[1]
Katz S, Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society. 1983 Dec;
[PubMed PMID: 6418786]
[2]
Bieńkiewicz MM,Brandi ML,Goldenberg G,Hughes CM,Hermsdörfer J, The tool in the brain: apraxia in ADL. Behavioral and neurological correlates of apraxia in daily living. Frontiers in psychology. 2014;
[PubMed PMID: 24795685]
[3]
Guidet B,de Lange DW,Boumendil A,Leaver S,Watson X,Boulanger C,Szczeklik W,Artigas A,Morandi A,Andersen F,Zafeiridis T,Jung C,Moreno R,Walther S,Oeyen S,Schefold JC,Cecconi M,Marsh B,Joannidis M,Nalapko Y,Elhadi M,Fjølner J,Flaatten H, The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive care medicine. 2019 Nov 29;
[PubMed PMID: 31784798]
[4]
Costenoble A,Knoop V,Vermeiren S,Vella RA,Debain A,Rossi G,Bautmans I,Verté D,Gorus E,De Vriendt P, A Comprehensive Overview of Activities of Daily Living in Existing Frailty Instruments: A Systematic Literature Search. The Gerontologist. 2019 Dec 17;
[PubMed PMID: 31872238]
Level 3 (low-level) evidence
[5]
Cagle JG, Lee J, Ornstein KA, Guralnik JM. Hospice Utilization in the United States: A Prospective Cohort Study Comparing Cancer and Noncancer Deaths. Journal of the American Geriatrics Society. 2020 Apr:68(4):783-793. doi: 10.1111/jgs.16294. Epub 2019 Dec 27
[PubMed PMID: 31880312]
[6]
Rosenberg T, Montgomery P, Hay V, Lattimer R. Using frailty and quality of life measures in clinical care of the elderly in Canada to predict death, nursing home transfer and hospitalisation - the frailty and ageing cohort study. BMJ open. 2019 Nov 12:9(11):e032712. doi: 10.1136/bmjopen-2019-032712. Epub 2019 Nov 12
[PubMed PMID: 31722953]
Level 2 (mid-level) evidence
[7]
Wolff JL, Feder J, Schulz R. Supporting Family Caregivers of Older Americans. The New England journal of medicine. 2016 Dec 29:375(26):2513-2515. doi: 10.1056/NEJMp1612351. Epub
[PubMed PMID: 28029922]
[8]
Adams PF, Kirzinger WK, Martinez ME. Summary health statistics for the u.s. Population: national health interview survey, 2011. Vital and health statistics. Series 10, Data from the National Health Survey. 2012 Dec:(255):1-110
[PubMed PMID: 25116371]
Level 3 (low-level) evidence
[9]
Cahn-Weiner DA, Boyle PA, Malloy PF. Tests of executive function predict instrumental activities of daily living in community-dwelling older individuals. Applied neuropsychology. 2002:9(3):187-91
[PubMed PMID: 12584085]
[10]
Delirium is prevalent in older hospital inpatients and associated with adverse outcomes: results of a prospective multi-centre study on World Delirium Awareness Day. BMC medicine. 2019 Dec 14;
[PubMed PMID: 31837711]
[11]
Farias ST,Park LQ,Harvey DJ,Simon C,Reed BR,Carmichael O,Mungas D, Everyday cognition in older adults: associations with neuropsychological performance and structural brain imaging. Journal of the International Neuropsychological Society : JINS. 2013 Apr;
[PubMed PMID: 23369894]
[12]
Farias ST, Harrell E, Neumann C, Houtz A. The relationship between neuropsychological performance and daily functioning in individuals with Alzheimer's disease: ecological validity of neuropsychological tests. Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists. 2003 Aug:18(6):655-72
[PubMed PMID: 14591439]
Level 2 (mid-level) evidence
[13]
Chu NM, Sison S, Muzaale AD, Haugen CE, Garonzik-Wang JM, Brennan DC, Norman SP, Segev DL, McAdams-DeMarco M. Functional independence, access to kidney transplantation and waitlist mortality. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2020 May 1:35(5):870-877. doi: 10.1093/ndt/gfz265. Epub
[PubMed PMID: 31860087]
[14]
Desai AK, Grossberg GT, Sheth DN. Activities of daily living in patients with dementia: clinical relevance, methods of assessment and effects of treatment. CNS drugs. 2004:18(13):853-75
[PubMed PMID: 15521790]
[15]
Fields JA,Machulda M,Aakre J,Ivnik RJ,Boeve BF,Knopman DS,Petersen RC,Smith GE, Utility of the DRS for predicting problems in day-to-day functioning. The Clinical neuropsychologist. 2010 Oct;
[PubMed PMID: 20924981]
[16]
Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. The Gerontologist. 1970 Spring:10(1):20-30
[PubMed PMID: 5420677]
[17]
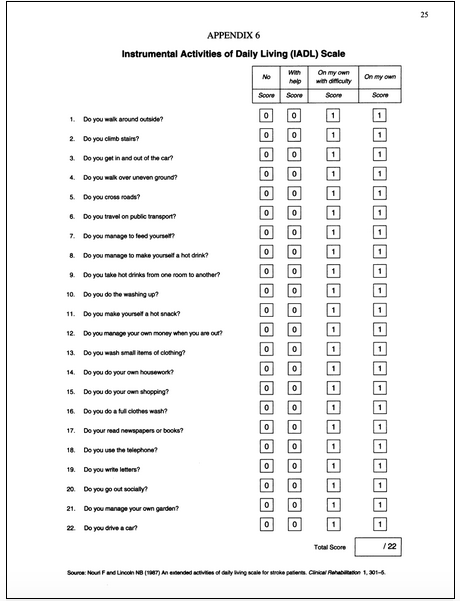
Graf C. The Lawton Instrumental Activities of Daily Living (IADL) Scale. Medsurg nursing : official journal of the Academy of Medical-Surgical Nurses. 2009 Sep-Oct:18(5):315-6
[PubMed PMID: 19927971]
[18]
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969 Autumn:9(3):179-86
[PubMed PMID: 5349366]
[19]
Wong MM, Pang PF. Factors Associated with Falls in Psychogeriatric Inpatients and Comparison of Two Fall Risk Assessment Tools. East Asian archives of psychiatry : official journal of the Hong Kong College of Psychiatrists = Dong Ya jing shen ke xue zhi : Xianggang jing shen ke yi xue yuan qi kan. 2019 Mar:29(1):10-14
[PubMed PMID: 31237251]
Level 2 (mid-level) evidence
[20]
Vaughan L,Leng X,La Monte MJ,Tindle HA,Cochrane BB,Shumaker SA, Functional Independence in Late-Life: Maintaining Physical Functioning in Older Adulthood Predicts Daily Life Function after Age 80. The journals of gerontology. Series A, Biological sciences and medical sciences. 2016 Mar;
[PubMed PMID: 26858328]
[21]
Warmoth K, Tarrant M, Abraham C, Lang IA. Relationship between perceptions of ageing and frailty in English older adults. Psychology, health & medicine. 2018 Apr:23(4):465-474. doi: 10.1080/13548506.2017.1349325. Epub 2017 Jul 4
[PubMed PMID: 28675053]
[22]
Damukaitis C,Schirm V, Program planning for long-term care: meeting the demand for nursing services. Nursing homes and senior citizen care. 1989 Nov
[PubMed PMID: 10296792]
[23]
Gorges RJ, Sanghavi P, Konetzka RT. A National Examination Of Long-Term Care Setting, Outcomes, And Disparities Among Elderly Dual Eligibles. Health affairs (Project Hope). 2019 Jul:38(7):1110-1118. doi: 10.1377/hlthaff.2018.05409. Epub
[PubMed PMID: 31260370]
[24]
Abrahamson K,Hass Z,Arling G, Shall I Stay or Shall I Go? The Choice to Remain in the Nursing Home Among Residents With High Potential for Discharge. Journal of applied gerontology : the official journal of the Southern Gerontological Society. 2018 Oct 26;
[PubMed PMID: 30366510]
[25]
Wang J,Caprio TV,Simning A,Shang J,Conwell Y,Yu F,Li Y, Association Between Home Health Services and Facility Admission in Older Adults With and Without Alzheimer's Disease. Journal of the American Medical Directors Association. 2019 Dec 23;
[PubMed PMID: 31879184]
[26]
Fong JH, Mitchell OS, Koh BS. Disaggregating activities of daily living limitations for predicting nursing home admission. Health services research. 2015 Apr:50(2):560-78. doi: 10.1111/1475-6773.12235. Epub 2014 Sep 26
[PubMed PMID: 25256014]