Continuing Education Activity
Two of the most prevalent diseases worldwide are type 2 diabetes mellitus (T2DM) and coronary artery disease. T2DM occurs when there is a decrease in insulin sensitivity, leading to higher amounts of glucose being present in the bloodstream. Coronary artery disease, or heart disease, develops over time as plaque builds up within the coronary arteries, causing a higher likelihood of developing myocardial infarction in the future. Though both of these conditions have specific disease processes, developing T2DM has been associated with a significantly higher incidence of developing coronary artery disease.
This activity delves into the global impact of these 2 diseases, emphasizing their interconnection and the heightened risk of coronary artery disease in individuals with T2DM. With a staggering prevalence and economic burden, affecting millions worldwide, these conditions demand proactive prevention strategies. This session reviews the management of T2DM and coronary artery disease, focusing on the pivotal role of an interprofessional healthcare team in mitigating risk factors and preventing these debilitating conditions. Participants will gain insights into the significance of lifestyle modifications in averting T2DM and heart disease, considering their substantial impact on morbidity, mortality, and economic burdens. Pharmacological interventions are also explored. Learners will be equipped with a comprehensive understanding of the global health implications of these conditions and practical insights into implementing effective preventative measures within an interprofessional framework.
Objectives:
Identify the connection between the prevalence of type 2 diabetes mellitus and cardiovascular disease and the associated cost burden.
Compare practical strategies for assisting patients in achieving dietary changes to help manage type 2 diabetes mellitus and cardiovascular disease.
Differentiate between various T2DM and cardiovascular disease prevention programs and their applications, emphasizing lifestyle modifications, pharmacological interventions, and community-based initiatives.
Collaborate with all members of the interprofessional team, including nutritionists, to educate, treat, and monitor patients with obesity and type 2 diabetes mellitus regarding the role of nutrition in preventing, treating, and reversing diabetes.
Issues of Concern
Prevention of T2DM
T2DM is a chronic condition characterized by the impairment of insulin secretion within the body and insulin resistance. It is estimated that T2DM now affects more than 8% of adults in the United States and is most prevalent among older adults, men, people with lower family incomes, lower educational levels, higher body mass indexes, and specific ethnic groups.[5] In addition to creating a personal and economic burden on the patient, T2DM can lead to several long-term complications, including retinopathy, nephropathy, and other vascular complications leading to amputations. Furthermore, patients with T2DM are more than twice as likely to develop cardiovascular disease and experience a stroke in their lifetime.[6][7]
Due to these complications and the increasing prevalence and incidence surrounding T2DM, preventing this disease process has become increasingly important.[8] Several methods that have been proven successful in preventing T2DM include lifestyle modifications such as weight loss, increased physical activity, and dietary changes.[8]
Weight Loss
Weight loss for the prevention of T2DM has shown to be an effective strategy as it has been found to improve insulin secretion; it has also been a suggested intervention for patients with T2DM who are overweight or obese. Evidence from several prominent studies has supported the notion that weight loss is associated with a decreased risk of developing T2DM.[7]
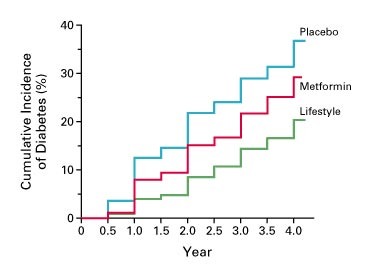
One such study is the Diabetes Prevention Program, one of the largest and most comprehensive lifestyle modification studies involving T2DM.[9] The program, described by Knowler et al. in 2002, randomly assigned 3,234 overweight adults with impaired glucose tolerance to either a lifestyle intervention, metformin, or a placebo group, with the lifestyle intervention arm aiming to have a reduction of 7% body weight in 24 weeks.[9]
For this intervention, participants were required to perform 150 minutes per week of moderate-intensity physical activity and were placed on a low-fat and calorie-reduced diet.[9] During this trial, participants lost an average of 7% body weight over 1 year, which was associated with a 58% reduction in the incidence of diabetes compared with the study's placebo arm.[9]
The study demonstrated that patients diagnosed with T2DM in the United States who were either overweight or obese could effectively reduce T2DM risk with weight loss, which was also found in Asian populations. Multiple studies assessing lifestyle modifications for the prevention of T2DM included participants with impaired glucose tolerance testing, and clear benefits were found by achieving a body mass index below 25.[9][10]
Physical Activity
Several studies have also determined that physical activity is crucial in preventing T2DM. A Finnish study called the Diabetes Prevention Study, which aimed to study the effects of lifestyle intervention as a method of preventing T2DM, randomly assigned 522 middle-aged adults who were in the overweight category and who had impaired glucose tolerance, to either an intervention group or a control group. The intervention group of the study included both diet and exercise, with the goal of 30 minutes or more of moderate-intensity exercise each day and a low-fat, low-dairy diet as methods of weight loss.[6]
Compared with the control group, the intervention group had a 58% reduction in T2DM incidence over 4 years and was reported to have an average weight loss of approximately 4.2 kg (9.25 lbs). Though this study was not designed to analyze the exercise components of individual participants, researchers found that those who participated in more vigorous physical activity during their leisure time during the study period had a more significant reduction in their risk of developing T2DM.[6]
The Diabetes Prevention Study describes how lifestyle modifications effectively reduce the risk of developing T2DM, and that individuals who can continue and even challenge themselves with physical activity can even further reduce the risk of developing T2DM. These findings are supported by the physiology surrounding glucose metabolism during physical activity, as physical activity causes an increased uptake of glucose into muscles as they are actively used.[11]
Furthermore, as muscle activity increases in intensity, there is a greater reliance on carbohydrates to fuel these active muscles, leading to lower fasting blood glucose for at least the first 24 hours after the individual has completed the exercise.[11] This consumption of carbohydrates by active muscle groups and the effect of lowering the fasting blood glucose after physical activity explains the results demonstrated by some of the participants of the Diabetes Prevention Study, who were deemed to have even more success by undergoing more physical activity in their leisure time, outside of the prescribed 30 minutes of daily moderate-intensity exercise.
Prevention of Cardiovascular Disease
T2DM is closely associated with other medical conditions, such as hypertension, obesity, and hypercholesterolemia, which together form portions of what is known as metabolic syndrome. Patients with metabolic syndrome are more likely to develop cardiovascular conditions and, therefore, have a higher mortality risk.[12]
As one of the leading causes of death in the United States, CVD prevention methods have been studied consistently over time.[13] Various studies have determined that the lifestyle factors that influence cardiovascular disease the most are an individual's diet, physical activity, and tobacco use.
Diet greatly influences the management and potential progression of CVD. Research has found that once coronary artery disease has been established, diet plays an integral role in furthering plaque deposition and influences endothelium reactivity, where both of these factors can largely predict cardiac events in the future. Prior evidence has determined that diets high in sodium, sugar-sweetened beverages, and meats positively correlate with cardiovascular morbidity and mortality.[13] This information analyzes specific diets to determine which dietary nutrients are best to prevent CVD and improve mortality.
Dietary Modifications
In addition to increasing physical activity (see below), dietary changes have been shown to benefit weight loss and the prevention of T2DM. Dietary modifications are an important aspect of diabetes prevention largely because they are associated with improved glycemic control.[14] In conjunction with increased physical activity, healthy dietary habits can increase weight loss, which has been proven an effective strategy for T2DM prevention. However, in terms of diets, specific types allow for better glycemic control. A systematic review that analyzed 48 articles regarding dietary modifications for T2DM prevention determined that diets such as the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet were both associated with significant T2DM incidence risk reductions.[14][15]
In this review article, the Mediterranean diet consisted of fish, seafood, fruits, nuts, vegetables, and legumes, with moderate alcohol consumption. The review, which analyzed 5 studies, determined that for T2DM incidence, there was a range from 9% risk reduction to 25% risk reduction, meaning that the incidence of T2DM was reduced within a range of 9 to 25% when this diet was initiated.[15] A large volume of literature details the Mediterranean diet's beneficial health effects.[13] The Lyon Diet Heart Study studied patients recovering from a myocardial infarction and reported a nearly 70% reduction in further cardiovascular events when switching to the Mediterranean diet, but a Cochran review suggested that the findings are controversial and not entirely supported by the evidence.[16]
The other diet that has been recommended is the DASH diet, which is defined as 10 total food groups and was developed to target hypertensive patients.[15] It requires 4 or more cups of fruits and vegetables each day, low-fat dairy products, 3 ounces of whole grains each day, 7 ounces total of fish per week, less than 1500 mg of sodium each day, and less than 450 calories of sugar-sweetened beverages each week. A meta-analysis of 6 studies that used the DASH diet determined that the risk of coronary artery disease was reduced by 21%, and the risk of stroke was also reduced by 21%, demonstrating that the DASH diet has the potential to improve the risk of developing these 2 conditions significantly.[17] Recent trials have demonstrated beneficial effects on blood pressure and improvements in other cardiovascular risk factors; and although the DASH diet was initially targeted toward patients with hypertension, a meta-analysis of various studies using it has determined that patients following it had a 20% risk reduction for developing T2DM.[18]
Overall, vegetarian diets of various types are associated with a lower prevalence of diabetes. A subset of the Adventist Health Study-2, which included over 60,000 subjects, showed a lower prevalence of T2DM in vegetarians than nonvegetarians. Vegans (2.9%), ovo-lacto (3.2%), pesco (4.8%), and semi (6.1%) all had a lower prevalence than nonvegetarians (7.6%).[19]
Physical Activity
Physical activity, as it has been studied for cardiovascular health benefits, is defined as the movement by skeletal muscle that causes an increase in energy expenditure compared to rest. Decreasing cardiac disease risk factors is important for patients with T2DM. Physical activity has been shown to improve cardiovascular risk factors, such as hypertension, coronary artery calcium, and lipids, and has been associated with a reduced risk of coronary artery disease or heart failure.[13]
A meta-analysis and review completed in 2016, which was based on cardiac rehabilitation programs, determined that the relative risk for cardiovascular mortality and hospitalization in these programs was 0.74 and 0.82, respectively. Another meta-analysis of 44 randomized controlled trials showed that aerobic exercise reduced blood pressure in both normotensive and hypertensive individuals. As these and various other studies have demonstrated, there is significant evidence of the benefit of physical activity. Consequently, the American Heart Association recommends a minimum of 30 minutes of moderate-to-intense exercise at least 5 days out of the week.[13]
Tobacco Cessation
Tobacco has long been associated with cardiovascular deaths, and it has been estimated that up to 10% of cardiovascular deaths worldwide in adults aged 30 years or older can be attributed to tobacco use. Tobacco smoke itself contains approximately 98 components that are hazardous when inhaled.[13] Evidence suggests that it causes endothelial cell dysfunction, increases lipid oxidation, and activates both pro-inflammatory and procoagulation states. A meta-analysis completed in 2021 analyzed 9 studies that compared tobacco users and cardiovascular disease and stroke. It was found that smoking cessation was associated with significantly lowered mortality from cardiovascular disease, despite some postcessation weight gain.[20]
In conclusion, lifestyle modifications for both T2DM and coronary artery disease do overlap in terms of dietary changes and increasing physical activity. Both the DASH and Mediterranean diets have shown positive evidence of reducing the incidence of both T2DM and coronary artery disease. Additionally, physical activity in the form of moderate-to-intense exercise (~30 minutes, 5 days per week) reduces the risk of developing both T2DM and coronary artery disease. Weight loss has specifically been shown to reduce the incidence of T2DM as it reduces insulin resistance, whereas tobacco cessation has been correlated with a reduction in coronary artery disease risk as it decreases pro-inflammatory and endothelial injury.[6][13]
Clinical Significance
T2DM and cardiovascular disease are 2 of the most common chronic health conditions, leading to significant mortality rates and financial burdens. The various lifestyle modifications indicate changes that patients can make in their daily lives and allow patients to feel empowered to take control of their medical conditions.
Patients diagnosed with T2DM are more at risk for developing microvascular disease, a sequela of this condition. However, weight loss through diet and physical activity has been shown to significantly reduce the incidence of diabetes, reducing the patient’s chance of developing nephropathy, retinopathy, and neuropathy.[6]
In patients diagnosed with T2DM, reducing the severity of diabetes and preventing its sequela ultimately increases the patient’s quality of life and long-term health. Overall, these preventative methods aim to reduce the incidence of T2DM, which would significantly reduce chronic disease and prevent patients from experiencing the hardships associated with diabetes, both in terms of health and finances.[6][21]
Cardiovascular disease is closely associated with T2DM as the pathophysiology behind T2DM induces changes in vessels that lead to a greater likelihood of developing both of these comorbid conditions.[12] Like T2DM, patients diagnosed with cardiovascular disease will have the ability to improve their risk of worsening or progressive disease through dietary changes, physical activity, and tobacco cessation.[13]
Dietary changes, such as certain vegetarian diets, the Mediterranean diet, or incorporating the DASH diet, have been shown to reduce the risk of cardiovascular events and allow patients to make these changes themselves.[13][17] Tobacco cessation is a key lifestyle modification that allows patients to improve their cardiovascular risk, reduce their risk of developing chronic lung conditions, and enhance their overall quality of life.[13][20]
These preventative methods allow patients to control their medical conditions more than medications, surgical interventions, or procedures. Some changes can be made in the patient’s home environment that significantly impact the progression of their disease process and the sequela surrounding the conditions.
Enhancing Healthcare Team Outcomes
T2DM and coronary artery disease are some of the leading causes of mortality in the United States and globally. T2DM is a condition in which impaired insulin secretion increases blood glucose[6]. Significant evidence demonstrates that patients diagnosed with T2DM are more likely to develop coronary artery disease. However, there are multiple prevention methods, and as healthcare professionals, it is essential to provide patients with accurate information regarding preventing these chronic conditions.
One of the most influential studies completed regarding T2DM prevention with the prevention strategy of weight loss was the Diabetes Prevention Study, which randomly assigned over 3,000 overweight adults with impaired glucose tolerance to groups to either receive placebo, metformin, or join the lifestyle interventional group.[6]
It was found that a lifestyle intervention consisting of a low-calorie, low-fat diet, and moderate-intensity exercise for 150 minutes each week reduced the risk of developing T2DM by 67% in patients in the lifestyle intervention group. This study showed that patients could participate in prevention methods and significantly reduce risk.
Clinicians are responsible for informing patients about their risk of developing T2DM and prevention methods, as well as how these methods would impact their long-term health. Other health professionals, especially nurses, nurse practitioners, and physician assistants, are responsible for sharing this information and working with patients on these lifestyle changes.
Coronary artery disease is a comorbid condition that poses life-threatening consequences of disease sequelae; like T2DM, it is a condition that can be managed with prevention methods. Specifically, the Lyon Diet Heart Study demonstrated that patients who have experienced a myocardial infarction in the past had a 70% reduction in risk after starting the Mediterranean diet.[13]
Thus, prevention strategies involving dietary changes should be communicated to patients at higher risk of developing this comorbidity. Physicians should be educated in the physiology behind preventative methods to recommend the best patient strategies. Other health professionals should also be aware of these so they can educate and provide the best care for patients.
T2DM and coronary artery disease are associated with some of the highest mortalities. However, preventative strategies have been extensively studied and have demonstrated significant risk reductions in these conditions. Health professionals should be well informed regarding the benefits of these prevention methods to improve patient outcomes.