Continuing Education Activity
Topical oxygen therapy can be considered as an adjunctive modality for the treatment and management of wound care. The device has broad applications for use on wounds. This activity reviews the pathophysiology, indications, contraindications, different types of oxygen therapy and other key elements of topical oxygen therapy in the clinical setting. In addition, this activity will describe the essential points needed by members of an interprofessional team managing the care of patients with wounds.
Objectives:
- Describe the pathophysiology of topical oxygen.
- Identify the indications for the use of topical oxygen therapy.
- Summarize the different mechanisms of delivering oxygen therapy.
- Explain the importance of monitoring for patients receiving topical oxygen therapy.
Introduction
Oxygen boosts vitality to support increased demand during healing. Oxygen is required for multiple intracellular processes, including synthesis and transport.[1] Increased oxygen levels aid the natural capacity to fight infection and are essential for respiratory burst.[2] This production of reactive oxygen species (ROS) is used by neutrophils and macrophages in removing cellular debris and bacteria.[3] Oxygen levels directly affect the rate and the quality of new blood vessel growth in the wound bed. Angiogenesis or new blood vessel formation is essential to the growth and repair of wound healing tissue.[4]
Oxygen levels also directly affect the rate and quality of collagen formation. Oxygen is required by multiple enzymes for the proper formation of fibers and cross-linking of collagen fibers to form organized structures, resulting in better strength with reduced recidivism and improved appearance with reduced scarring. Increasing oxygen levels results in faster cell proliferation, reepithelialization, and collagen formation, all of which accelerate wound healing.[4] Oxygen has been shown to initiate various signaling cascades, including the signaling processes of growth factors. The integral process of recruiting leukocytes, creating angiogenesis, and extracellular matrix formation in diabetic foot ulcers are also affected by oxygen levels.[5]
Anatomy and Physiology
Oxygen transport into a clean, moist wound occurs by diffusion, similar to the pulmonary process of diffusion. In diffusion, gases and liquids move from an area of high partial pressure to areas of low partial pressure. If there is a mixture of gases in a container, the partial pressure of each gas is equal to the pressure that each gas would produce if it occupied the container alone. This applies equally well to the concentration of a gas in a liquid. Thus, if a gas such as oxygen is present above a liquid like the presentation as an open moist wound, the gas will diffuse into the liquid until it reaches equilibrium in concentration (partial pressure) in the liquid in proportion to that present in the gas above it.
Henry's law states that at a constant temperature, the amount of a gas that dissolves in a liquid is directly proportional to the partial pressure of that gas in equilibrium with that liquid. So the solubility of oxygen in the air (pO=KO?xO) is proportional to the partial pressure of oxygen (p0 in Torr), where xO is the mole fraction of oxygen in oxygen-saturated water, and KO is Henry's law constant for oxygen in water (about 3.30×107 K/Torr at 298 K).
Oxygen levels in human tissue contain about 50 mmHg pO at 3 to 4 mm below the wound for wounds exposed to air (21% oxygen (pO = 159 mmHg). By applying topical oxygen wound, the oxygen concentration increases from 21% (pO = 159 mmHg) to 100% (pO = 760 mmHg), to 250 mmHg pO without any additional pressure. These levels have been found experimentally to be optimal for many of the enzymatic pathways involved in the molecular level of the proliferative phase of wound healing.
Topical oxygen increases oxygen levels in the wound bed when pure oxygen is applied directly to the surface of a moist wound at normobaric pressures (slightly above atmospheric, not hyperbaric). Preclinically, pure oxygen applied topically to an open wound has been shown to rapidly and significantly increase the pO of the superficial wound tissue.[6] In this study, the pO was measured using an implanted probe at a depth of 2 mm in the center of the wound bed. The pO was less than 10 mmHg with air above the wound (21% oxygen) and increased over 4-fold to 40 mmHg in 4 minutes upon topical application of pure oxygen.
Indications
Topical oxygen therapy can be used as an adjunctive advanced modality to help to treat chronic wounds failing to respond to a trial of conservative management. Typical wound types that topically applied oxygen is indicated for and/or has demonstrated successful outcomes encompasses a wide range of wound types, including skin ulcerations due to:
- Diabetes
- Vascular ulcers
- Post-surgical infections
- Pressure injury
- Amputations and infected stumps
- Skin grafts
- Cellular tissue-based products
- Prevention of wound dehiscence
- Ischemic tissues
- Burns
- Frostbite
A critical component of wound care is assessment for associated arterial insufficiency. Arterial insufficiency can be the etiology of wound formation or be a limiting factor for the healing. Assessment for arterial insufficiency includes a complete history and physical exam. A screening ankle-brachial index is recommended for chronic lower extremity wounds. If arterial insufficiency is present, the patient should be referred for further workup by a vascular surgeon or specialist. Wounds with associated arterial insufficiency should be considered for revascularization before committing to treatment with hyperbaric or topical oxygen therapy. Following revascularization, topical oxygen therapy may still be indicated if the wound fails to respond to basic wound care.[7]
Contraindications
The limits of topically applied oxygen therapy using advanced systems are still under investigation. For example, it remains yet to be determined if there is a lower limit on ischemia in a wound that would restrict the use of topically applied oxygen. However, because the oxygen diffuses directly into the tissue, it is hypothesized that there may be no lower limit for the therapy to work.
There are few contraindications or precautions for the therapy, yet the same precautions that apply to moist wound therapy apply to topical oxygen. Ensure the wound is free from necrotic tissue. Removing eschar and slough allows oxygen to access the wound directly and has been shown to improve results.[8] Anything that can prevent access of oxygen to the wound should be avoided, including petrolatum-based salves.
Equipment
Regarding delivery of oxygen, the modalities can be classified as inspired or topical and intermittent or continuous. An example of intermittent, inspired oxygen is hyperbaric oxygen (HBO) therapy: the oxygen is applied by breathing concentrated oxygen in a high-pressure chamber (>1.4 atm) for about 90 minutes a day, 3 to 5 days a week. Topically applied oxygen is applied either intermittently, following a treatment regimen similar to HBO (90 minutes a day, 3 to 5 days a week), or continuously (24 hours a day, 7 days a week).[9] Intermittent topical oxygen therapy is used to treat an area directly surrounding a patient’s wound using concentrated (~93%) oxygen at pressures slightly above atmospheric, typically less than 1.1 atm, which is supplied by a high-flow oxygen concentrator and applied using a bag or chamber sealed around the wound. Continuously applied topical oxygen therapy is applied directly to the wound, using pure (>99%), humidified oxygen supplied by a small, wearable electrochemical oxygen generator.
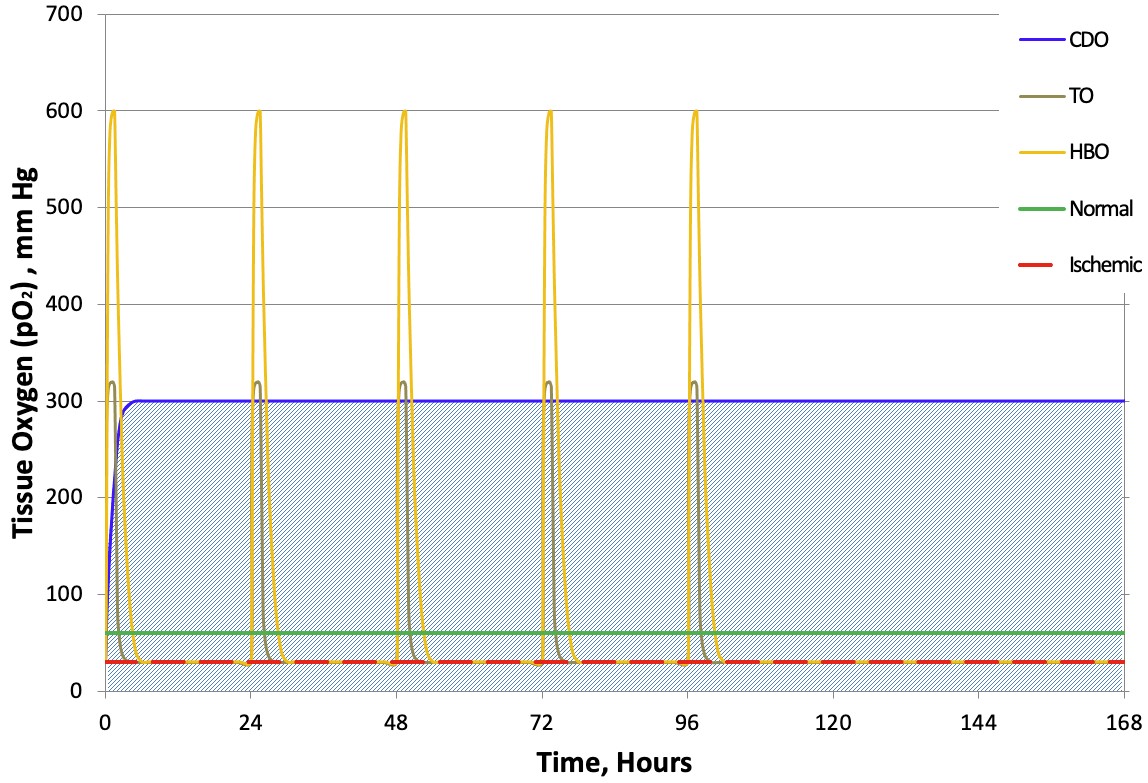
All of these technologies are similar in that they use oxygen as an aid to wound healing. However, several primary differentiating factors determine the amount of oxygen delivered to the wound: pressure, concentration, therapy time, and route of entry. These differences are shown in Table 1. A graphical representation of oxygen therapy time combined with concentration and pressure, which determines the potential amount of oxygen delivered to the wound, is perhaps best portrayed graphically in a typical week-long regimen of oxygen therapy, shown in Figure 1. In this figure, the potential concentration of oxygen reaching the wound is shown for each therapy over time. The area under each curve is representative of the potential amount of oxygen that the wound receives.
Table 1. Primary differentiating factors affecting the amount of oxygen delivered by oxygen therapies.
| Factor |
HBO, Intermittent |
TO, Intermittent |
TO, Continuous (CDO) |
| Pressure |
1.4 to 3.0 atm |
Typically <1.1 atm |
Typically <1.1 atm |
| Concentration |
93 to 99% |
87-93% |
>99% |
| Time |
1.5 hours/day, 3 to 5 days/week
(7.5 hours per week) |
1.5 hours/day, 3 to 5 days/week
(7.5 hours per week) |
24 hours/day, 7 days/week
(168 hours per week) |
| Mode of Oxygen Entry |
Inspired - dependent on blood supply and local microvasculature
|
Direct topical application diffuses directly into tissue
|
Direct topical application diffuses directly into tissue
|
All three modalities rely on oxygen diffusion to deliver oxygen to the affected tissues at the cellular level. HBO relies primarily on inspired oxygen: the oxygen diffuses into and through the alveolar tissue before being picked up by the bloodstream for delivery throughout the body (again by diffusion from the blood/plasma through capillaries and to the target tissue). Once the hemoglobin is saturated, the elevated levels of oxygen are in the plasma itself. A limitation of HBO in wound care is the need for adequate local blood supply to deliver the oxygen to the affected tissues (hence the requirement for minimum TCOM levels in the periphery of the wound). Topically applied oxygen directly diffuses oxygen into the affected tissues, bypassing reliance on local micro-vascularization to deliver oxygen to the wound tissue. This allows oxygen to rapidly penetrate wounds affected by local ischemia.
Classification of Topically Applied Oxygen Therapy
Topically applied oxygen comes in various forms, ranging from large systems consisting of high flow oxygen concentrators bundled with hard-walled chambers to small, wearable oxygen generators with oxygen delivery systems. One of the advantages of all these systems is that they all can be placed/used in most environments, including at home. These systems apply oxygen directly to the wound and can be used adjunctively to many other therapies, including but not limited to moist wound therapy dressings and grafting materials. There are basically three different classes of gaseous topical oxygen delivery (we do not explore liquid, gel, or spray forms here). We will describe them by their most commonly known acronyms: TO, TCOT and CDO. An overview of the similarities and differences between these classes is shown in Table 2. Statements made in the discussions below come from publicly available information in publications or by the manufacturers online.
The first class is the oldest and what is traditionally known as topical oxygen (TO). These systems use a high flow oxygen concentrator connected via oxygen tubing to either a reusable hard-walled chamber or a disposable bag to surround the affected wound. As mentioned above, TO uses the same treatment regimen as HBO to treat wounds: oxygen is applied to the wound for 90-minute sessions, 3 to 5 days per week. The patient is immobile during the treatment, yet TO does allow for treatment in a wide variety of settings, including home care. To enable optimal diffusion of oxygen into the wound, the wound dressing is removed during treatment, and the wound should be kept moist. Unfortunately, the oxygen concentrators used to generate purified oxygen (87 to 93%) are high flow, heavy, and can generate significant noise and heat levels during operation.
The first continuous system, a class is known as transcutaneous oxygen therapy (TCOT), was introduced in the mid-2000s. These devices use tape-based electrochemical oxygen generators to continuously generate pure oxygen from ambient air and provide oxygen to a wound using open-ended tubing that could be placed within a moist wound dressing. The entire system is disposable and intended to be used for up to 15 days before being thrown away and replaced with a new system. The systems are small, lightweight, wearable, and completely silent. This has the advantage that the systems can be worn at all times and carried discreetly.
The latest continuous systems, known as continuous diffusion of oxygen (CDO), appeared within a few years of the first systems. These systems are similar in that they are also small, lightweight, wearable, and completely silent, allowing them to be worn at all times and carried discreetly. However, these systems have several improvements over the early disposable systems, including using robust, compression stacked electrochemical oxygen generators that are reusable and oxygen distribution systems to distribute and diffuse oxygen into the wound bed evenly. These distribution systems are available as fully integrated oxygen diffusion dressings or oxygen distribution wheels, both of which ensure that oxygen is distributed relatively evenly across the entire wound—more on these points later. CDO can be thought of as essentially moist wound therapy plus oxygen. This allows the wounds to “breathe,” similar to how we breathe, continuously.
Table 2. Primary features and specifications for the various classes of topically applied oxygen therapies.
| Feature |
TO |
TCOT |
CDO |
| Therapy Time |
Intermittent
(0 to 1.5 hours/day) |
Continuous
(24 hours/day) |
Continuous
(24 hours/day) |
| Oxygen Source |
Respiratory oxygen concentrator
|
Tape-based electrochemical oxygen generator
|
Compression cell electrochemical oxygen generator |
| Power Source |
Wall Power (up to two 20 amp circuits) |
Disposable batteries |
Rechargeable batteries |
| Noise / Heat |
Noisy and can generate quite a bit of heat |
Silent and cool |
Silent and cool |
| Size / Weight |
Generator large and heavy (up to 30 kgs)
|
Small (fits in palm) and lightweight (<500g) |
Small (fits in palm) and lightweight (<500g) |
| Oxygen Delivery |
A large, solid-walled chamber or disposable bag/boot
|
Open-ended tubing
Requires moist wound therapy dressings not part of the system |
Oxygen distribution system
Diffusion dressing or wheel
|
| Patient Mobile During Treatment |
No
|
Yes
|
Yes
|
| O2 Fire Hazard |
Yes
|
No
|
No
|
Within the various classes of topically applied oxygen, there are differences in the systems available commercially. These differences can affect not only patient satisfaction, yet also therapy outcomes. Refer to Table 3 for comparisons of features of the various systems.
Table 3. Features of various topical oxygen delivery systems.
| |
TO |
TO |
TCOT |
CDO |
CDO |
| Therapy Time |
Intermittent |
Intermittent |
Continuous |
Continuous |
Continuous |
| Oxygen Delivery |
Disposable Bag or Boot |
Disposable Bag or Boot, Reusable Chamber |
Open-Ended Tubing |
Oxygen Distribution System
(ODS) |
Oxygen Diffusion Dressing
(ODD) |
| Pressure at Wound Bed |
Uncontrolled |
Controlled, Cyclic
0 to 50 mm Hg |
Uncontrolled |
Uncontrolled |
Controlled,
Max 20 mm Hg |
| Typical Acronyms |
TO
(Topical Oxygen) |
TWO2
(Topical Wound Oxygen) |
TCOT
(Transcutaneous Continuous Oxygen Therapy) |
CTO
(Continuous Topical Oxygen)
& CDO |
CDO
(Continuous Diffusion of Oxygen) |
| Oxygen Source |
High Flow Oxygen Concentrator |
High Flow Oxygen Concentrator |
Disposable Electrochemical Oxygen Generator |
Electrochemical Oxygen Generator |
Electrochemical Oxygen Generator |
| Oxygen Flow Rate |
Fixed, 6-10 liters/minute
|
Fixed, 6-10 liters/minute
|
Fixed, 3 liters/minute
|
Fixed, 14 liters/minute
|
Adjustable, 3-15 liters/minute
|
| Oxygen Purity |
87-93% |
87-93% |
>99% |
>99% |
>99% |
For TO systems, there are two primary commercial systems available. Both are similar in that they use standard high-flow respiratory oxygen concentrators to supply oxygen to a bag or boot. However, one system does not control the pressure within the bag/boot, and it is therefore relatively constant during the 90-minute therapy session. The other system employs a cyclic pressure controller to vary the pressure at the wound bed from 0 to 50 mm Hg. This cyclic pressure can improve the diffusion of oxygen into the wound. This system also has an option for a solid-walled chamber for placement of the extremity (typically, a lower leg is displayed within the chamber). Both systems have the ability to humidify the oxygen, which is an important feature since dry oxygen would rapidly desiccate the wound surface and impair the delivery of oxygen.
There is only one TCOT system available. While it is the smallest system available, it also has several potential drawbacks compared to other continuous systems. These include the construction of the oxygen generator, lack of flow at low humidity, and lack of alarms to warn the user of malfunction. One item that all continuous systems have in common is that a minimum relative humidity level (typically 30 to 40% r.h.) is required for nominal operation. This disposable device can cease to generate measurable oxygen at low relative humidity levels, for example, in arid or cold environments, such as desert climates or most places in the winter, respectively. The oxygen generator uses a tape membrane that can rupture under excessive pressure with improper offloading and cease functioning. Additionally, the system lacks alarms to notify the patient that the device is not functioning properly.
Two primary CDO systems are commercially available. Both of these systems overcome the shortfalls of the disposable system discussed above. However, low humidity levels can still impact their performance, yet they will continue to produce oxygen at lower levels. One system (CDO with ODD) has a display to warn of low flow and a humidification system to restore nominal operation.
Both systems are similar in that they use robust compression-plate oxygen generators (immune to backpressure from improper offloading), are similar in size and weight, and have oxygen distribution systems for even distribution of oxygen across the wound bed. One of the systems uses a fixed flow of oxygen delivered through an oxygen distribution system (ODS) that consists of tubing connected to a diffusive membrane in the shape of a wheel. The ODS is placed above the wound bed and underneath a moist wound therapy dressing chosen by the wound care provider. The other system uses an integrated oxygen distribution system within an oxygen diffusion dressing (ODD) available in multiple sizes, with or without an adhesive border. This system does not require using other dressings yet can be used with any non-occlusive dressing. The ODD system also has the ability to vary the oxygen flow rate, which can aid in the management of exudate and pain levels and monitor the pressure in the wound bed. The ODD system monitors wound bed pressure and do not allow the pressure in the wound bed to exceed 20 mm Hg, which is at the lowest reported levels of capillary collapse in skin tissue.[10] This may be of significant benefit since it ensures that the localized pressure does not limit the underlying flow of nutrients and blood to the tissue.
Complications
Regarding the therapy's safety and associated devices, topical oxygen therapy is considered safe with no known risks to the patient above moist wound therapy alone. There have been no reported serious adverse events or reactions associated with the use of topically applied oxygen therapy in the literature.
Clinical Significance
The clinical literature regarding the use of topically applied oxygen on open moist wounds has clearly shown that the technology is safe and efficacious for recently advanced implementations. Older literature on the topic of topical oxygen suffers from multiple issues that resulted in a wide variety of outcomes, including not only poor study design but also devices that were not designed and tested to ensure efficacious delivery of oxygen to ensure that the wound stayed moist using humidified oxygen or that the oxygen source delivered oxygen to the wound. Recent advances in topical oxygen device development within the last decade have led to consistent outcomes that demonstrate significant improvements in wound healing. Recent studies using rigorous designs with run-in periods to eliminate non-chronic wounds, full blinding of data with independent analysts, and random enrollment into either the oxygen or a control group have shown excellent results compared to moist wound therapy alone.[11][12][13]
These studies have been analyzed in recent literature reviews, including meta-analysis, which shows that current methods of topically applied oxygen are efficacious in a wide variety of wounds, including diabetic foot ulcers, leg ulcers, and pressure ulcers.[14][15] Of these, a recent meta-analysis reviews double-blinded, randomly controlled studies on diabetic foot ulcers that show that the risk ratio ranges from 1.09 to 4.5, with an overall risk ratio of 1.94.[15] The risk ratio improves to the range of 2.34 to 4.5, with an overall risk ratio of 2.73 when the results of the TCOT device are excluded. Results of TCOT in randomly controlled trials may have been affected by the involvement of weight-bearing wounds. Overall, these studies involved the use of comparative controls and run-in periods to eliminate non-chronic wounds. The trials demonstrate that intervention with topically applied oxygen has significant benefits for diabetic foot ulcers.
These reviews and other recent literature support the efficacy of topically applied oxygen in various wound types. Studies show that oxygen applied directly to wounds resulted in accelerated closure of the wound, either in comparison to the history of the wound on the same patient or in comparison to another standard of wound care therapy. This is even more significant when one considers the types of wounds involved and the duration for which those wounds were unresponsive to other technologies. For example, closure rates using oxygen on recalcitrant wounds were high in studies with open-ended time frames, which are more representative of real-world clinical results than defined time clinical trials, ranging from 73% to 90% full closure.[16][17][18]
The studies show that the use of oxygen resulted in a significant acceleration of the rate of wound closure, thereby significantly reducing the time of treatment. Furthermore, many other beneficial effects of oxygen are listed in recent literature, including dramatic and rapid pain reduction, increased patient compliance, reduced recurrence of wounds, and reduced infection rates and costs.[17][18][17][19] There is also evidence from multiple studies that the relative effect or impact of oxygen, compared to moist wound therapy alone, increases as the wounds get larger, deeper, and more chronic and on weight-bearing surfaces.[11][20][11]
Enhancing Healthcare Team Outcomes
New devices have advanced in the application of topical oxygen therapy to accelerate wound healing, especially in patients with diabetic foot ulcers.[11][12][13][Level 1] Chronic wounds lead to an increase in healthcare costs as well as contribute to reduced quality of life.[19]
Topical oxygen therapy can be administered and monitored by nurses, clinicians, and other providers, including the patient. It is important to understand the different types of topical oxygen available to best suit the patient. Knowing when to apply the device and understanding the importance of an optimal wound bed will improve the oxygen delivery to the tissues. An interprofessional team that provides an integrated approach to patient care can help achieve the best possible outcomes.