Continuing Education Activity
Blunt cardiac injury (BCI) refers to damage to the heart typically resulting from high-impact trauma, such as motor vehicle accidents, pedestrian collisions, motorcycle crashes, and significant falls. Previously termed "cardiac contusion," BCI encompasses a broad spectrum of myocardial injuries ranging from minor, asymptomatic conditions to severe, life-threatening cardiac ruptures. Often clinically silent initially, BCIs can lead to sudden arrhythmias or cardiac pump failure, requiring careful monitoring and treatment. Symptoms may include chest pain, shortness of breath, and arrhythmias—but many patients initially present without symptoms initially. Diagnosing BCI is challenging due to the lack of standardized diagnostic criteria and a definitive diagnostic test. Evaluation typically involves a thorough physical examination, electrocardiogram, cardiac biomarker monitoring, and possibly echocardiography. Treatment focuses on addressing dysrhythmias, providing supportive care, and, in severe cases, surgical intervention may be necessary.
Participants in this course gain comprehensive knowledge about the significance of BCI, learning to perform the recommended evaluations and implement appropriate management strategies. The course emphasizes the importance of collaborating with an interprofessional team that includes emergency physicians, cardiologists, nurses, and surgeons. This collaborative approach enhances patient outcomes by ensuring timely diagnosis, comprehensive monitoring, and coordinated care plans that address immediate and long-term needs.
Objectives:
Identify the clinical signs and symptoms associated with blunt cardiac injury, including both symptomatic and asymptomatic presentations.
Differentiate between blunt cardiac injury and other potential causes of chest trauma-related symptoms through careful assessment and diagnostic procedures.
Assess the severity of myocardial injury in patients with blunt cardiac injury using advanced diagnostic tools, including echocardiography and cardiac magnetic resonance imaging when indicated.
Collaborate with an interprofessional team, including emergency physicians, cardiologists, nurses, and surgeons, to ensure comprehensive care for patients with blunt cardiac injury.
Introduction
Blunt cardiac injury (BCI) encompasses a spectrum of conditions resulting from blunt chest trauma, ranging from minor myocardial bruising to severe, life-threatening cardiac rupture. While a minority of patients exhibit abnormal electrocardiogram (ECG) results or signs of shock, most present with no symptoms initially. However, the risk of sudden arrhythmias or cardiac pump failure necessitates consideration of BCI to ensure appropriate monitoring and treatment.[1]
The term "cardiac contusion" has traditionally been used to describe heart injuries following blunt chest trauma.[2] Histologically, a cardiac contusion is marked by a contused myocardium with hemorrhagic infiltrate, localized necrosis, and edema. These findings are most definitively confirmed during surgery or autopsy.[3] However, the clinical term blunt cardiac trauma is now preferred, as it encompasses the broad range of potential cardiac injuries resulting from blunt chest trauma.[4][5]
Between 2017 and 2021, according to the National Trauma Data Bank, a reported 14,219 out of 4.8 million patients with blunt trauma patients were diagnosed with BCI, resulting in a 0.3% overall incidence rate.[6] BCIs can be further described by specific injuries or observed dysfunction.[7] Significant BCI is usually associated with high-impact trauma, with motor vehicle accidents accounting for 50% of cases, pedestrians struck by motor vehicles for 35% of cases, motorcycle crashes for 9% of cases, and falls from significant heights for 6% of cases.[8][9][10]
Diagnosing BCI is challenging due to the lack of standardized diagnostic criteria and a definitive diagnostic test. The difficulty is compounded in polytrauma patients. The reported incidence of cardiac injury following blunt chest trauma ranges from 8% to 76%, primarily due to the absence of established diagnostic guidelines.[10] In patients without severe arrhythmias and hemodynamic instability, the significance of BCI is sometimes debated.[8][11] In the setting of blunt trauma, a high clinical suspicion for BCI is required, and certain patients should be monitored for adverse sequelae; no pathognomonic clinical signs or symptoms have been supported by evidence that correlates with the risk of cardiac complications.[8][12][13] Consequently, the sequelae of BCI are more important than its label.
Etiology
BCI from blunt chest trauma is most commonly due to motor vehicle collisions (50%), with 20% of all motor vehicle collision deaths involving blunt chest trauma.[4] Other mechanisms, including falls, blast injuries, assault, and other blunt mechanisms, also play a role.[2] The mechanism and magnitude of force determine the cardiac injury sustained. With enough force, the heart can be compressed between the sternum and spine. Deceleration injury may tear the heart from its attachments. Most often, these types of injuries are not survivable, and patients typically expire in the field. Although BCI may be associated with injuries to nearby structures, including the thoracic aorta, lung, rib, sternum, and spine, these types of injuries do not definitively indicate BCI. However, clinicians should have high clinical suspicion when caring for patients with thoracic injury.[9]
Epidemiology
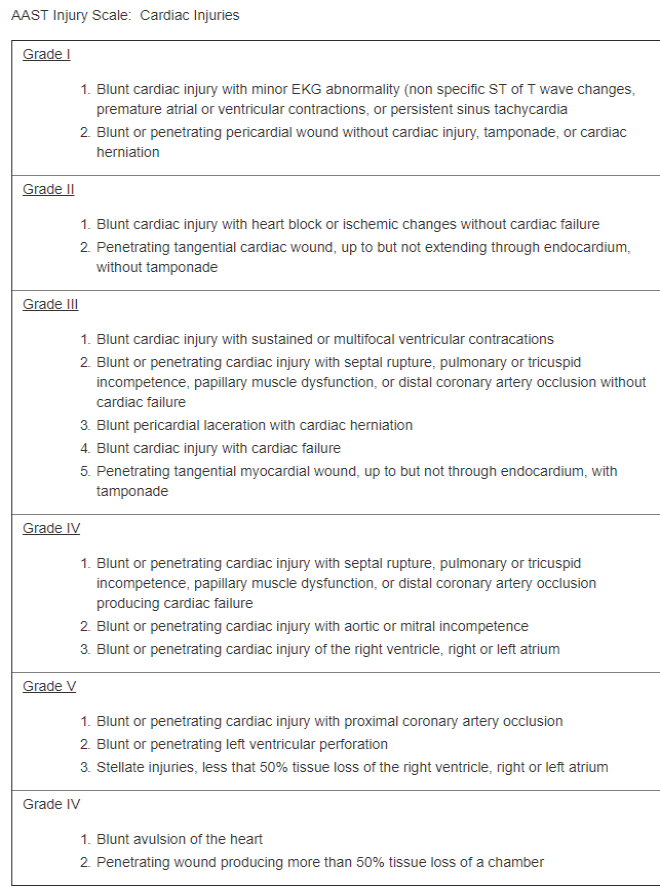
In the United States, trauma is the 4th leading cause of death. BCI incidence has a wide range due to a lack of widely accepted diagnostic criteria, inconsistencies in reporting, and the absence of an established definition. Misdiagnosis can occur when clinical features overlap with differential diagnoses not related to BCI, such as an arrhythmia secondary to a preexisting condition. Furthermore, diagnostics, including elevated troponins, can be due to trauma unrelated to the chest.[14] The American Association for the Surgery of Trauma (AAST) developed the AAST Cardiac Injury Scale, which is used to grade blunt and penetrating cardiac injuries (see Image. The American Association for the Surgery of Trauma Injury Scale). However, clinicians should be aware that patients with multiple penetrating wounds to a single chamber or multiple chamber involvement increase the injury grade by a factor of 1.
Pathophysiology
Direct, indirect, bidirectional, deceleration, blast, crush, concussive, or combined are potential mechanisms that have been suggested for BCI.[2][4][15] Direct impact to the chest is considered the most common mechanism, and cardiac injury is most likely when the ventricles are maximally distended at the end of diastole.[8] An indirect increase in preload by way of abdominal or extremity veins can result in a sudden increase in the intracardiac pressure, thereby making the heart susceptible to rupture.[8] Bidirectional forces result in compression of the heart between the spine and sternum.[8] Deceleration mechanisms may result in tears to valvular structures, the myocardium, or coronary arteries.[2][8]
The cardiac chamber injury distribution reflects the position of the heart in the chest, where the right ventricle and right atrium are more anterior compared to the left ventricle and left atrium.[8][16] The most common cardiac injuries from blunt trauma resulting in death are due to cardiac chamber rupture (64%), venous-atrial confluence tears (33%), coronary artery tear or dissection, or a combination of these.[9] Commotio cordis, usually seen in young men who are athletes, is sudden death due to cardiac arrest from BCI in the absence of preexisting disease and with no morphological injury to the heart at autopsy. Ventricular fibrillation is thought to be a complication that occurs due to impact during ventricular repolarization.[4][9]
Most patients who survive BCI have less severe injuries that range from structural injuries to electrical and conduction disturbances.[9] An intramural hematoma is one such structural injury that, for the most part, has a benign clinical course that resolves in 4 to 12 weeks. Intramural hematomas can cause premature ventricular contraction and transient bundle branch block. Another common structural injury is papillary muscle rupture, which can lead to valve regurgitation and may require repair.[9] Septal injuries can present with a murmur or arrhythmia on an echocardiogram. This injury begins with contusion followed by necrosis and then delayed rupture. Hence, early diagnosis is important as the injury may be treatable.[8][9] The most common dysrhythmia in BCI is sinus tachycardia, premature atrial or ventricular contractions, and atrial fibrillation.[4][9] Tachycardia in the patient with trauma should raise greater suspicion of ongoing bleeding than BCI. Once bleeding is ruled out, BCI becomes more probable in the differential diagnosis.
History and Physical
Prompt identification of the trauma in the patient with blunt chest injury by the mechanism of force is critical. For instance, patients involved in a motor vehicle collision should be asked if impaction against the steering wheel occurred. In one study, 54% of patients with a fall history more significant than 20 feet had BCI.[9] The most common complaint is chest pain or shortness of breath,[2][4] but some may report palpitations or even present with typical symptoms of angina.[4][17]
Assessment of cardiac risk factors, including history of myocardial infarction, cardiovascular disease, and other commonly associated comorbidities, should be performed. Obtaining an accurate medication history is essential, especially if the patient takes cardiac medications, which can alter the patient's presentation. For example, beta-blockers and calcium channel blockers may mask tachycardia.
The physical exam should be thorough. Patients can present with cardiac tamponade, and suspicion should be high in the presence of jugular venous distention and hypotension. The focused assessment with sonography for trauma (FAST exam) facilitates the assessment of pericardial fluid and cardiac tamponade. However, some nonspecific physical examination findings that should raise clinical suspicion for BCI include tachypnea, irregular lung sounds, chest wall tenderness, chest abrasion or ecchymosis, rib or sternal fractures, and seatbelt signs across the chest.[2][4][12][17] Furthermore, patients with severe BCI are more likely to have other significant traumatic injuries that may mask or distract from some of its physical sequelae.[12][17]
Evaluation
No consensus has been established to diagnose blunt cardiac injuries. However, in 2012, the Eastern Association of Trauma published BCI practice guidelines that supported obtaining an echocardiogram (ECG) in all patients with suspected BCI.[8][9] Patients with abnormal findings should be admitted for continuous cardiac monitoring; however, a normal ECG does not entirely exclude BCI, as it has been reported that a significant number of patients with an initial ECG with normal findings were noted to have a possible cardiac injury 24 hours later as measured by elevated cardiac troponin I (cTnI) levels.[4][8] Nevertheless, patients with a normal ECG in conjunction with normal levels of cTnI can be safely discharged home.[4][8][9] Furthermore, normal ECG and cTnI levels do not exclude all BCIs, as some may have a delayed presentation (eg, septal injury).
Standard diagnostic tests for BCI include ECG, echocardiography, cardiac biomarkers, and radioisotope scanning. If the initial 12-lead ECG is normal, a follow-up ECG after 4 to 6 hours is recommended, along with cardiac biomarker levels (eg, troponin and creatine kinase). Subsequent measurements of these biomarkers and additional echocardiography or radioisotope scans should be based on clinical observations, ECG results, and biomarker levels. However, the approach to managing BCI varies significantly and is often determined by individual hospital protocols. Diagnosing BCI and associated complications in patients with trauma remains a complex task.[18]
Computerized tomography (CT) and magnetic resonance imaging (MRI) do not play a role in the initial diagnostic evaluation of BCI; however, these modalities can be complementary or useful in patients with symptoms without a clear clinical etiology and can be considered on a case-by-case basis.[4][8] FAST is a bedside ultrasound procedure used to evaluate circulation issues in trauma patients. This procedure is recommended for patients who are hemodynamically unstable with blunt abdominal trauma, those with penetrating trauma at the thoracoabdominal junction where it is unclear if the abdominal cavity has been penetrated, and any patient with unexplained instability. The traditional FAST protocol examines the following 4 areas:
- Pericardium (to identify cardiac tamponade)
- Right upper quadrant
- Left upper quadrant
- Pelvis (to detect hemoperitoneum) [6]
The extended FAST (e-FAST) protocol also includes assessing the pleural spaces to check for hemothorax and pneumothorax.[6] Please see StatPearls' companion resource, "Focused Assessment With Sonography for Trauma," for more information.
Treatment / Management
The initial assessment of an injured patient should adhere to the guidelines provided by the American College of Surgeons' Advanced Trauma Life Support (ATLS) course. In cases of shock, all potential causes must be evaluated, especially in patients with thoracic trauma, where cardiogenic and compressive cardiac issues are more prevalent. Physical examination, ECG, and e-FAST are essential to identify critical conditions like pericardial tamponade and significant hemodynamic dysrhythmias.[1] See Image. Blunt Cardiac Injury Algorithm.
Patients with abnormal ECG and cTnI levels should be admitted for cardiac monitoring for 24 to 48 hours because life-threatening arrhythmias or cardiac failure will most likely present during this time.[4][17] Patients can be admitted to the intensive care unit or placed under telemetry, depending on concurrent injuries, type of ECG change, and the grade of hemodynamic imbalance. Admission of all patients with sternal fractures and normal ECG findings is unnecessary to rule out BCI. The most prevalent of the BCIs are the subset of patients with isolated abnormal ECG or cTnI elevations, which usually have a benign course with the rare occurrence of long-term functional impairment.[2]
Dysrhythmias should be treated using the same management approach as in patients without BCI. Replete electrolytes accordingly, avoid hypoxia and acidosis, and when clinically indicated, utilize antidysrhythmics and advanced life support algorithms. Although rare with isolated BCI, a complete heart block may necessitate a pacemaker. ST segment elevations can be due to either a contused heart or a traumatic myocardial infarction, necessitating coronary angiography.[4]
Patients with severe clinically diagnosed or imaged structural cardiac injury require emergent cardiology evaluation for further management. Temporizing measures such as fluid resuscitation, inotropes, or vasopressors may be indicated in the interim based on the specific clinical findings and associated injuries. Patients presenting with cardiac tamponade, most frequently seen in cardiac rupture, require emergent surgical intervention.[2][4] Cardiothoracic intervention is required, and time is of the essence in the majority of those cases. Refractory cardiogenic shock can benefit from an intra-aortic balloon pump to help increase coronary blood flow, allowing the stunned heart to recover in days to weeks.[2]
Differential Diagnosis
Differential diagnoses that should also be considered when evaluating blunt cardiac injury include:
- Arrhythmia
- Cardiac tamponade
- Cardiac wall motion abnormality
- Cardiogenic pulmonary edema
- Cardiogenic shock
- Hemorrhagic shock
- Myocardial infarction
- Valvular regurgitation
Prognosis
Prognosis in BCI is highly dependent on the specified injury, its association with concomitant injuries, and any history of previous cardiac disease or injury.[17] The patient with isolated BCI that is presented by way of an abnormal ECG or cTnI level tends to have a more favorable outcome than the patient who is hemodynamically compromised with a cardiac structural injury with an associated high trauma injury score.[9][17] Given that the former represents the largest pool of patients with BCI, this condition generally has a favorable prognosis overall.
A prospective study compared 12 patients who had experienced a myocardial contusion 12 months earlier with 12 matched patients who had experienced blunt chest trauma without myocardial contusion. Both groups showed no significant differences in ECG results or right and left ventricular function. A more recent prospective study examined patients with blunt thoracic trauma at 3 and 12 months post-injury. Among those with myocardial contusion and wall motion abnormalities, 10 out of 17 patients still had wall motion abnormalities at 3 months, and 4 out of 17 patients had wall motion abnormalities at 12 months. Additionally, exercise testing revealed no ECG abnormalities, and no patients experienced cardiac-related limitations during follow-up.[1]
Complications
Overall, BCI complications are rare.[9][17] Acute complications from severe cardiac injuries usually necessitate immediate management, and those who survive may have long-term complications related to their specific injury. However, most patients with BCI do not have long-term sequelae. Still, a few late complications have been reported, including delayed cardiac rupture, complete atrioventricular block, heart failure, pericardial effusion, and constrictive pericarditis.[9] Therefore, good practice entails reevaluating these patients in 3 to 6 months.[9]
Deterrence and Patient Education
Although long-term outcomes of patients with blunt cardiac injury after discharge are excellent, they should be instructed to return to the clinic for follow-up 3 to 6 months after the trauma for a reevaluation of any signs of cardiac injury and dysrhythmia.
Enhancing Healthcare Team Outcomes
The diagnosis of BCI remains challenging due to its variable presentation and range of injury. Moreover, BCI diagnostic criteria have not been defined. However, a crucial factor in caring for these patients is maintaining a high suspicion in trauma cases. ECG and cardiac enzyme levels can serve as initial screening tools, with subsequent admission and echocardiography for abnormalities, recognizing that BCI may take up to 48 hours to manifest. An interprofessional consensus is essential to identify BCI based on the specific injury. Physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals must collaborate effectively to enhance patient-centered care, improve outcomes, ensure patient safety, and boost team performance.
Interprofessional communication and care coordination are vital, with all team members contributing to rapidly identifying and managing BCI. While the majority of BCI cases may be inconsequential, the true significance of the diagnosis remains controversial due to inadequate assessment of long-term outcomes. Those suspected of having BCI who are hemodynamically stable without dysrhythmia should at least undergo a short observation period. Further consensus and research among clinicians are necessary to better define BCI's management and long-term significance—ultimately improving patient care and outcomes.