Continuing Education Activity
Transconjunctival blepharoplasty is usually used for cosmetic improvement of the lower eyelid or reconstructive surgery. There is no skin incision involved in addressing the deeper structures of ligaments, orbital fat, and orbital septum in this procedure. This activity reviews the indications, contraindications, and complications associated with a transconjunctival blepharoplasty. This activity highlights the role of the interprofessional team in the care of patients undergoing this procedure.
Objectives:
- Identify the indications for transconjunctival blepharoplasty.
- Describe the technique involved in performing transconjunctival blepharoplasty.
- Review the complications of transconjunctival blepharoplasty.
- Explain interprofessional team strategies for enhancing care coordination and communication to advance the management of patients undergoing transconjunctival blepharoplasty.
Introduction
Transconjunctival blepharoplasty is the management of lower eyelid structures via the conjunctival approach and is usually applied to the cosmetic improvement of the lower eyelid using this approach.[1][2] The transconjunctival approach is often also used for reconstructive surgery. The very essence of this surgical procedure implies that there is no skin incision made when addressing the deeper structures of orbital fat, ligaments, and orbital septum. However, there are times when some degree of skin and tendon manipulation will be necessary during the transconjunctival blepharoplasty. We will discuss the reasons for specific manipulations in the transconjunctival blepharoplasty.[3]
Types of Transconjunctival Blepharoplasty
- Pure transconjunctival blepharoplasty
- Transconjunctival blepharoplasty with lateral canthal tightening with a canthopexy or canthoplasty
- Transconjunctival blepharoplasty with lateral canthal tightening and skin pinch excision
- Transconjunctival blepharoplasty with the release of the orbitomalar ligament and fat transposition or grafting, lateral canthal tightening, with or without skin excision
- Transconjunctival blepharoplasty with skin-muscle flap (infrequently performed now, but there are exceptional cases where this approach is indicated)
- Transconjunctival blepharoplasty with midfacial tissue repositioning via a temporal incision (what we have designed and termed the "hammock lift").
In all of the above procedures, chemical peels, erbium or CO2 laser, broadband light therapy, or any other skin ablation modality may improve skin laxity, irregularities, wrinkles, and lesions.
This article will concentrate on the indications, assessment, marking, and performing the pure transconjunctival blepharoplasty.
Anatomy and Physiology
A detailed discussion of lower eyelid anatomy is available elsewhere, but the focus is on the important structures that apply when performing the transconjunctival blepharoplasty.
Normal Lower Eyelid Position
The lower eyelid position is at or just above the inferior limbus. The eyelid sits snug against the globe. This position results from normal anatomical and physiological factors: the medial and lateral canthal tendon integrity, normal orbicularis tone and attachments, normal pliable skin, and a normal tarsal plate. If there is a disruption of any of these structures, lower eyelid retraction, canthal dystopia, or ectropion may occur. Furthermore, even if these structures are normal, any excessive distracting, downward force can cause lower eyelid malposition. With scarring or shortage of the lower eyelid skin, an ectropion or retraction may occur. Middle lamellar scarring (involving the orbital septum and retractors) can result in lower eyelid retraction. Scarring or loss of part of the tarsus can result in an ectropion or entropion. Injury to the facial nerve or orbicularis muscle can result in lower lid ectropion and retraction, and disruption of the medial or lateral canthal tendons can similarly cause a lower eyelid malposition.
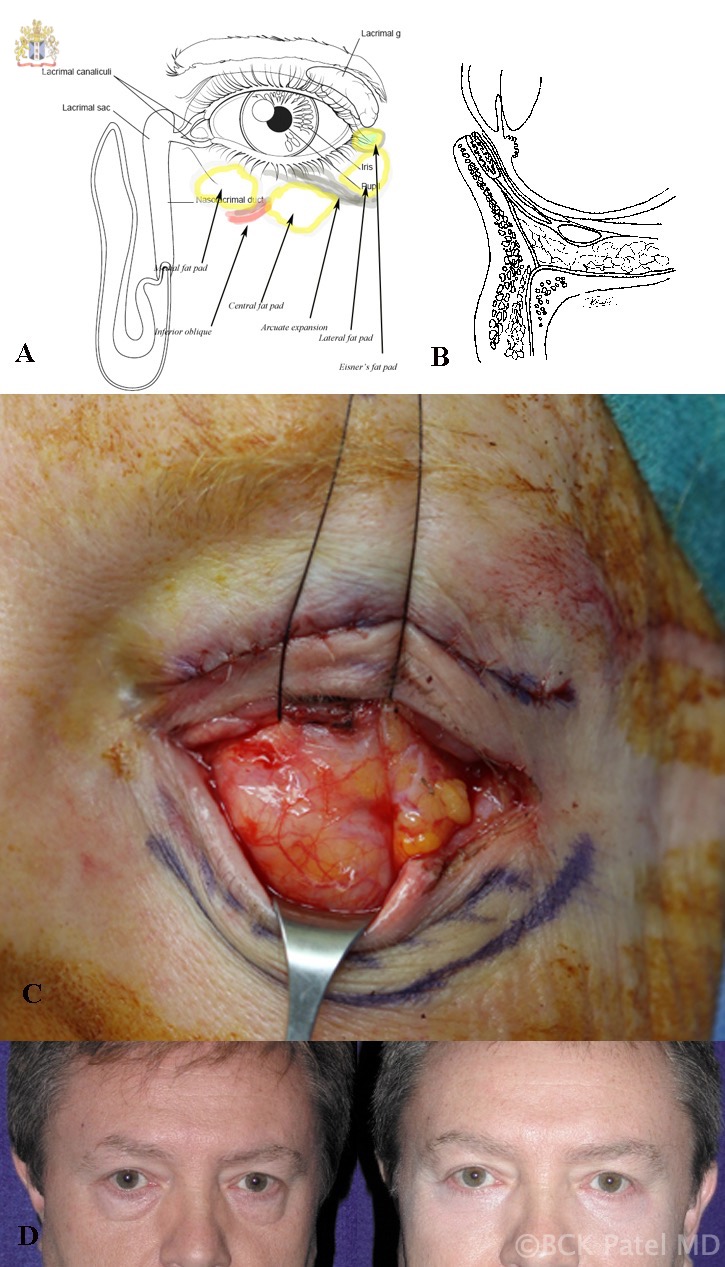
Applied Anatomy
The lower eyelid is supported medially by the medial canthal tendon and laterally by the lateral canthal tendon. At the tarsal plate level, the eyelid has a bi-lamellar structure with an anterior lamella of skin and orbicularis muscle with a suborbicularis fascial plane with minimal fat. The posterior lamella comprises the tarsus (which measures 1 mm in thickness and 5 to 6 mm in height) and conjunctiva. Below the level of the tarsal plate, the eyelid may be considered as having a tri-lamella structure with anterior lamella consisting of skin and orbicularis oculi muscle, the middle lamella comprising of the orbital septum, and to a degree, the lower eyelid retractors (called the capsulopalpebral fascia) with fat interposed between the septum and the retractors. At the orbital rim, the orbital septum fuses with the periosteum creating what is called the arcus marginalis. The posterior lamella may be considered as consisting of, to a degree, the lower eyelid retractors and the conjunctiva. The lower eyelid retractors are analogous to the upper eyelid retractors (levator palpebrae superioris and its aponeurosis): the lower lid retractors arise from the inferior rectus muscle, envelope the inferior oblique muscle, and proceed to insert into the inferior border of the tarsal plate and orbital septum. Like the levator palpebrae, the lower lid retractors are supplied by the oculomotor nerve. The equivalent of Muller's muscle (innervated by the sympathetic fibers originating from the carotid plexus) is a less defined muscle present just behind the capsulopalpebral fascia, often called the inferior tarsal smooth muscle. Similar to the Whitnall's ligament in the upper eyelid, Lockwood's ligament (the suspensory ligamentous sling supporting the globe) is attached laterally to the Whitnall's tubercle and inferolateral orbital rim and medially to the inferomedial orbital rim. Analogous to the upper eyelid post-levator aponeurosis fat pad, the lower eyelid has two additional thin layers of fat, the inter-lower eyelid retractor fat pad lying between the two layers of the lower eyelid retractors and the post-lower eyelid retractor fat pad lying between this and the conjunctiva. Whitnall’s tubercle is 3 to 4 mm inside the orbital rim and just above the horizontal axis. Into this tubercle, insert several structures: lateral canthal tendon, orbital septum, Lockwood’s ligament, Whitnall’s ligament, the deep head of orbicularis muscle, and the check ligaments of the lateral rectus muscle.
Orbital Septum
The orbital septum attaches at the orbital rim, except inferolaterally, where it inserts anteriorly, forming a recess (of Eisler). Therefore, the lateral orbital fat drapes over the inferolateral orbital rim into this recess, and this portion of the fat may be missed in the resection. The orbital septum attaches to the inferior border of the tarsal plate. The septum is thinnest over the medial fat pad. It has a thickening, which goes inferolaterally called the arcuate expansion, which separates the central and lateral fat pockets. The thought is that the purpose of this dense arcuate expansion is to retain the fat within the orbit.
Orbital Fat
The inferior oblique muscle separates the medial and central fat pads. However, there is usually an isthmus of fat over the inferior oblique belonging to one or both of these fat pads so during surgery, if one wants to see the inferior oblique muscle, one has to tease this fat off the inferior oblique muscle. The central and lateral fat pads are separated by the arcuate expansion, a thickening in the orbital septum.
Indications
Transconjunctival blepharoplasty is undertaken to improve the appearance of lower eyelids. Specifically, it aims to reduce or efface the bulges created by the medial, central, and lateral fat pads. In its purest form, the procedure is indicated in the younger patients who have isolated prominence of these fat pads without significant lower eyelid laxity, without skin or orbicularis redundancy, and without festoons. The patient should not have significant nasojugal or malar grooves or cheek ptosis.
There is no functional improvement obtained with a transconjunctival blepharoplasty in the majority of patients. An exception is an occasional patient who has such prominent steatoblepharon that it obstructs their inferior visual fields or whose spectacles cannot sit in the correct position because of the prominent eyelid fat pads. In such cases, functional lower blepharoplasty is indicated.
Contraindications
Contraindications to a pure transconjunctival blepharoplasty exist if any of these are present:
- Skin excess
- Poor lower eyelid skin tone or excessive solar elastosis
- Orbicularis redundancy or hypertrophy
- Festoons
- Lower eyelid laxity
- Floppy eyelid syndrome
- Ectropion
- Lower eyelid retraction
- Lateral canthal dystopia
- Significant orbital groove (composed of the nasojugal groove and malar groove)
- Significant cheek ptosis
Relative contraindications include:
- Proptosis
- Negative malar angle
Equipment
Within a "Plastics" surgical instrument set, the following instruments are specifically necessary for the reasons stated:
- A small Desmarres retractor and a four-pronged blunt-tipped rake for lower eyelid retraction: wide retractors limit the surgical view - the rake tips are blunt to avoid unnecessary trauma when retracting
- An electrocautery unit with a sharp tip cutting needle is reasonable to use. Alternative devices include a radio-frequency device with a cutting needle, although this gives less hemostasis than an electrocautery unit (which, in turn, leads to more collateral heat)
- Many practitioners prefer to make incisions with Westcott scissors, dissect the fat with Stevens or Westcott scissors, and use bipolar cautery during the procedure, rather than the monopolar unit.
- A 4-0 silk suture to provide traction to the conjunctiva to aid exposure
- Q-tips for delicate dabbing to control small bleeders
- Bipolar cautery
- Frozen gauze or sterile ice packs for use during surgery
- A plastic corneal shield should be used to protect the cornea during eyelid surgery.
Personnel
Transconjunctival blepharoplasty is generally performed under sedation in a surgical theatre. Although the procedure may be performed under local anesthesia in the surgical office, many practitioners choose to have proper suction, lighting, cautery, and sedation anesthesia to allow the surgeon to concentrate on the procedure. A good assistant is also vital to allow adequate exposure to the surgical field.
Preparation
Preoperative Assessment
Every patient should have a vision examination before surgery. Basic assessment of the tear film, for evidence of lid margin and meibomian disease, is imperative.
When assessing any cosmetic patient, it is important to ask exactly what improvement the patient wishes to see. This can be done with the patient looking into a mirror and, where necessary, with the help of a clinical photograph on a big screen. Younger photographs are reviewed, as are previous surgical procedures. As chemosis is one of the commonest complications of transconjunctival blepharoplasty, the patient should have an examination for evidence of conjunctival solar damage and conjunctivochalasis.
Sequential Assessment Performance
Skin
The eyelid and surrounding skin are examined for effects of sun exposure, rhytids, laxity, and festoons. The skin turgor and tone undergo assessment, as are any vessels, pigmented lesions, or evidence of chronic edema. A history of use of continuous positive airway pressure (CPAP) machines is taken on every patient as this predisposes patients to malar edema. Preoperative evidence of malar edema (with or without festoons) is a predictor of almost certain postoperative fluid and swelling in this region. Skin redundancy is assessed by the patient looking up and pinching the skin; then, the patient opens their mouth at the same time, and the pinch test is repeated. These are all subjective tests that have to consider any midfacial ptosis, solar elastosis, globe position, and prior surgery.
Lower Eyelid Position
The lower eyelid position should be at or just above the inferior corneal limbus. This position varies racially and depends upon the position of the globe (relative enophthalmos or exophthalmos). The position of the lower eyelid margin in relation to the limbus should be measured and documented as an inferior scleral show in millimeters if the lower eyelid is retracted. Causes of lower eyelid retraction include prior lower eyelid surgery or trauma, thyroid disease, solar elastosis, relative proptosis, and certain cicatrizing diseases like chemical burns, pemphigoid, and Stevens-Johnson syndrome.
Tests for Lower Eyelid Laxity
- The distraction test is performed by pulling the lower eyelid away from the globe with a finger. The distraction of the lid away from the globe increases with age, but a distraction of more than 6 mm is considered abnormal; this can be due to lateral canthal laxity, medial canthal laxity, or lower eyelid tarsal redundancy as may be seen in the floppy eyelid syndrome.
- The snapback test is next performed by pulling the lower eyelid away from the globe and releasing it. The eyelid should "snap" back to the globe without delay. A slow return to the globe or if the patient has to blink to allow the eyelid to oppose the globe, eludes to the presence of lower eyelid laxity. A weak snapback is present if there is facial nerve weakness; if there is orbicularis weakness, there is a cicatricial component to the anterior lamella and also in the presence of lateral and medial canthal laxity. The snapback test is always abnormal in patients with floppy eyelid syndrome.
- The gape test is not well-known, especially in general plastic surgery, and bears discussing. With normal eyelid tone, the lower eyelids move upwards in upgaze, and even with the mouth open, the lid stays snug with the globe. An increase in the scleral show on looking up or opening the mouth is a sign of lower lid laxity or retraction. If the lid stays snug with the eye with upgaze, it is graded "0," which is normal. If the lid moves away from the globe with upgaze, it is a grade "3", and if it only moves away with upgaze and opening the mouth, it is a grade "2". A grade "1" is if the lid only stays away with upgaze, mouth opening, and pulling the lid down and releasing it. This maneuver allows the surgeon to plan the best surgical approach.
- Medial canthal tendon laxity: the movement of the punctum is measured with the lower lid being pulled laterally with a finger. The punctum is used to measure the degree of lateral movement. The normal movement should be 2 to 4 mm. However, movement of the punctum beyond the medial corneal limbus (with the patient looking straight ahead) reveals medial canthal tendon laxity.
- Lateral canthal tendon laxity: similarly, the lateral canthus should move less than 2 mm when pulling the lid medially.
- Punctal eversion and stenosis: this is best noted under biomicroscopic examination. It indicates laxity with or without anterior lamellar cicatrization.
- Every eyelid procedure should have their MRD-1 (the distance between the corneal reflex and upper lid margin, where the normal is 3 to 4 mm) and MRD- 2 (the distance between the corneal reflex and the lower lid margin, where the normal distance is 3 to 5 mm) measured.
Lateral Canthus
The lateral canthal tendon insertion is 2 mm above that of the medial canthal tendon. In the presence of lateral canthal laxity, this lateral canthal attachment of the canthal tendon stretches (or detaches in extreme cases), and the lateral canthal position is then at the same position or lower than the medial canthal tendon. The normal distance between the lateral eyelid commissure and the lateral orbital wall is 2 to 3 mm in an adult. Any increase is an indication of stretching or detachment of the lateral canthal tendon; the lateral upper and lower eyelid angle becomes more curved ("C" shaped instead of "V" shaped). The normal lateral canthal position is about 15 degrees above the medial canthal position.
Fat
The prominence of the medial, central, and lateral fat pads is noted. The associated nasojugal and malar grooves undergo assessment.
Midface
The surface of the cornea is normally at the same position as the most prominent position of the cheek. If the cheek is recessed, it is a negative malar angle. This angle may predispose the patient to postoperative lower eyelid retraction after any of the lower blepharoplasty procedures. The cheek position and it's relation to the cornea should be assessed in every patient. The cheek prominence also varies with age and the degree to which the cheek may need to be lifted to support the lower lid. There may be a limitation to the degree to which a purely transconjunctival blepharoplasty is performable in the presence of a negative malar angle.[4]
Jowls
The ophthalmologist or the oculoplastic surgeon may fail to assess the degree to which jowls are present when a patient presents for a lower blepharoplasty. In the presence of prominent jowls, there can be a secondary effect on the skin of the lower and midface, with the resultant downward pull of the lower eyelid. In such patients, care must be taken not to worsen the support normally provided by lower eyelid fat pads as subsequent lower lid retraction will occur.
Technique or Treatment
It is important to recall that patients presenting with "baggy lower eyelids" will always have worse swelling the first hour or so after waking up when they are tired and after salty meals. The rest of the time, the degree of "puffiness" or "bagginess" will vary. Therefore, there is no distinct degree of procedure that may be necessary.
Markings
Patients should be marked sitting up. The outlines of the three fat pads are marked, and a topographical marking is made over the individual pads, together with notes if one pad or side needs more or less attention. Careful attention is paid to the nasojugal groove and the malar groove. In most patients undergoing straight transconjunctival blepharoplasty, these grooves will not be prominent. The presence of prominent nasojugal and malar grooves indicate different surgical procedures. Sometimes, subtle grooves may be present: these should be marked in case they need filling with the patient's own fat or fillers, during or after a transconjunctival lower blepharoplasty.
Anesthesia
Transconjunctival blepharoplasty may be performed under local anesthesia injections or with the use of sedation or even general anesthesia. The local anesthetic injection should be in the region of the lateral canthus, the lower eyelid, and transconjunctivally into the three fat pockets. About 2 ccs of 2% lidocaine with 1:100,000 epinephrine per side is appropriate.
Retraction and Incision
A plastic corneal shield should be placed over the cornea to protect the cornea, maintain ocular surface moisture, and also prevent bright lights from distressing the patient. The lower eyelid is retracted using the smallest available Desmarres retractor: this allows the surgeon access to the inferior fornix. Under traction, an incision is made in the conjunctiva about 6 mm below the inferior tarsal border. However, other levels of making incisions have also been presented.[5] This incision can be carried to the inferior orbital rim in a post-septal plane. This dissection can be continued into a subperiosteal plane to release the arcus marginalis or orbitomalar ligament, but to access the infraorbital fat pads for excision, an incision in the inferior aspect of the septum is made just superior to the arcus marginalis. A little pressure on the upper eyelid and globe is helpful, making the fat come forward into the inferior fornix, showing the bulge where the incision is made. Although it is increasingly popular for surgeons to use the CO2 laser or the unipolar cautery to cut the conjunctiva, other surgeons prefer to make the incision with a blade and Westcott scissors to avoid collateral heat injury to the conjunctiva.
We have shown that the lower conjunctiva and retractors may be placed on traction using a 4-0 silk suture on a hemostat when performing this surgery: it helps expose the fat pads better and protects the cornea.[6]
Removal of Fat
Again, pressure on the upper eyelid and globe will make each fat pad more prominent. The medial, central, and lateral fat pads are opened via the transconjunctival approach, and judicious removal of the fat is carried out with careful attention to obtaining hemostasis. Although some surgeons clamp the fat in a hemostat and excise the fat, others prefer to remove fat using an "open sky" technique and cauterize vessels as needed. There are prominent vessels in the orbital fat but especially so in the medial fat pad. These require careful cauterization. No forward traction is placed on the fat as this runs the risk of over-excision of the orbital fat.
The central fat pad is deeper (more inferior) than a surgeon may think. It is often necessary to palpate the inferior orbital rim and incise the tissues just above to obtain access to the central fat pad.
The lateral fat pad is the one that is most frequently inadequately removed by inexperienced surgeons. Furthermore, the lateral fat pad needs to be exposed with proper lateral lower eyelid traction and may have a firmer fascia over it than the medial fat pad. Again the relevant fat pad reductions are performed based upon the preoperative assessment. Where necessary, pedicles of fat or free fat grafts may be used during surgery if the nasojugal and malar grooves require attention.[7]
When assessing the degree of fat reduction, it helps to have iced gauze, which may be used to press on the eyelids to reduce edema related to surgery and local anesthetic injections. By balloting the globe, one can get a dynamic impression of the prominence or otherwise of the lower lid fat. Of course, it need not be stressed that lower eyelid fat pads tend to be more apparent when the patient is sitting up and when tired or first thing in the morning. With the patient lying down, the fat "falls back," and therefore, surgical judgment is needed when performing this surgery. Conservative removal of fat and repositioning, sometimes with a septal release, to treat associated grooves is a useful technique.[8][9]
Closure
The traction suture is removed, and the area of surgery is examined once more, looking for any bleeders. One or two buried 6-0 catgut sutures may be used to close the conjunctiva, although it is also acceptable to leave the wound open to allow the egress of any fluids. The wound closes very nicely with or without sutures. It is important not to apply ointment into the inferior fornix as granulomas may occur if the lanolin in the ointment gains access to the deeper tissues.[10]
Patching
Some surgeons prefer not to patch the eyes after transconjunctival blepharoplasty. Ice packs are placed over a moist gauze or face cloth. Topical antibiotic ointment may be applied to the outer and inner corners of the eyes.
Postoperatively
It is common to observe the patient for a minimum of 30 minutes after surgery and examine the surgical site for any hematoma or bleeding as well as assess the patient's vision before considering discharge to home.
Postoperative Instructions
The patient is discharged with instructions to ice the eyelids on-and-off for the following 24 to 48 hours. Topical antibiotic eye ointment is prescribed and applied twice a day. If laser or a TCA peel has been used on the skin, appropriate moisturizing is instituted. The patient is asked to sleep with two to three pillows for the first two to three nights. The patient may bathe/wash the next day but is informed that there will be some blurry vision, especially when using the ointment. Artificial tears may be used as needed. Strict instructions are given to the patient to call the emergency number of the surgeon if there is any undue pain, bleeding, or change in vision.
Complications
Complications of the transconjunctival blepharoplasty include[11]:
- Chemosis
- Infection
- Bleeding
- Residual prominence of fat pads
- Lower eyelid retraction
- Excessive fat removal
- Neuropraxia
- Trauma to extraocular muscles, most commonly inferior oblique
- Double vision
- Loss of vision
Clinical Significance
Transconjunctival blepharoplasty is a useful procedure with proper patient selection. With an absence of any visible incisions, the results are very gratifying. Although there is a tendency for surgeons to want to simplify lower blepharoplasty, a proper anatomical and physiological approach to assessing and planning lower eyelid blepharoplasty is vital.[12][13]
Enhancing Healthcare Team Outcomes
With a purely cosmetic procedure such as transconjunctival blepharoplasty, the surgeon must ensure that a complete and detailed examination has been performed to avoid complications. In particular, this procedure is dependent upon the surgeon's skills as an accomplished examiner and diagnostician. The ophthalmology nurse familiar with the procedure should assist in follow up evaluation and monitoring the patient for complications. [Level 5]