Continuing Education Activity
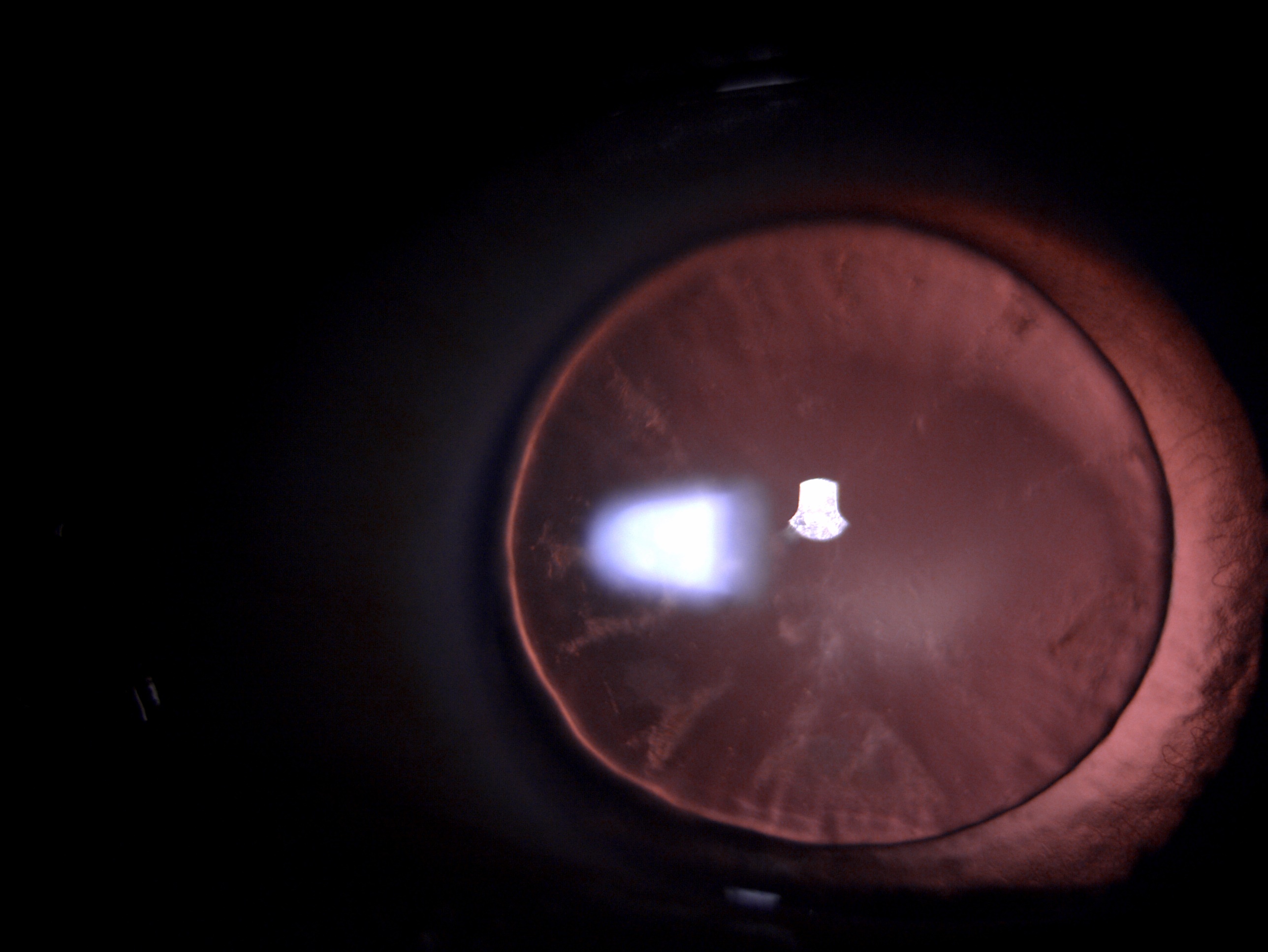
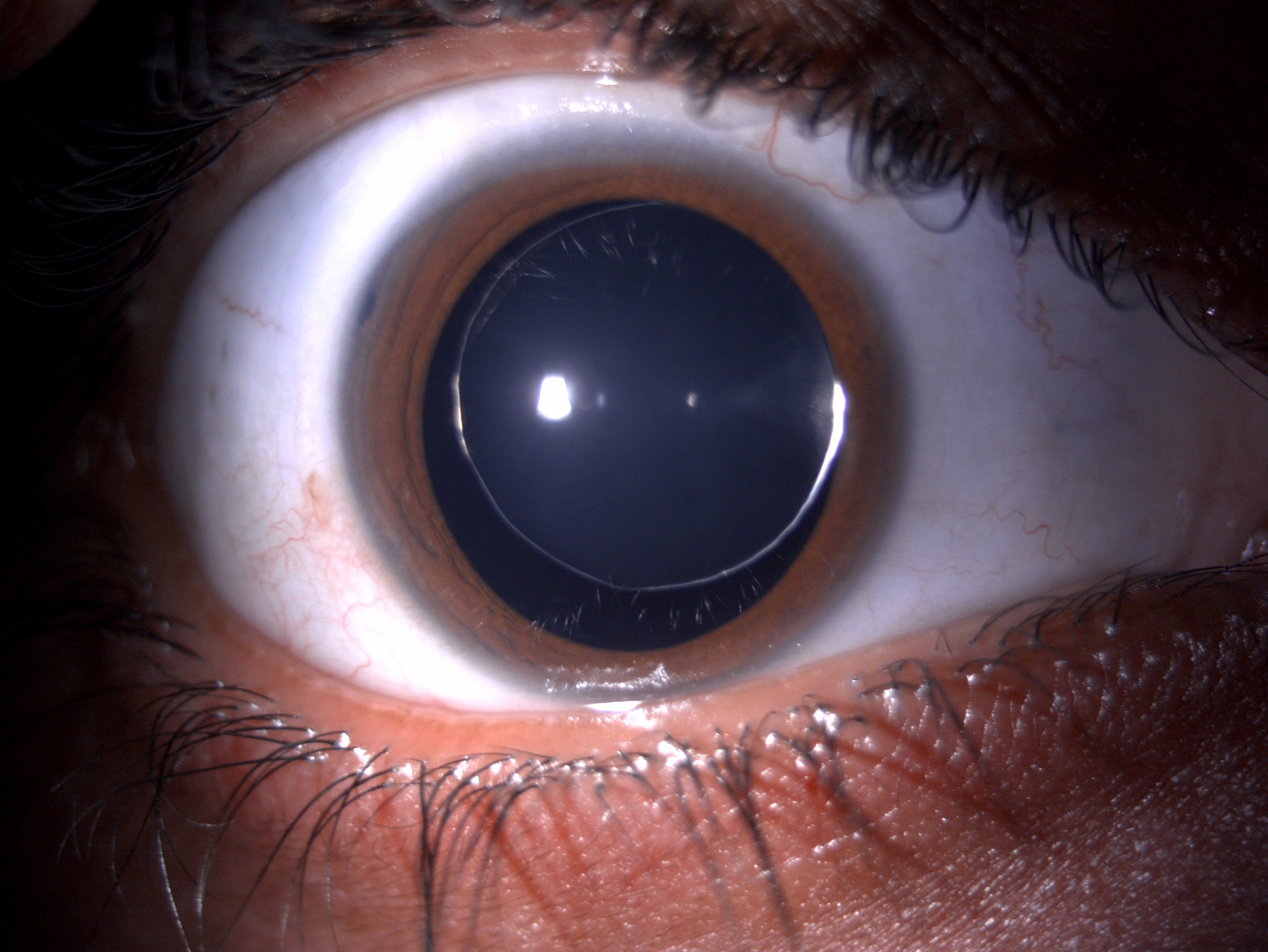
Microspherophakia is a rare congenital entity that is characterized by a bi-convex spherical lens with reduced equatorial diameter. This is primarily because of the developmental anomaly of zonules. The clinical manifestations can range from asymptomatic to high lenticular myopia, acute angle-closure, or chronic glaucoma. The diagnosis is based on meticulous and detailed clinical evaluation and dilated pupillary examination through which equatorial lens margins are easily visible. Anterior segment optical coherence tomography (ASOCT) or ultrasound biomicroscopy (UBM) also helps understand the lens curvature, thickness, or angle structures crowding owing to spherical lenticular shape. A high index of clinical suspicion, careful examination, regular follow-ups for correction of refractive error or planning surgical intervention, regular postoperative follow-ups, with monitoring of intraocular pressures and fundus for glaucomatous damage form the basis of successful management. This review describes the etiology, predisposing risk factors, variable clinical manifestations, investigations, imaging modalities, treatment protocols, and postoperative care of patients with microspherophakia by an interprofessional team.
Objectives:
- Describe the pathophysiology of microspherophakia.
- Outline the clinical investigations and role of imaging in microspherophakia.
- Summarize the management of patients with microspherophakia.
- Explain the possible ocular complications in patients with microspherophakia.
Introduction
Microspherophakia is a rare congenital anomaly characterized by the abnormal spherical shape of the crystalline lens. It is characterized by an increased anteroposterior thickness of the lens associated with reduced equatorial diameter.[1] The primary pathology lies in the development of zonules. The condition is often bilateral and is characterized by small, thick, and spherical lenses. Mutation in the LTBP2 gene is often implicated as the underlying pathology. The most common associations are lens subluxation, anterior or posterior dislocation, high myopia, accommodation deficits, or raised intraocular pressures.[2] Rare cases of microspherophakia associated with retinitis pigmentosa, Axenfeld Rieger anomaly, XYY syndrome have also been reported.[3][4][5]
Etiology
The underlying etiology lies in the development of zonules during embryogenesis. The genetic mutations in the latent TGF ?-binding protein-2 (LTBP2) gene, ADAMTS17, FBN1 genes have also been implicated. The LTBP2 gene is present in the trabecular meshwork, ciliary processes, and lens capsule and has structural homology with fibrillin protein. This gene is responsible for elastic fiber assembly. ADAMTS17 and FBN1 genes are the primary genes implicated in Weill Marchesani syndrome.[6][7]
Epidemiology
Microspherophakia is often present in association with different other developmental anomalies. This has also been well recognized as part of syndromic associations like Weil Marchesani syndrome. The prevalence for Weil Marchesani has been estimated at 1 in 100,000. Though isolated microspherophakia has been identified in different ethnic groups, its prevalence is not much studied. A study from India reported the prevalence of microspherophakia as 1.2% among children presenting with some lens abnormalities to the clinic.[8]
Pathophysiology
The crystalline lens is almost spherical at birth, with an anteroposterior thickness of 3.5 mm and an equatorial diameter of 6.5 mm. This increases to 5mm thickness and about 9 to 10 mm equatorial dimensions by adulthood. In the presence of weak zonules, there is a lack of tension at the equatorial plane, resulting in a more spherical and convex lens. This shape of the lens leads to high lenticular myopia and often subluxation because of weak zonules.
The two primary pathophysiological mechanisms implicated in microspherophakia are as follows:
- During the fifth to sixth decade of embryonic life, there can be a developmental delay or defective insertion of secondary lenticular fibers. This usually results from malnourishment and defects in tunica vasculosa lentis.
- Due to abnormal development of lenticular fibers, the zonules may become rudimentary, and the lens may remain spherical rather than normal biconvex shape.[1]
Histopathology
Histopathological analysis has revealed that the zonules can be rudimentary and unusually long. Moreover, there can be development defects and abnormal distribution of secondary lenticular fibers. Eventually, it can result in hyaloid degeneration because of changes in lenticular shape disrupting the lenticular fibers.
History and Physical
Microspherophakia is often a bilateral condition. The patients commonly present with complaints of low vision and defective accommodation. Rarely, the patient might complain of acute pain and redness with the presentation of acute angle closure.[9]
Occasionally, the patient will complain of uniocular diplopia due to lens subluxation. Rarely the child may present with flashes and floaters, and neglected cases may result in amblyopia. Fundoscopy may reveal signs of pathological myopia like a myopic disc, myopic crescent, posterior staphyloma, and myopic macular degeneration. The other signs can be blue sclera, ectopic pupil, retinal detachment, tears, retinal holes, or lattice degeneration.
In a study by Muralidhar et al., it was reported that all patients had different grades of lenticular myopia with a mean refractive error of -11.07 dioptres. Almost 45% developed glaucoma, and half of these had high intraocular pressures at the presentation itself. The chances of developing high intraocular pressures and angle-closure glaucoma are increased if the lens is displaced anteriorly. Microspherophakia may often be present as an isolated finding or might be associated with syndromes.[10] The most common systemic association reported was homocystinuria.[11]
There can be systemic as well as the local association. The systemic associations include Lowe syndrome, Marfan syndrome, Weill- Marchesani syndrome, Alport syndrome, microspherophakia-metaphyseal dysplasia, Cri du chat syndrome, Axenfield-Rieger syndrome, congenital rubella, Peter anomaly, hyperlysinaemia, Klinefelter syndrome, chondrodysplasia punctate, and metaphyseal dysplasia. The various local associations include aniridia, megalocornea, optic disc colobomata, and iridocorneal endothelial syndrome.[12]
Evaluation
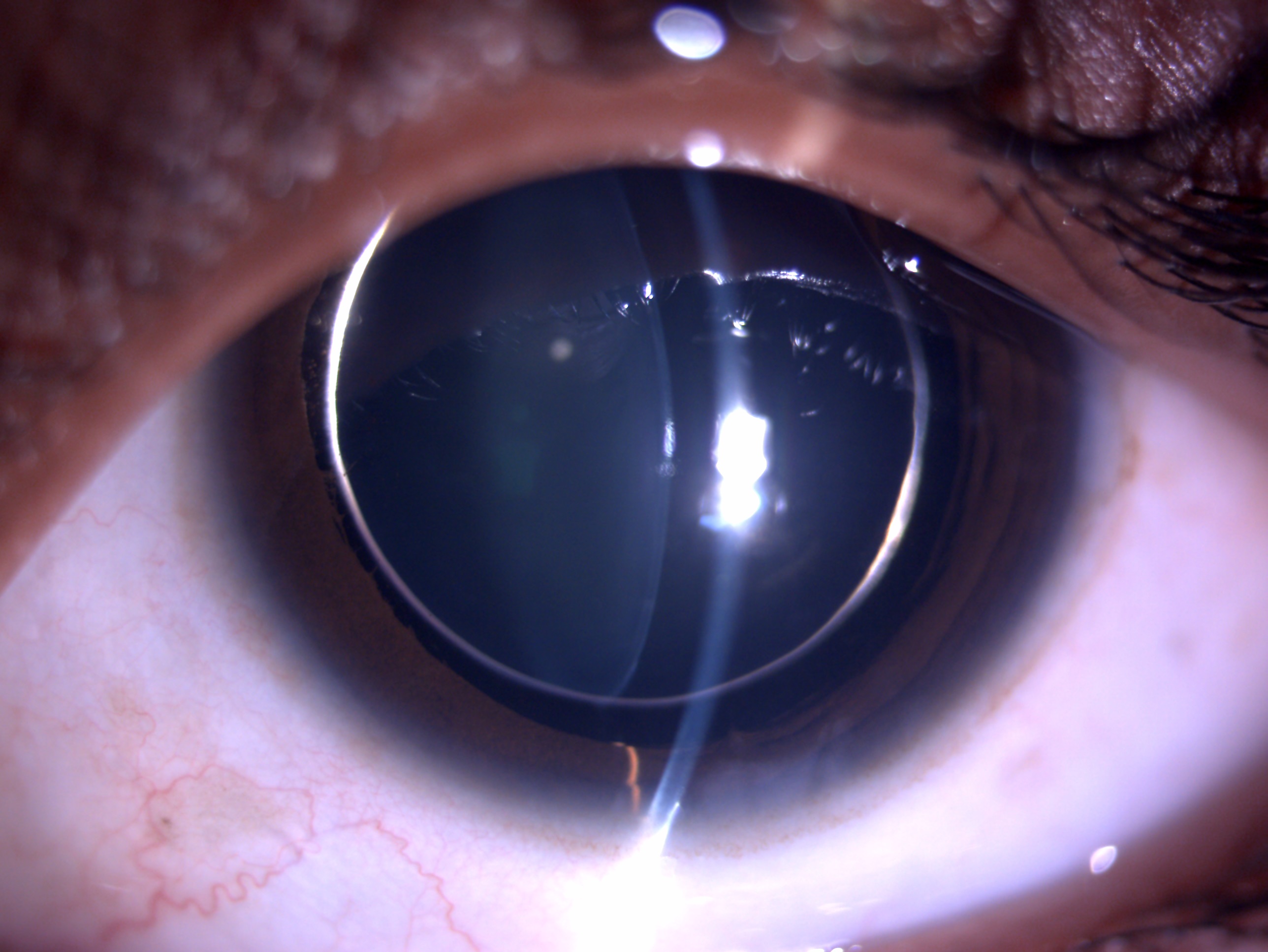
The ocular examination should include a detailed slit lamp examination. The important features to be looked at include retinoscopy, best-corrected visual acuity, intraocular pressure, anterior chamber angle and depth, gonioscopy, lens morphology, and signs of subluxation. Dilated fundus examination is needed to look for glaucomatous disc changes, myopic retinal changes, or coexisting retinal pathology. Gupta et al. reported an E sign for early recognition of microspherophakia cases clinically.[13]
Extra investigations might include lens thickness, axial length, ultrasound biomicroscopy, and anterior segment optical coherence tomography. These investigations might help understand the mechanism of angle closure in these patients. The role of iTrace has been described in analyzing the underlying cause of pre-operative reduced visual acuity and predicting postoperative outcomes.[14]
Often, patients might have reduced endothelial cell count, and electron microscopy might be needed before planning surgical intervention in these cases.[15] Apart from these, a detailed systemic examination is essential to rule out any syndromic features.
Treatment / Management
The specific management depends on the presenting features. Targeted management protocol includes
Lenticular Myopia
- All patients should be checked for underlying refractive errors. Timely refractive error correction helps in avoiding irreversible vision loss, thus preventing amblyopia. The patient should be followed up closely for any change in refractive error and appropriate correction.
Pupillary Block
- This is a common complication owing to the spherical shape of the lens. Pupillary block glaucoma is preventable by prophylactic Nd-Yag laser iridotomy. An acute attack can be controlled with the help of cycloplegics. Cycloplegics relax the ciliary muscles, thus tightening the zonules and pulling the lens iris diaphragm posteriorly. Intravenous mannitol also helps by causing the vitreous shrinkage and thus relieving the pupillary block.
Angle-Closure Glaucoma
- These patients might gain control of intraocular pressure following YAG iridotomy. Some patients might need additional antiglaucoma medications to control the intraocular pressure. Advanced cases might need glaucoma surgery in the form of a filtration procedure or glaucoma drainage device to attain further lower intraocular pressures and prevent additional damage to the disc.[16] Senthil et al. reported success rates of up to 86% till six months of follow-up following trabeculectomy.[12] Goel et al. reported successful management of two sisters with bilateral microspherophakia with advanced angle-closure glaucoma in the form of combined procedures including lensectomy, vitrectomy, and transversal ciliary body photocoagulation.[17]
Subluxated Lens
- The spherical lens with a smaller equatorial diameter and weak zonules is prone to anterior or posterior subluxation.[18] These cases might be planned for a precise lens extraction. IOL placement, if possible, should be targeted within the bag. Additionally, capsular tension rings or segments may be used by the surgeon if needed. Few novel modifications like the double-flanged technique in which capsulorhexis is performed using a femtosecond laser, followed by the standard capsular tension ring insertion, have been described to manage microspherophakia.[19] Clear lens extraction, goniosynechiolysis with or without secondary IOL in the form of scleral fixated intraocular lens implantation through anterior or pars plana route can be planned in patients with corneal-lenticular touch or posterior dislocation into the vitreous cavity.[15][20] Lens extraction alone might be planned in patients with high myopia. 25791701. The various indications of clear lens extraction in microspherophakia patients can be cornea-lenticular touch, high myopia in one eye, and pupillary block glaucoma.
Low Vision
- These patients often have low best-corrected visual acuity resulting from high lenticular myopia and refractive amblyopia, thus needing low vision assistive devices. Low vision in the form of reduced best-corrected visual acuity or restricted fields can also result from an advanced stage of glaucoma.
Systemic Conditions
- Evaluation by a physician to rule out any systemic associations is mandatory. These patients might need holistic management by ophthalmologists, optometrists, orthopedics, and a cardiologist.
Differential Diagnosis
The clinical conditions linked to microspherophakia include:
Ocular Associations
- Aniridia
- Megalocornea
- Iridocorneal endothelial syndrome
- High lenticular myopia
- Disc coloboma
- Retinal detachment[21]
Systemic Associations
- Alport syndrome[22]
- Weil Marchesani syndrome
- Homocystinuria
- Marfan syndrome
- Axenfeld-Rieger syndrome
- Metaphyseal dysplasia
Prognosis
Prognosis depends on the severity of the presentation. Senthil et al., in their study, found 51% of patients had glaucoma among eyes with microspherophakia. Success rates following trabeculectomy were reported as 86% following trabeculectomy till six months of follow up and 77% till one year. These results were the same till seven years of the follow-up period. Blindness was reported as high as in 20% of eyes at the time of presentation, and up to 30% of eyes till last follow up.[12]
Senthil et al., in another study, reported outcomes following trabeculectomy in 29 eyes of 18 patients with microspherophakia. They reported the probability of complete success in 96% at one year and 88% at two years of follow-up. These results were maintained till a follow-up period of 7 years.[23] Harasymowycz et al. reported trabeculectomy in one eye, which required lensectomy, vitrectomy with a scleral fixated intraocular lens, and Molteno tube shunt implant for the management of persistent flat anterior chamber following trabeculectomy.[24]
Another study by Garudadri et al. on 61 eyes with microspherophakia reported that 12 needed laser iridotomy and 40 eyes needed surgical intervention in the form of trabeculectomy, lensectomy, or drainage procedures. Twenty eyes (16%) were blind due to glaucoma.
Complications
Microspherophakia can be associated with complications secondary to the biconvex lens shape resulting in high myopia. Further, a relatively weak zonules lens is prone to subluxation or even complete anterior or posterior dislocation. The anterior subluxation can lead to corneo-lenticular touch, thus predisposing to endothelial cell loss or endothelial decompensation.
The posterior dislocation of the lens can lead to vitreous tractions and subsequent retinal detachment. Earlier studies have reported an incidence of up to 44% for subluxation of the lens in patients with microspherophakia. Further, the anterior subluxation of the lens can lead to a shallow anterior chamber, and pupillary block or patient might present with intermittent irido-lenticular touch.
The incidence of angle-closure glaucoma has been reported as high as 44.4 to 51%. Chronic pupillary block glaucoma can result from the formation of peripheral anterior synechiae, trabecular crowding by the spherophakic lens, reverse angle-closure glaucoma, or malignant glaucoma. Rarely, non-resolving malignant glaucoma might lead to permanent loss of vision or phthisis, or even there might be a painful blind eye needing enucleation.[25]
Postoperative and Rehabilitation Care
Postoperative care will include the use of short-term topical steroids, cycloplegics with or without antiglaucoma medications. The patient needs to be followed up for refractive error and corrected for residual refractive error or aphakic glasses. It is essential to monitor the intraocular pressure on every subsequent visit for at least six months. Patients with low best-corrected visual acuity or restricted fields from glaucomatous disc damage might need low vision assistive devices, and appropriate counseling regarding lifestyle modifications should be emphasized.
Consultations
Any child presenting to the outpatient department with complaints of defective vision, pain, and redness should be evaluated in detail to pinpoint the ocular pathology. All patients with a probable diagnosis of microspherophakia must be referred to a pediatric ophthalmologist for meticulous evaluation and targeted treatment to prevent irreversible vision-threatening sequalae and amblyopia.[26]
Deterrence and Patient Education
All patients must be educated regarding the need for regular follow-up. The patients should be explained the need to seek urgent health care if the patient develops acute redness/pain/colored haloes/sudden deterioration of vision. They should be stressed about the need for timely screening for refractive error, intraocular pressures and might need a change of glasses from time to time.
Surgical intervention might be planned as per the assessment on subsequent visits. Patient counseling is essential to understand that microspherophakia has an overall favorable prognosis, and good visual acuity can be achieved with timely intervention.
Pearls and Other Issues
Microspherophakia is a clinical diagnosis, and all patients with this pathology should be aggressively treated for an excellent visual outcome. A detailed systemic evaluation is mandatory in all cases to rule out syndromic associations. Special emphasis should be given to children to prevent amblyopia and secondary glaucoma.
Enhancing Healthcare Team Outcomes
Patients presenting with high myopia, acute angle-closure glaucoma, or spontaneously subluxated lenses should be examined carefully to rule out microspherophakia. Often, the optometrists might be the first ones to come in contact with these patients.
It is important to refer all high myopes presenting for the first time for evaluation to the ophthalmologist for detailed dilated anterior and posterior segment examination. The nursing team can help in explaining the need for regular follow-ups, preparing for any surgical intervention, and guiding the patients for postoperative medications and regular follow-up care. They also play a vital role in providing cross-referrals to low vision clinics and guiding patients for lifestyle modifications and overall psychological upliftment.
Assessment by a pediatrician or physician is necessary to rule out any systemic associations and manage the same. Thus, an interprofessional and holistic management approach can help achieve maximum success with optimal visual outcomes.