9
[PubMed PMID: 32902893]
[70]
Ko KJ, Cho WJ, Lee YS, Choi J, Byun HJ, Lee KS. Comparison of the Efficacy Between Transurethral Coagulation and Transurethral Resection of Hunner Lesion in Interstitial Cystitis/Bladder Pain Syndrome Patients: A Prospective Randomized Controlled Trial. European urology. 2020 May:77(5):644-651. doi: 10.1016/j.eururo.2020.01.002. Epub 2020 Jan 17
[PubMed PMID: 31959549]
Level 1 (high-level) evidence
[71]
Peeker R, Aldenborg F, Fall M. Complete transurethral resection of ulcers in classic interstitial cystitis. International urogynecology journal and pelvic floor dysfunction. 2000:11(5):290-5
[PubMed PMID: 11052564]
[72]
Sairanen J, Tammela TL, Leppilahti M, Multanen M, Paananen I, Lehtoranta K, Ruutu M. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. The Journal of urology. 2005 Dec:174(6):2235-8
[PubMed PMID: 16280777]
Level 2 (mid-level) evidence
[73]
Tissot WD, Diokno AC, Peters KM. A referral center's experience with transitional cell carcinoma misdiagnosed as interstitial cystitis. The Journal of urology. 2004 Aug:172(2):478-80
[PubMed PMID: 15247708]
[74]
Chen Y, Ying Z, Xiao Y, Liu Y, Wu S. The diagnostic and therapeutic efficacy of cystoscopy with hydrodistension and random biopsies in clinically suspected interstitial cystitis/bladder pain syndrome. European journal of obstetrics, gynecology, and reproductive biology. 2021 Oct:265():156-161. doi: 10.1016/j.ejogrb.2021.08.025. Epub 2021 Aug 27
[PubMed PMID: 34492610]
[75]
Sholan R. Clinical manifestations and results of cystoscopy in women with interstitial cystitis/bladder pain syndrome. Northern clinics of Istanbul. 2020:7(5):417-424. doi: 10.14744/nci.2020.23245. Epub 2020 Aug 18
[PubMed PMID: 33163875]
[76]
Grover S, Srivastava A, Lee R, Tewari AK, Te AE. Role of inflammation in bladder function and interstitial cystitis. Therapeutic advances in urology. 2011 Feb:3(1):19-33. doi: 10.1177/1756287211398255. Epub
[PubMed PMID: 21789096]
Level 3 (low-level) evidence
[77]
FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, Nickel JC, Hanno PM, Kreder KJ, Burks DA, Mayer R, Kotarinos R, Fortman C, Allen TM, Fraser L, Mason-Cover M, Furey C, Odabachian L, Sanfield A, Chu J, Huestis K, Tata GE, Dugan N, Sheth H, Bewyer K, Anaeme A, Newton K, Featherstone W, Halle-Podell R, Cen L, Landis JR, Propert KJ, Foster HE Jr, Kusek JW, Nyberg LM, Interstitial Cystitis Collaborative Research Network. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. The Journal of urology. 2012 Jun:187(6):2113-8. doi: 10.1016/j.juro.2012.01.123. Epub 2012 Apr 12
[PubMed PMID: 22503015]
Level 1 (high-level) evidence
[78]
Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. The Journal of urology. 2001 Dec:166(6):2226-31
[PubMed PMID: 11696740]
[79]
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016 Apr 19:315(15):1624-45. doi: 10.1001/jama.2016.1464. Epub
[PubMed PMID: 26977696]
[80]
Santos TGD, Miranda IAS, Nygaard CC, Schreiner L, Castro RA, Haddad JM. Systematic Review of Oral Therapy for the Treatment of Symptoms of Bladder Pain Syndrome: The Brazilian Guidelines. Revista brasileira de ginecologia e obstetricia : revista da Federacao Brasileira das Sociedades de Ginecologia e Obstetricia. 2018 Feb:40(2):96-102. doi: 10.1055/s-0037-1609049. Epub 2017 Dec 14
[PubMed PMID: 29241263]
Level 1 (high-level) evidence
[81]
Vollstedt A, Tennyson L, Turner K, Hasenau D, Saon M, McCartney T, Beck D, Gilleran J, Peters K. Evidence for Early Cyclosporine Treatment for Hunner Lesion Interstitial Cystitis. Female pelvic medicine & reconstructive surgery. 2022 Jan 1:28(1):e1-e5. doi: 10.1097/SPV.0000000000001108. Epub
[PubMed PMID: 34608034]
[82]
Chermansky CJ, Guirguis MO. Pharmacologic Management of Interstitial Cystitis/Bladder Pain Syndrome. The Urologic clinics of North America. 2022 May:49(2):273-282. doi: 10.1016/j.ucl.2022.01.003. Epub
[PubMed PMID: 35428433]
[84]
van Ophoven A, Pokupic S, Heinecke A, Hertle L. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. The Journal of urology. 2004 Aug:172(2):533-6
[PubMed PMID: 15247722]
Level 1 (high-level) evidence
[85]
Foster HE Jr, Hanno PM, Nickel JC, Payne CK, Mayer RD, Burks DA, Yang CC, Chai TC, Kreder KJ, Peters KM, Lukacz ES, FitzGerald MP, Cen L, Landis JR, Propert KJ, Yang W, Kusek JW, Nyberg LM, Interstitial Cystitis Collaborative Research Network. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. The Journal of urology. 2010 May:183(5):1853-8. doi: 10.1016/j.juro.2009.12.106. Epub 2010 Mar 29
[PubMed PMID: 20303115]
[86]
Abat D, Altunkol A, Gökalp F. The effect of intravesical cocktail therapy combined with low-dose amitriptyline on primary bladder pain syndrome. International urogynecology journal. 2022 May:33(5):1225-1230. doi: 10.1007/s00192-021-05043-y. Epub 2022 Jan 3
[PubMed PMID: 34977954]
[87]
Dasgupta P, Sharma SD, Womack C, Blackford HN, Dennis P. Cimetidine in painful bladder syndrome: a histopathological study. BJU international. 2001 Aug:88(3):183-6
[PubMed PMID: 11488726]
[89]
Thilagarajah R, Witherow RO, Walker MM. Oral cimetidine gives effective symptom relief in painful bladder disease: a prospective, randomized, double-blind placebo-controlled trial. BJU international. 2001 Feb:87(3):207-12
[PubMed PMID: 11167643]
Level 1 (high-level) evidence
[91]
Forrest JB, Payne CK, Erickson DR. Cyclosporine A for refractory interstitial cystitis/bladder pain syndrome: experience of 3 tertiary centers. The Journal of urology. 2012 Oct:188(4):1186-91. doi: 10.1016/j.juro.2012.06.023. Epub 2012 Aug 15
[PubMed PMID: 22901569]
[92]
Di XP, Luo DY, Jin X, Zhao WY, Li H, Wang KJ. Efficacy and safety comparison of pharmacotherapies for interstitial cystitis and bladder pain syndrome: a systematic review and Bayesian network meta-analysis. International urogynecology journal. 2021 May:32(5):1129-1141. doi: 10.1007/s00192-020-04659-w. Epub 2021 Feb 27
[PubMed PMID: 33638677]
Level 1 (high-level) evidence
[94]
Brière R, Bouchard F, Ismail S, Gareau Labelle AK, Tu LM. A pilot study on oral cyclosporine A in association with fulguration for the treatment of interstitial cystitis with Hunner's lesions. Neurourology and urodynamics. 2022 Aug:41(6):1498-1504. doi: 10.1002/nau.24997. Epub 2022 Jun 22
[PubMed PMID: 35731015]
Level 3 (low-level) evidence
[95]
Speer LM, Mushkbar S, Erbele T. Chronic Pelvic Pain in Women. American family physician. 2016 Mar 1:93(5):380-7
[PubMed PMID: 26926975]
[96]
Hansen HC. Interstitial cystitis and the potential role of gabapentin. Southern medical journal. 2000 Feb:93(2):238-42
[PubMed PMID: 10701800]
[97]
Sasaki K, Smith CP, Chuang YC, Lee JY, Kim JC, Chancellor MB. Oral gabapentin (neurontin) treatment of refractory genitourinary tract pain. Techniques in urology. 2001 Mar:7(1):47-9
[PubMed PMID: 11272678]
[98]
Kim YT, Kwon DD, Kim J, Kim DK, Lee JY, Chancellor MB. Gabapentin for overactive bladder and nocturia after anticholinergic failure. International braz j urol : official journal of the Brazilian Society of Urology. 2004 Jul-Aug:30(4):275-8
[PubMed PMID: 15679954]
[100]
Sant GR, Propert KJ, Hanno PM, Burks D, Culkin D, Diokno AC, Hardy C, Landis JR, Mayer R, Madigan R, Messing EM, Peters K, Theoharides TC, Warren J, Wein AJ, Steers W, Kusek JW, Nyberg LM, Interstitial Cystitis Clinical Trials Group. A pilot clinical trial of oral pentosan polysulfate and oral hydroxyzine in patients with interstitial cystitis. The Journal of urology. 2003 Sep:170(3):810-5
[PubMed PMID: 12913705]
Level 3 (low-level) evidence
[101]
Minogiannis P, El-Mansoury M, Betances JA, Sant GR, Theoharides TC. Hydroxyzine inhibits neurogenic bladder mast cell activation. International journal of immunopharmacology. 1998 Oct:20(10):553-63
[PubMed PMID: 9839659]
[102]
Dobberfuhl AD. Pathophysiology, assessment, and treatment of overactive bladder symptoms in patients with interstitial cystitis/bladder pain syndrome. Neurourology and urodynamics. 2022 Nov:41(8):1958-1966. doi: 10.1002/nau.24958. Epub 2022 May 24
[PubMed PMID: 35607890]
[103]
Loloi J, Clearwater W, Schulz A, Suadicani SO, Abraham N. Medical Treatment of Overactive Bladder. The Urologic clinics of North America. 2022 May:49(2):249-261. doi: 10.1016/j.ucl.2021.12.005. Epub
[PubMed PMID: 35428431]
[104]
Holm-Bentzen M, Jacobsen F, Nerstrøm B, Lose G, Kristensen JK, Pedersen RH, Krarup T, Feggetter J, Bates P, Barnard R. A prospective double-blind clinically controlled multicenter trial of sodium pentosanpolysulfate in the treatment of interstitial cystitis and related painful bladder disease. The Journal of urology. 1987 Sep:138(3):503-7
[PubMed PMID: 2442415]
Level 1 (high-level) evidence
[105]
Nickel JC, Herschorn S, Whitmore KE, Forrest JB, Hu P, Friedman AJ, Baseman AS. Pentosan polysulfate sodium for treatment of interstitial cystitis/bladder pain syndrome: insights from a randomized, double-blind, placebo controlled study. The Journal of urology. 2015 Mar:193(3):857-62. doi: 10.1016/j.juro.2014.09.036. Epub 2014 Sep 20
[PubMed PMID: 25245489]
Level 1 (high-level) evidence
[106]
Mulholland SG, Hanno P, Parsons CL, Sant GR, Staskin DR. Pentosan polysulfate sodium for therapy of interstitial cystitis. A double-blind placebo-controlled clinical study. Urology. 1990 Jun:35(6):552-8
[PubMed PMID: 1693797]
Level 1 (high-level) evidence
[107]
Parsons CL, Benson G, Childs SJ, Hanno P, Sant GR, Webster G. A quantitatively controlled method to study prospectively interstitial cystitis and demonstrate the efficacy of pentosanpolysulfate. The Journal of urology. 1993 Sep:150(3):845-8
[PubMed PMID: 7688432]
[108]
Parsons CL, Mulholland SG. Successful therapy of interstitial cystitis with pentosanpolysulfate. The Journal of urology. 1987 Sep:138(3):513-6
[PubMed PMID: 2442417]
[109]
Hanno PM. Analysis of long-term Elmiron therapy for interstitial cystitis. Urology. 1997 May:49(5A Suppl):93-9
[PubMed PMID: 9146008]
[111]
Pearce WA, Chen R, Jain N. Pigmentary Maculopathy Associated with Chronic Exposure to Pentosan Polysulfate Sodium. Ophthalmology. 2018 Nov:125(11):1793-1802. doi: 10.1016/j.ophtha.2018.04.026. Epub 2018 May 22
[PubMed PMID: 29801663]
[112]
Ohning C, Skopis G, Levinson J, Kasi S. Characteristics of Pentosan Polysulfate Sodium-Associated Maculopathy and Similarities With Other Maculopathies Commonly Managed in a Retina Practice. Journal of vitreoretinal diseases. 2022 Mar-Apr:6(2):104-110. doi: 10.1177/24741264211020259. Epub 2021 Jul 30
[PubMed PMID: 37008666]
[113]
Hanif AM, Armenti ST, Taylor SC, Shah RA, Igelman AD, Jayasundera KT, Pennesi ME, Khurana RN, Foote JE, O'Keefe GA, Yang P, Hubbard GB 3rd, Hwang TS, Flaxel CJ, Stein JD, Yan J, Jain N. Phenotypic Spectrum of Pentosan Polysulfate Sodium-Associated Maculopathy: A Multicenter Study. JAMA ophthalmology. 2019 Nov 1:137(11):1275-1282. doi: 10.1001/jamaophthalmol.2019.3392. Epub
[PubMed PMID: 31486843]
Level 2 (mid-level) evidence
[114]
Jain N, Li AL, Yu Y, VanderBeek BL. Association of macular disease with long-term use of pentosan polysulfate sodium: findings from a US cohort. The British journal of ophthalmology. 2020 Aug:104(8):1093-1097. doi: 10.1136/bjophthalmol-2019-314765. Epub 2019 Nov 6
[PubMed PMID: 31694837]
[115]
Mukhopadhyay C, Boyce TM, Gehrs KM, Folk JC, Mullins RF, Luo Y, Kreder K, Sohn EH. Age-Related Macular Degeneration Masquerade: A Review of Pentosan Polysulfate Maculopathy and Implications for Clinical Practice. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.). 2022 Mar-Apr 01:11(2):100-110. doi: 10.1097/APO.0000000000000504. Epub
[PubMed PMID: 35533330]
[116]
Priluck A, Fung AT, Singh MS. Pentosan polysulfate maculopathy: a brief primer for general practitioners, ophthalmologists, optometrists and urologists. The Medical journal of Australia. 2023 May 1:218(8):348-350. doi: 10.5694/mja2.51913. Epub 2023 Mar 29
[PubMed PMID: 36990107]
[117]
Jung EH, Lindeke-Myers A, Jain N. Two-Year Outcomes After Variable Duration of Drug Cessation in Patients With Maculopathy Associated With Pentosan Polysulfate Use. JAMA ophthalmology. 2023 Mar 1:141(3):260-266. doi: 10.1001/jamaophthalmol.2022.6093. Epub
[PubMed PMID: 36729449]
[118]
Greig J, Mak Q, Furrer MA, Sahai A, Raison N. Sacral neuromodulation in the management of chronic pelvic pain: A systematic review and meta-analysis. Neurourology and urodynamics. 2023 Apr:42(4):822-836. doi: 10.1002/nau.25167. Epub 2023 Mar 6
[PubMed PMID: 36877182]
Level 1 (high-level) evidence
[120]
Peters KM, Konstandt D. Sacral neuromodulation decreases narcotic requirements in refractory interstitial cystitis. BJU international. 2004 Apr:93(6):777-9
[PubMed PMID: 15049989]
[121]
Alkis O, Aras B, Sevim M, Kartal İG, Sönmez OY, İvelik Hİ. Efficacy of transcutaneous tibial nerve stimulation in the treatment of bladder pain syndrome. Current urology. 2022 Jun:16(2):83-87. doi: 10.1097/CU9.0000000000000082. Epub 2022 Jan 27
[PubMed PMID: 36570363]
[122]
Padilla-Fernández B, Hernández-Hernández D, Castro-Díaz DM. Current role of neuromodulation in bladder pain syndrome/interstitial cystitis. Therapeutic advances in urology. 2022 Jan-Dec:14():17562872221135941. doi: 10.1177/17562872221135941. Epub 2022 Nov 21
[PubMed PMID: 36438605]
Level 3 (low-level) evidence
[123]
Elhilali MM, Khaled SM, Kashiwabara T, Elzayat E, Corcos J. Sacral neuromodulation: long-term experience of one center. Urology. 2005 Jun:65(6):1114-7
[PubMed PMID: 15913732]
[124]
Sogutdelen E, Citamak B. Efficacy of intravesical cocktail therapy with or without dimethyl sulphoxide in interstitial cystitis. Central European journal of urology. 2022:75(3):299-304. doi: 10.5173/ceju.2022.129. Epub 2022 Sep 24
[PubMed PMID: 36381159]
[125]
Perez-Marrero R, Emerson LE, Feltis JT. A controlled study of dimethyl sulfoxide in interstitial cystitis. The Journal of urology. 1988 Jul:140(1):36-9
[PubMed PMID: 3288775]
[126]
Moss NP, Chill HH, Sand PK, Chang C, Goldberg RP, Gafni-Kane A. A prospective, randomized trial comparing intravesical dimethyl sulfoxide (DMSO) to bupivacaine, triamcinolone, and heparin (BTH), for newly diagnosed interstitial cystitis/painful bladder syndrome (IC/PBS). Neurourology and urodynamics. 2023 Mar:42(3):615-622. doi: 10.1002/nau.25142. Epub 2023 Feb 6
[PubMed PMID: 36747494]
Level 1 (high-level) evidence
[127]
Yoshimura N, Homma Y, Tomoe H, Otsuka A, Kitta T, Masumori N, Akiyama Y, Niimi A, Mitsui T, Nanri M, Namima T, Takei M, Yamaguchi A, Sekiguchi Y, Kajiwara M, Kobayashi S, Ameda K, Ohashi Y, Sakamoto S, Muraki O, Shishido T, Kageyama S, Kokura K, Okazoe H, Yamanishi T, Watanabe T, Uno T, Ohinata A, Ueda T. Efficacy and safety of intravesical instillation of KRP-116D (50% dimethyl sulfoxide solution) for interstitial cystitis/bladder pain syndrome in Japanese patients: A multicenter, randomized, double-blind, placebo-controlled, clinical study. International journal of urology : official journal of the Japanese Urological Association. 2021 May:28(5):545-553. doi: 10.1111/iju.14505. Epub 2021 Feb 12
[PubMed PMID: 33580603]
Level 1 (high-level) evidence
[128]
Hung MJ, Chen YT, Shen PS, Hsu ST, Chen GD, Ho ES. Risk factors that affect the treatment of interstitial cystitis using intravesical therapy with a dimethyl sulfoxide cocktail. International urogynecology journal. 2012 Nov:23(11):1533-9. doi: 10.1007/s00192-012-1699-x. Epub 2012 Mar 17
[PubMed PMID: 22426874]
[129]
Iyer S, Lotsof E, Zhou Y, Tran A, Botros C, Sand P, Goldberg R, Tomezsko J, Gafni-Kane A, Botros S. Which bladder instillations are more effective? DMSO vs. bupivacaine/heparin/triamcinolone: a retrospective study. International urogynecology journal. 2017 Sep:28(9):1335-1340. doi: 10.1007/s00192-017-3266-y. Epub 2017 Feb 1
[PubMed PMID: 28150028]
Level 2 (mid-level) evidence
[130]
Tomoe H. In what type of interstitial cystitis/bladder pain syndrome is DMSO intravesical instillation therapy effective? Translational andrology and urology. 2015 Dec:4(6):600-4. doi: 10.3978/j.issn.2223-4683.2015.09.01. Epub
[PubMed PMID: 26816859]
[131]
Parsons CL, Housley T, Schmidt JD, Lebow D. Treatment of interstitial cystitis with intravesical heparin. British journal of urology. 1994 May:73(5):504-7
[PubMed PMID: 8012771]
[132]
Parsons CL, Zupkas P, Proctor J, Koziol J, Franklin A, Giesing D, Davis E, Lakin CM, Kahn BS, Garner WJ. Alkalinized lidocaine and heparin provide immediate relief of pain and urgency in patients with interstitial cystitis. The journal of sexual medicine. 2012 Jan:9(1):207-12. doi: 10.1111/j.1743-6109.2011.02542.x. Epub 2011 Nov 14
[PubMed PMID: 22082303]
[133]
Parsons CL, Koziol JA, Proctor JG, Zupkas P, Argade S. Heparin and alkalinized lidocaine versus alkalinized lidocaine for treatment of interstitial cystitis symptoms. The Canadian journal of urology. 2015 Apr:22(2):7739-44
[PubMed PMID: 25891339]
[134]
Digesu GA, Tailor V, Bhide AA, Khullar V. The role of bladder instillation in the treatment of bladder pain syndrome: Is intravesical treatment an effective option for patients with bladder pain as well as LUTS? International urogynecology journal. 2020 Jul:31(7):1387-1392. doi: 10.1007/s00192-020-04303-7. Epub 2020 May 1
[PubMed PMID: 32358624]
[135]
Madurga Patuel B, González-López R, Resel Folkersma L, Machado Fernández G, Adot Zurbano JM, Bonillo MÁ, Vozmediano Chicharro R, Zubiaur Líbano C. Recommendations on the use of intravesical hyaluronic acid instillations in bladder pain syndrome. Actas urologicas espanolas. 2022 Apr:46(3):131-137. doi: 10.1016/j.acuroe.2022.02.007. Epub 2022 Mar 4
[PubMed PMID: 35256323]
[136]
Han XM, Wu XH, Li B, Pan F, Li WC, Liu SL, Zeng FQ, Chen M. The effects of intravesical therapy with hyaluronic acid for painful bladder syndrome: Preliminary Chinese experience and systematic review. Taiwanese journal of obstetrics & gynecology. 2015 Jun:54(3):240-7. doi: 10.1016/j.tjog.2014.09.007. Epub
[PubMed PMID: 26166334]
Level 1 (high-level) evidence
[137]
Pyo JS, Cho WJ. Systematic Review and Meta-Analysis of Intravesical Hyaluronic Acid and Hyaluronic Acid/Chondroitin Sulfate Instillation for Interstitial Cystitis/Painful Bladder Syndrome. Cellular physiology and biochemistry : international journal of experimental cellular physiology, biochemistry, and pharmacology. 2016:39(4):1618-25. doi: 10.1159/000447863. Epub 2016 Sep 15
[PubMed PMID: 27627755]
Level 1 (high-level) evidence
[138]
Rooney P, Srivastava A, Watson L, Quinlan LR, Pandit A. Hyaluronic acid decreases IL-6 and IL-8 secretion and permeability in an inflammatory model of interstitial cystitis. Acta biomaterialia. 2015 Jun:19():66-75. doi: 10.1016/j.actbio.2015.02.030. Epub 2015 Mar 26
[PubMed PMID: 25818949]
[139]
Liang CC, Lin YH, Hsieh WC, Huang L. Urinary and psychological outcomes in women with interstitial cystitis/bladder pain syndrome following hyaluronic acid treatment. Taiwanese journal of obstetrics & gynecology. 2018 Jun:57(3):360-363. doi: 10.1016/j.tjog.2018.04.006. Epub
[PubMed PMID: 29880165]
[140]
Hung MJ, Tsai CP, Lin YH, Huang WC, Chen GD, Shen PS. Hyaluronic acid improves pain symptoms more than bladder storage symptoms in women with interstitial cystitis. Taiwanese journal of obstetrics & gynecology. 2019 May:58(3):417-422. doi: 10.1016/j.tjog.2018.11.033. Epub
[PubMed PMID: 31122535]
[141]
Henry RA, Morales A, Cahill CM. Beyond a Simple Anesthetic Effect: Lidocaine in the Diagnosis and Treatment of Interstitial Cystitis/bladder Pain Syndrome. Urology. 2015 May:85(5):1025-1033. doi: 10.1016/j.urology.2015.01.021. Epub
[PubMed PMID: 25917728]
[142]
Liu T, Zhang L, Joo D, Sun SC. NF-κB signaling in inflammation. Signal transduction and targeted therapy. 2017:2():17023-. doi: 10.1038/sigtrans.2017.23. Epub 2017 Jul 14
[PubMed PMID: 29158945]
[143]
Abdel-Mageed AB, Bajwa A, Shenassa BB, Human L, Ghoniem GM. NF-kappaB-dependent gene expression of proinflammatory cytokines in T24 cells: possible role in interstitial cystitis. Urological research. 2003 Oct:31(5):300-5
[PubMed PMID: 14574533]
[145]
Tyagi P, Li Z, Chancellor M, De Groat WC, Yoshimura N, Huang L. Sustained intravesical drug delivery using thermosensitive hydrogel. Pharmaceutical research. 2004 May:21(5):832-7
[PubMed PMID: 15180342]
[146]
Gray KJ, Engelmann UH, Johnson EH, Fishman IJ. Evaluation of misoprostol cytoprotection of the bladder with cyclophosphamide (Cytoxan) therapy. The Journal of urology. 1986 Aug:136(2):497-500
[PubMed PMID: 3090278]
[147]
Kelly JD, Young MR, Johnston SR, Keane PF. Clinical response to an oral prostaglandin analogue in patients with interstitial cystitis. European urology. 1998:34(1):53-6
[PubMed PMID: 9676414]
[148]
Cardenas-Trowers OO, Abraham AG, Dotson TK, Houlette BA, Gaskins JT, Francis SL. Bladder Instillations With Triamcinolone Acetonide for Interstitial Cystitis-Bladder Pain Syndrome: A Randomized Controlled Trial. Obstetrics and gynecology. 2021 May 1:137(5):810-819. doi: 10.1097/AOG.0000000000004348. Epub
[PubMed PMID: 33831942]
Level 1 (high-level) evidence
[149]
Jiang T, Zhou X, Chen Z, Xiong T, Fu J, Liu Z, Yan D, Zhou Z, Shen W. Clinical efficacy of submucosal injection of triamcinolone acetonide in the treatment of type II/III interstitial cystitis/bladder pain syndrome. BMC urology. 2020 Mar 30:20(1):36. doi: 10.1186/s12894-020-00597-3. Epub 2020 Mar 30
[PubMed PMID: 32228552]
[150]
Gülpınar O, Haliloğlu AH, Gökce Mİ, Arıkan N. Instillation of Hyaluronic Acid via Electromotive Drug Administration Can Improve the Efficacy of Treatment in Patients With Interstitial Cystitis/Painful Bladder Syndrome: A Randomized Prospective Study. Korean journal of urology. 2014 May:55(5):354-9. doi: 10.4111/kju.2014.55.5.354. Epub 2014 May 12
[PubMed PMID: 24868341]
Level 1 (high-level) evidence
[151]
Hashemi S, Sahai A, Malde S. Applications of electromotive drug administration in urology. Urology annals. 2020 Oct-Dec:12(4):301-308. doi: 10.4103/UA.UA_152_19. Epub 2020 Oct 15
[PubMed PMID: 33776323]
[152]
Kuo HC. Repeated intravesical onabotulinumtoxinA injections are effective in treatment of refractory interstitial cystitis/bladder pain syndrome. International journal of clinical practice. 2013 May:67(5):427-34. doi: 10.1111/ijcp.12113. Epub
[PubMed PMID: 23574103]
[153]
Pinto RA, Costa D, Morgado A, Pereira P, Charrua A, Silva J, Cruz F. Intratrigonal OnabotulinumtoxinA Improves Bladder Symptoms and Quality of Life in Patients with Bladder Pain Syndrome/Interstitial Cystitis: A Pilot, Single Center, Randomized, Double-Blind, Placebo Controlled Trial. The Journal of urology. 2018 Apr:199(4):998-1003. doi: 10.1016/j.juro.2017.10.018. Epub 2017 Oct 13
[PubMed PMID: 29031769]
Level 1 (high-level) evidence
[154]
Kuo HC, Chancellor MB. Comparison of intravesical botulinum toxin type A injections plus hydrodistention with hydrodistention alone for the treatment of refractory interstitial cystitis/painful bladder syndrome. BJU international. 2009 Sep:104(5):657-61. doi: 10.1111/j.1464-410X.2009.08495.x. Epub 2009 Mar 30
[PubMed PMID: 19338543]
[155]
Giannantoni A, Gubbiotti M, Bini V. Botulinum Neurotoxin A Intravesical Injections in Interstitial Cystitis/Bladder Painful Syndrome: A Systematic Review with Meta-Analysis. Toxins. 2019 Aug 30:11(9):. doi: 10.3390/toxins11090510. Epub 2019 Aug 30
[PubMed PMID: 31480323]
Level 1 (high-level) evidence
[156]
Panunzio A, Tafuri A, Mazzucato G, Cerrato C, Orlando R, Pagliarulo V, Antonelli A, Cerruto MA. Botulinum Toxin-A Injection in Chronic Pelvic Pain Syndrome Treatment: A Systematic Review and Pooled Meta-Analysis. Toxins. 2022 Jan 1:14(1):. doi: 10.3390/toxins14010025. Epub 2022 Jan 1
[PubMed PMID: 35051002]
Level 1 (high-level) evidence
[157]
Lee CL, Kuo HC. Long-Term Efficacy and Safety of Repeated Intravescial OnabotulinumtoxinA Injections Plus Hydrodistention in the Treatment of Interstitial Cystitis/Bladder Pain Syndrome. Toxins. 2015 Oct 22:7(10):4283-93. doi: 10.3390/toxins7104283. Epub 2015 Oct 22
[PubMed PMID: 26506388]
[158]
Wang Y, Zheng J, Li Z, Jiang Y, Yu J, Li S, Chen X. Modified Botulinum Toxin Type A Injections Improve Symptoms Associated With Interstitial Cystitis/Bladder Pain Syndrome in Women: A Retrospective Cohort Study. Urology. 2024 Jul:189():27-33. doi: 10.1016/j.urology.2024.04.039. Epub 2024 May 4
[PubMed PMID: 38710455]
Level 2 (mid-level) evidence
[159]
Kuo HC, Jiang YH, Tsai YC, Kuo YC. Intravesical botulinum toxin-A injections reduce bladder pain of interstitial cystitis/bladder pain syndrome refractory to conventional treatment - A prospective, multicenter, randomized, double-blind, placebo-controlled clinical trial. Neurourology and urodynamics. 2016 Jun:35(5):609-14. doi: 10.1002/nau.22760. Epub 2015 Apr 24
[PubMed PMID: 25914337]
Level 1 (high-level) evidence
[160]
Pinto R, Lopes T, Silva J, Silva C, Dinis P, Cruz F. Persistent therapeutic effect of repeated injections of onabotulinum toxin a in refractory bladder pain syndrome/interstitial cystitis. The Journal of urology. 2013 Feb:189(2):548-53. doi: 10.1016/j.juro.2012.09.027. Epub 2012 Dec 14
[PubMed PMID: 23253961]
[161]
Imamura M, Scott NW, Wallace SA, Ogah JA, Ford AA, Dubos YA, Brazzelli M. Interventions for treating people with symptoms of bladder pain syndrome: a network meta-analysis. The Cochrane database of systematic reviews. 2020 Jul 30:7(7):CD013325. doi: 10.1002/14651858.CD013325.pub2. Epub 2020 Jul 30
[PubMed PMID: 32734597]
Level 1 (high-level) evidence
[162]
Walker SJ, Plair A, Hemal K, Langefeld CD, Matthews C, Badlani G, Zambon J, Heath H, Evans RJ. Bladder Hydrodistention Does Not Result in a Significant Change in Bladder Capacity for Interstitial Cystitis/Bladder Pain Syndrome Patients. Urology. 2019 Oct:132():81-86. doi: 10.1016/j.urology.2019.06.031. Epub 2019 Jul 9
[PubMed PMID: 31299328]
[163]
Glemain P, Rivière C, Lenormand L, Karam G, Bouchot O, Buzelin JM. Prolonged hydrodistention of the bladder for symptomatic treatment of interstitial cystitis: efficacy at 6 months and 1 year. European urology. 2002 Jan:41(1):79-84
[PubMed PMID: 11999471]
[164]
Peters KM. Neuromodulation for the treatment of refractory interstitial cystitis. Reviews in urology. 2002:4 Suppl 1(Suppl 1):S36-43
[PubMed PMID: 16986033]
[165]
Wang J, Chen Y, Chen J, Zhang G, Wu P. Sacral Neuromodulation for Refractory Bladder Pain Syndrome/Interstitial Cystitis: a Global Systematic Review and Meta-analysis. Scientific reports. 2017 Sep 8:7(1):11031. doi: 10.1038/s41598-017-11062-x. Epub 2017 Sep 8
[PubMed PMID: 28887515]
Level 1 (high-level) evidence
[166]
Mahran A, Baaklini G, Hassani D, Abolella HA, Safwat AS, Neudecker M, Hijaz AK, Mahajan ST, Siegel SW, El-Nashar SA. Sacral neuromodulation treating chronic pelvic pain: a meta-analysis and systematic review of the literature. International urogynecology journal. 2019 Jul:30(7):1023-1035. doi: 10.1007/s00192-019-03898-w. Epub 2019 Mar 14
[PubMed PMID: 30874835]
Level 1 (high-level) evidence
[167]
Yang TX, Luo DY, Li H, Wang KJ, Shen H. Is Urethrectomy Necessary During Cystectomy in Patients With Interstitial Cystitis or Bladder Pain Syndrome? Urology. 2016 Nov:97():73-79. doi: 10.1016/j.urology.2016.07.003. Epub 2016 Jul 14
[PubMed PMID: 27424120]
[168]
Costello AJ, Crowe H, Agarwal D. Supratrigonal cystectomy and ileocystoplasty in management of interstitial cystitis. The Australian and New Zealand journal of surgery. 2000 Jan:70(1):34-8
[PubMed PMID: 10696940]
[169]
Kim HJ, Lee JS, Cho WJ, Lee HS, Lee HN, You HW, Jung W, Lee KS. Efficacy and safety of augmentation ileocystoplasty combined with supratrigonal cystectomy for the treatment of refractory bladder pain syndrome/interstitial cystitis with Hunner's lesion. International journal of urology : official journal of the Japanese Urological Association. 2014 Apr:21 Suppl 1():69-73. doi: 10.1111/iju.12320. Epub
[PubMed PMID: 24807503]
[170]
Madec FX, Hedhli O, Perrouin-Verbe MA, Levesque A, Le Normand L, Rigaud J. Feasibility, Morbidity, and Functional Results of Supratrigonal Cystectomy with Augmentation Ileocystoplasty by Combined Robot-Assisted Laparoscopy and Mini-Laparotomy Approach. Journal of endourology. 2017 Jul:31(7):655-660. doi: 10.1089/end.2017.0107. Epub 2017 Jun 6
[PubMed PMID: 28467725]
Level 2 (mid-level) evidence
[171]
Queissert F, Bruecher B, van Ophoven A, Schrader AJ. Supratrigonal cystectomy and augmentation cystoplasty with ileum or ileocecum in the treatment of ulcerative interstitial cystitis/bladder pain syndrome: a 14-year follow-up. International urogynecology journal. 2022 May:33(5):1267-1272. doi: 10.1007/s00192-022-05110-y. Epub 2022 Mar 1
[PubMed PMID: 35230481]
[172]
Osman NI, Bratt DG, Downey AP, Esperto F, Inman RD, Chapple CR. A Systematic Review of Surgical interventions for the Treatment of Bladder Pain Syndrome/Interstitial Cystitis. European urology focus. 2021 Jul:7(4):877-885. doi: 10.1016/j.euf.2020.02.014. Epub 2020 Mar 1
[PubMed PMID: 32127327]
[173]
Mykoniatis I, Tsiakaras S, Samarinas M, Anastasiadis A, Symeonidis EN, Sountoulides P. Monoclonal Antibody Therapy for the Treatment of Interstitial Cystitis. Biologics : targets & therapy. 2022:16():47-55. doi: 10.2147/BTT.S290286. Epub 2022 May 20
[PubMed PMID: 35619987]
[174]
Kocatürk H, Atasoy N, Bedir F, Altay MS, Demirdöğen ŞO, Koç E, Yilmaz S. Questionnaire-guided evaluation of the effectiveness of long-term intravesical 0.2% chondroitin sulfate therapy in interstitial cystitis. International urogynecology journal. 2021 May:32(5):1293-1298. doi: 10.1007/s00192-020-04245-0. Epub 2020 Feb 11
[PubMed PMID: 32047969]
[175]
Danacioglu YO, Erol B, Ozkanli S, Yildirim A, Atis RG, Silay MS, Caskurlu T. Comparison of Intravesical Hyaluronic Acid, Chondroitin Sulfate, and Combination of Hyaluronic Acid-Chondroitin Sulfate Therapies in Animal Model of Interstitial Cystitis. International neurourology journal. 2021 Mar:25(1):42-50. doi: 10.5213/inj.1938176.088. Epub 2021 Jan 19
[PubMed PMID: 33504136]
Level 3 (low-level) evidence
[176]
Özkıdık M. Assessment of long-term intravesical hyaluronic acid, chondroitin sulfate and combination therapy for patients with bladder pain syndrome. Central European journal of urology. 2019:72(3):270-275. doi: 10.5173/ceju.2019.0007. Epub 2019 Sep 16
[PubMed PMID: 31720029]
[177]
Stellavato A, Pirozzi AVA, Diana P, Reale S, Vassallo V, Fusco A, Donnarumma G, De Rosa M, Schiraldi C. Hyaluronic acid and chondroitin sulfate, alone or in combination, efficiently counteract induced bladder cell damage and inflammation. PloS one. 2019:14(6):e0218475. doi: 10.1371/journal.pone.0218475. Epub 2019 Jun 25
[PubMed PMID: 31237905]
[178]
Lee YK, Jiang YH, Jhang JF, Ho HC, Kuo HC. Changes in the Ultrastructure of the Bladder Urothelium in Patients with Interstitial Cystitis after Intravesical Injections of Platelet-Rich Plasma. Biomedicines. 2022 May 20:10(5):. doi: 10.3390/biomedicines10051182. Epub 2022 May 20
[PubMed PMID: 35625918]
[179]
Gallego-Vilar D, García-Fadrique G, Povo-Martin I, Salvador-Marin M, Gallego-Gomez J. Maintenance of the response to dimethyl sulfoxide treatment using hyperbaric oxygen in interstitial cystitis/painful bladder syndrome: a prospective, randomized, comparative study. Urologia internationalis. 2013:90(4):411-6. doi: 10.1159/000343697. Epub 2013 Mar 13
[PubMed PMID: 23485788]
Level 1 (high-level) evidence
[180]
Chuang YC, Lee WC, Lee WC, Chiang PH. Intravesical liposome versus oral pentosan polysulfate for interstitial cystitis/painful bladder syndrome. The Journal of urology. 2009 Oct:182(4):1393-400. doi: 10.1016/j.juro.2009.06.024. Epub 2009 Aug 15
[PubMed PMID: 19683290]
[181]
Tyagi P, Kashyap M, Majima T, Kawamorita N, Yoshizawa T, Yoshimura N. Intravesical liposome therapy for interstitial cystitis. International journal of urology : official journal of the Japanese Urological Association. 2017 Apr:24(4):262-271. doi: 10.1111/iju.13317. Epub 2017 Mar 4
[PubMed PMID: 28258657]
[182]
Wen C, Xie L, Hu C. Roles of mesenchymal stem cells and exosomes in interstitial cystitis/bladder pain syndrome. Journal of cellular and molecular medicine. 2022 Feb:26(3):624-635. doi: 10.1111/jcmm.17132. Epub 2021 Dec 24
[PubMed PMID: 34953040]
[183]
Etulain J. Platelets in wound healing and regenerative medicine. Platelets. 2018 Sep:29(6):556-568. doi: 10.1080/09537104.2018.1430357. Epub 2018 Feb 14
[PubMed PMID: 29442539]
[184]
Mussano F, Genova T, Munaron L, Petrillo S, Erovigni F, Carossa S. Cytokine, chemokine, and growth factor profile of platelet-rich plasma. Platelets. 2016 Jul:27(5):467-71. doi: 10.3109/09537104.2016.1143922. Epub 2016 Mar 7
[PubMed PMID: 26950533]
[185]
Kuffler DP. Platelet-rich plasma and the elimination of neuropathic pain. Molecular neurobiology. 2013 Oct:48(2):315-32. doi: 10.1007/s12035-013-8494-7. Epub 2013 Jul 7
[PubMed PMID: 23832571]
[186]
Jhang JF, Wu SY, Lin TY, Kuo HC. Repeated intravesical injections of platelet-rich plasma are effective in the treatment of interstitial cystitis: a case control pilot study. Lower urinary tract symptoms. 2019 Apr:11(2):O42-O47. doi: 10.1111/luts.12212. Epub 2017 Dec 19
[PubMed PMID: 29265766]
Level 2 (mid-level) evidence
[187]
Jhang JF, Lin TY, Kuo HC. Intravesical injections of platelet-rich plasma is effective and safe in treatment of interstitial cystitis refractory to conventional treatment-A prospective clinical trial. Neurourology and urodynamics. 2019 Feb:38(2):703-709. doi: 10.1002/nau.23898. Epub 2018 Dec 21
[PubMed PMID: 30576011]
[188]
Jiang YH, Kuo YC, Jhang JF, Lee CL, Hsu YH, Ho HC, Kuo HC. Repeated intravesical injections of platelet-rich plasma improve symptoms and alter urinary functional proteins in patients with refractory interstitial cystitis. Scientific reports. 2020 Sep 16:10(1):15218. doi: 10.1038/s41598-020-72292-0. Epub 2020 Sep 16
[PubMed PMID: 32939046]
[189]
Jhang JF, Jiang YH, Hsu YH, Ho HC, Birder LA, Lin TY, Kuo HC. Improved Urothelial Cell Proliferation, Cytoskeleton and Barrier Function Protein Expression in the Patients With Interstitial Cystitis/Bladder Pain Syndrome After Intravesical Platelet-Rich Plasma Injection. International neurourology journal. 2022 Feb:26(Suppl 1):S57-67. doi: 10.5213/inj.2142100.050. Epub 2022 Jan 20
[PubMed PMID: 35073671]
[190]
Ke QS, Jhang JF, Lin TY, Ho HC, Jiang YH, Hsu YH, Kuo HC. Therapeutic potential of intravesical injections of platelet-rich plasma in the treatment of lower urinary tract disorders due to regenerative deficiency. Ci ji yi xue za zhi = Tzu-chi medical journal. 2019 Jul-Sep:31(3):135-143. doi: 10.4103/tcmj.tcmj_92_19. Epub
[PubMed PMID: 31258287]
[191]
Li H, Zhang Z, Peng J, Xin Z, Li M, Yang B, Fang D, Tang Y, Guo Y. Treatment with low-energy shock wave alleviates pain in an animal model of uroplakin 3A-induced autoimmune interstitial cystitis/painful bladder syndrome. Investigative and clinical urology. 2019 Sep:60(5):359-366. doi: 10.4111/icu.2019.60.5.359. Epub 2019 Aug 30
[PubMed PMID: 31501798]
Level 3 (low-level) evidence
[192]
Jiang YH, Jhang JF, Lee YK, Kuo HC. Low-Energy Shock Wave Plus Intravesical Instillation of Botulinum Toxin A for Interstitial Cystitis/Bladder Pain Syndrome: Pathophysiology and Preliminary Result of a Novel Minimally Invasive Treatment. Biomedicines. 2022 Feb 7:10(2):. doi: 10.3390/biomedicines10020396. Epub 2022 Feb 7
[PubMed PMID: 35203604]
[193]
Jhang JF, Hsu YH, Peng CW, Jiang YH, Ho HC, Kuo HC. Epstein-Barr Virus as a Potential Etiology of Persistent Bladder Inflammation in Human Interstitial Cystitis/Bladder Pain Syndrome. The Journal of urology. 2018 Sep:200(3):590-596. doi: 10.1016/j.juro.2018.03.133. Epub 2018 Apr 11
[PubMed PMID: 29653163]
[194]
Marcu I, Campian EC, Tu FF. Interstitial Cystitis/Bladder Pain Syndrome. Seminars in reproductive medicine. 2018 Mar:36(2):123-135. doi: 10.1055/s-0038-1676089. Epub 2018 Dec 19
[PubMed PMID: 30566978]
[195]
Cvach K, Rosamilia A. Review of intravesical therapies for bladder pain syndrome/interstitial cystitis. Translational andrology and urology. 2015 Dec:4(6):629-37. doi: 10.3978/j.issn.2223-4683.2015.10.07. Epub
[PubMed PMID: 26816864]
[196]
Bradley CS, Gallop R, Sutcliffe S, Kreder KJ, Lai HH, Clemens JQ, Naliboff BD, Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network. Long-Term Symptom Trajectories in Urologic Chronic Pelvic Pain Syndrome: A MAPP Research Network Study. Urology. 2022 Nov:169():58-64. doi: 10.1016/j.urology.2022.07.045. Epub 2022 Aug 9
[PubMed PMID: 35961564]
[198]
Axiotakis LG Jr, Youngerman BE, Casals RK, Cooke TS, Winston GM, Chang CL, Boyett DM, Lalwani AK, McKhann GM. Risk of Acquiring Perioperative COVID-19 During the Initial Pandemic Peak: A Retrospective Cohort Study. Annals of surgery. 2021 Jan 1:273(1):41-48. doi: 10.1097/SLA.0000000000004586. Epub
[PubMed PMID: 33156061]
Level 2 (mid-level) evidence
[199]
Gottschalk A, Van Aken H, Zenz M, Standl T. Is anesthesia dangerous? Deutsches Arzteblatt international. 2011 Jul:108(27):469-74. doi: 10.3238/arztebl.2011.0469. Epub 2011 Jul 8
[PubMed PMID: 21814522]
[200]
Fasting S. [Risk in anaesthesia]. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke. 2010 Mar 11:130(5):498-502. doi: 10.4045/tidsskr.08.0666. Epub
[PubMed PMID: 20224619]
[201]
Breau RH, McGrath PJ, Norman RW. Assessing self-help issues for patients with prostate cancer, interstitial cystitis, erectile dysfunction and urinary diversion. BJU international. 2003 Nov:92(7):736-40
[PubMed PMID: 14616457]
[202]
Gohritz A, Dellon AL. Bladder Pain Syndome/Interstitial Cystitis due to Pudendal Nerve Compression: Described in 1915-A Reminder for Treating Pelvic Pain a Century Later. Journal of brachial plexus and peripheral nerve injury. 2020 Jan:15(1):e5-e8. doi: 10.1055/s-0039-1700538. Epub 2020 Mar 6
[PubMed PMID: 32153650]
[203]
Korting GE, Smith SD, Wheeler MA, Weiss RM, Foster HE Jr. A randomized double-blind trial of oral L-arginine for treatment of interstitial cystitis. The Journal of urology. 1999 Feb:161(2):558-65
[PubMed PMID: 9915448]
Level 1 (high-level) evidence
[204]
Murina F, Graziottin A, Felice R, Gambini D. Alpha Lipoic Acid Plus Omega-3 Fatty Acids for Vestibulodynia Associated With Painful Bladder Syndrome. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2017 Mar:39(3):131-137. doi: 10.1016/j.jogc.2016.12.035. Epub
[PubMed PMID: 28343553]
[205]
Di Tucci C, Di Feliciantonio M, Vena F, Capone C, Schiavi MC, Pietrangeli D, Muzii L, Benedetti Panici P. Alpha lipoic acid in obstetrics and gynecology. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology. 2018 Sep:34(9):729-733. doi: 10.1080/09513590.2018.1462320. Epub 2018 May 4
[PubMed PMID: 29726290]
Level 2 (mid-level) evidence
[206]
Katske F, Shoskes DA, Sender M, Poliakin R, Gagliano K, Rajfer J. Treatment of interstitial cystitis with a quercetin supplement. Techniques in urology. 2001 Mar:7(1):44-6
[PubMed PMID: 11272677]
[207]
Bologna RA, Gomelsky A, Lukban JC, Tu LM, Holzberg AS, Whitmore KE. The efficacy of calcium glycerophosphate in the prevention of food-related flares in interstitial cystitis. Urology. 2001 Jun:57(6 Suppl 1):119-20
[PubMed PMID: 11378102]
[208]
Gupta P, Gaines N, Sirls LT, Peters KM. A multidisciplinary approach to the evaluation and management of interstitial cystitis/bladder pain syndrome: an ideal model of care. Translational andrology and urology. 2015 Dec:4(6):611-9. doi: 10.3978/j.issn.2223-4683.2015.10.10. Epub
[PubMed PMID: 26816861]