Continuing Education Activity
Carpal tunnel syndrome (CTS) is an entrapment neuropathy caused by compression of the median nerve as it travels through the wrist's carpal tunnel. It is the most common nerve entrapment neuropathy, accounting for 90% of all neuropathies. Early symptoms of carpal tunnel syndrome include pain, numbness, and paresthesias. This activity reviews the etiology, presentation, evaluation, and management of carpal tunnel syndrome, and highlights the role of the interprofessional team in evaluating, and managing the condition.
Objectives:
- Describe the pathophysiology of carpal tunnel syndrome, including triggering and exacerbating factors and activities.
- Review the necessary elements for an examination to assess for carpal tunnel syndrome, including any necessary diagnostic imaging studies.
- Summarize the treatment options available for carpal tunnel syndrome, including both conservative and surgical care.
- Explain possible interprofessional team strategies for improving care coordination and communication to advance the evaluation and treatment of carpal tunnel syndrome and improve outcomes.
Introduction
Carpal tunnel syndrome (CTS) is an entrapment neuropathy caused by compression of the median nerve as it travels through the wrist's carpal tunnel. It is the most common nerve entrapment neuropathy, accounting for 90% of all neuropathies. Early symptoms of carpal tunnel syndrome include pain, numbness, and paresthesias. These symptoms typically present, with some variability, in the thumb, index finger, middle finger, and the radial half (thumb side) of the ring finger. Pain also can radiate up the affected arm. With further progression, hand weakness, decreased fine motor coordination, clumsiness, and thenar atrophy can occur.
In the early presentation of the disease, symptoms most often present at night when lying down and are relieved during the day. With further progression of the disease, symptoms will also be present during the day, especially with certain repetitive activities, such as when drawing, typing, or playing video games. In more advanced disease, symptoms can be constant.
Typical occupations of patients with carpal tunnel syndrome include those who use computers for extended periods of time, those who use equipment that has vibration such as construction workers, and any other occupation requiring frequent, repetitive movement.[1][2][3]
Etiology
Carpal tunnel syndrome results from increased carpal tunnel pressure and subsequent compression of the median nerve. The most common causes of carpal tunnel syndrome include genetic predisposition, history of repetitive wrist movements such as typing, or machine work as well as obesity, autoimmune disorders such as rheumatoid arthritis, and pregnancy.[4]
The majority of CTS cases are idiopathic. Secondary CTS causes are divided into abnormalities of the container or content. Dynamic CTS can occur with manual work.
Secondary Carpal Tunnel Syndrome
- Abnormalities of the Container - Any condition that modifies the walls of the carpal tunnel may cause compression of the median nerve
- Dislocation or subluxation of the carpus
- Fractures or skewed consolidation of the distal radius
- Wrist arthrosis, inflammatory arthritis, infectious arthritis
- Acromegaly
- Abnormalities of Content
- Tenosynovial hypertrophy
- Inflammatory rheumatism, and infection
- Diabetes mellitus (abnormality of collagen turnover), primary or secondary amyloidosis (chronic hemodialysis with deposition of beta-2-microglobulin), and go
- Abnormalities of fluid distribution: pregnancy, hypothyroidism, and chronic kidney failure (arteriovenous fistula)
- Arterial hypertrophy of the median nerve
- Intratunnel tumor: lipoma, synovial cyst, synovial sarcoma, or neural tumor (schwannoma, neurofibroma, or lipofibroma)
- Hematoma due to hemophilia, anticoagulant accident or trauma
- Obesity
- Dynamic Carpal Tunnel Syndrome - The pressure inside the carpal tunnel increases during the wrist's repetitive extension and flexion movements. This particular movement can be seen in occupational pathological conditions.
- Exposure to Vibration - Exposure to vibration causes ultrastructural consequences that comprise microcirculatory compression problems and intraneural edema following an injury of the myelin and axons.
Epidemiology
Frequency
In the United States, carpal tunnel syndrome (CTS) has an incidence of 1 to 3 persons per 1000 per year, with a prevalence of 50 per 1000, with similar incidence and prevalence in most developed countries.
Race
It most commonly affects Whites. Whites are two to three times more prone to get affected than Blacks.
Age
The peak age of CTS occurrence is 40-60 years.
Gender
CTS is ten times more common in females as compared to males.[5]
Mortality/Morbidity
Carpal tunnel syndrome does not cause mortality, but it can lead to irreversible median nerve damage, with severe loss of hand function, if not treated.
Pathophysiology
Carpal tunnel syndrome (CTS) is multifactorial and often results from multiple patient-specific, occupational, social, and environmental risk factors. A single, specific cause is not always determined unless there is, for example, a space-occupying lesion that can be attributable to patient-reported symptoms. While this can be appreciated in select medical conditions (e.g., gout), these relatively straightforward clinical presentations are relatively uncommon in comparison to most presentations of CTS.
In general, the pathophysiology of CTS results from a combination of compression and traction mechanisms. The compressive element of the pathophysiology includes a detrimental cycle of increased pressure, obstruction of overall venous outflow, increasing local edema, and compromise to the median nerve's intraneural microcirculation. Nerve dysfunction becomes compromised, and the structural integrity of the nerve itself further propagates the dysfunctional environment - the myelin sheath and axon develop lesions, and the surrounding connective tissues become inflamed and lose normal physiologic protective and supportive function. Repetitive traction and wrist motion exacerbate the negative environment, further injuring the nerve. In addition, any of the nine flexor tendons traveling through the carpal tunnel can become inflamed and compress the median nerve.[6] Sensory fibers often are affected before motor fibers. Autonomic nerve fibers carried in the median nerve also may be affected.
History and Physical
History
Patients often report numbness, tingling, and pain that increase at night. Weakness, clumsiness, and temperature changes also are common complaints. The thumb, second and third digits, and the radial half of the fourth digit are typically affected. Symptoms are intermittent and are associated with activities like driving, reading the newspaper, and painting. Nighttime symptoms are more specific to CTS, especially if the patient relieves symptoms by shaking the hand/wrist. Bilateral CTS is common, but the dominant hand is usually affected first. Numbness predominantly in the fifth digit or extending to the thenar eminence or dorsum of the hand should suggest other diagnoses.
Physical
The clinical physical exam may include testing for sensory and motor deficits and evidence of thenar wasting. There are several special tests with varying degrees of sensitivities and specificities.
Sensory Examination
Abnormalities in sensory modalities are usually present on the palmar aspect of the first three digits and radial one-half of the fourth digit. Sensory examination is most useful in confirming that thenar eminence, hypothenar eminence, and the dorsum of the first web space are normal.
Motor Examination
Wasting and weakness of first and second lumbricals, opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis.
Special Tests
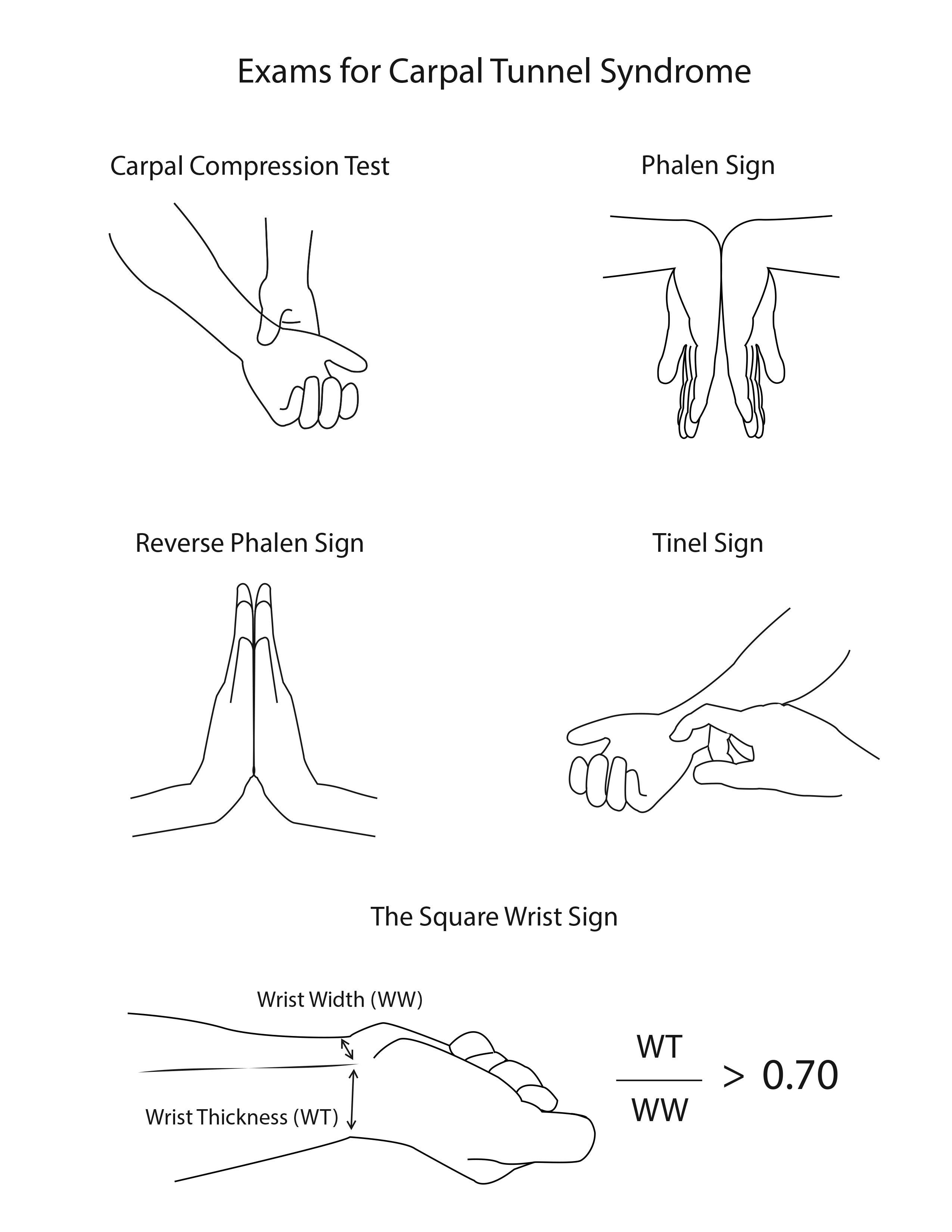
- Hoffmann-Tinel sign - Although a low sensitivity and specificity, the Hoffmann-Tinel sign is another test commonly performed. In this test the healthcare professional taps immediately over the carpal tunnel to stimulate the median nerve. Like the above tests, a positive test is when symptoms are reproduced.
- The carpal compression test - The carpal compression test is the best test. This is done by applying firm pressure directly over the carpal tunnel for 30 seconds. The test is positive when paresthesias, pain, or other symptoms are reproduced.
- Phalen sign - The Phalen test or ‘reverse prayer’ is performed by having the patient fully flex their wrists by placing dorsal surfaces of both hands for one minute. A positive test is when symptoms (numbness, tingling, pain) are reproduced.
- Reverse Phalen test - The reverse Phalen, or ‘prayer test,’ is done by having the patient extend both of their wrists by placing palmar surfaces of both hands together for one minute (as if praying). Again a positive test is with the reproduction of symptoms.
- Palpatory diagnosis - Another test is a palpatory diagnosis. In this test, the health care provider examines soft tissue over the median nerve for mechanical restriction.
- The square wrist sign - The square sign test is an evaluation to determine the risk of developing carpal tunnel syndrome. The test is positive if the ratio of the thickness of the wrist divided by the width of the wrist is great than 0.7.
Evaluation
There is no blood test that could help in the diagnosis of carpal tunnel syndrome.
Magnetic Resonance Imaging (MRI)
MRI of the carpal tunnel is particularly useful preoperatively if a space-occupying lesion in the carpal tunnel is suggested. MRI is a resource-intensive investigation and does not rule out other differential diagnoses.
Ultrasonography
Ultrasonography potentially can identify space-occupying lesions in the carpal tunnel. It can also detect abnormalities in the median nerve like an increased cross-sectional area that can be diagnostic of CTS. Ultrasonography can also help to guide steroid injections into the carpal tunnel.[7]
Electromyography and Nerve Conduction Studies
Electromyography and nerve conduction studies are the basis for carpal tunnel syndrome diagnosis. Other clinical or special exams do not confirm carpal tunnel syndrome but do assist in ruling out other diagnoses. These findings can prompt electromyography and nerve conduction studies. Abnormalities on electrophysiologic testing, in association with specific symptoms and signs, are considered the gold standard for CTS diagnosis. Electrophysiologic testing also can assess the severity of the damage to the nerve and also determine prognosis. CTS is usually divided into mild, moderate, and severe. In mild CTS patients have sensory abnormalities alone on electrophysiologic testing, and in moderate CTS patients have sensory plus motor abnormalities.
Treatment / Management
If carpal tunnel syndrome is identified early, conservative treatment is recommended.
Physical and Occupational Therapy
Initially, the patient should be instructed in modifying symptom provoking wrist movement. This can be through proper hand ergonomics such as placing the keyboard at a proper height and minimizing flexion, extension, abduction, and adduction of the hand when typing. It should be recommended to decrease repetitive activities if possible. Counseling on weight loss and increased aerobic activity also can be beneficial. A properly fitted nighttime wrist splint can be offered. An occupational therapist trained in hand therapy also may be a beneficial referral. Combined therapy may be more beneficial than any single treatment. A short course of nonsteroidal anti-inflammatory medication can relieve symptoms but some do not feel it of adequate benefit.
Medical Treatment
Patients with mild to moderate carpal tunnel syndrome respond to conservative management, which includes splinting the wrist at nighttime for at least three weeks. If conservative treatment fails, a steroid injection into the carpal tunnel can be beneficial.[8] Steroid injections may also be beneficial before surgical management or when surgery is relatively contraindicated as in pregnancy.[8] Median nerve measurements by ultrasound can predict response to steroid injection.
Nonsteroidal anti-inflammatory drugs (NSAIDs) may be useful against CTS in patients with wrist flexor tendinitis. Similarly, diuretics can be helpful in patients with fluid overload. gabapentin and pregabalin, which are used in different types of neuropathic pain, can be used, for CTS off-label.[9] The American Academy of Orthopaedic Surgeons state that oral agents are no better than placebo in the treatment of CTS.
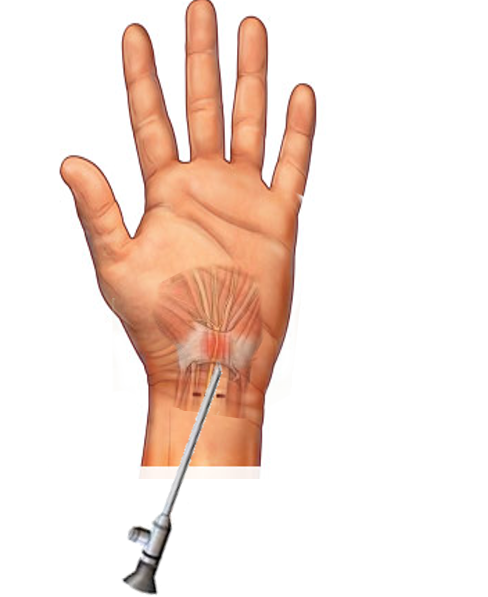
Surgical Treatment
Patients who do not get better following conservative treatment and those who have severe carpal tunnel syndrome as defined by electrophysiologic testing should be considered for surgery. The definitive treatment for persistent carpal tunnel syndrome is a surgical intervention with carpal tunnel release after nerve conduction studies showing significant axonal degeneration. Carpal tunnel release typically is performed by a neuro/orthopedic/plastic surgeon or hand surgeon. This procedure can be performed either open or endoscopically. Carpal tunnel release is considered a minor surgery in which the transverse carpal ligament or flexor retinaculum is cut, opening more space in the carpal tunnel and decreasing pressure on the median nerve. It does not typically require overnight hospitalization.[10][11][12] Surgical release of the transverse ligament gives greater than 90% initial success rate, and low rates of complication. However, it has been found in different trials that the long-term success rate is lower than initially thought (approximately 60% at 5 years).
Guidelines by the American Academy of Orthopaedic Surgeons
The American Academy of Orthopaedic Surgeons released guidelines on the management of CTS. Following recommendations were made:
- Thenar atrophy is strongly associated with ruling in CTS but is poorly associated with ruling it out
- Phalen test, Tinel sign, flick sign, or upper limb neurodynamic/nerve tension test (ULNT) criterion A/B should not be used as independent physical examination maneuvers to diagnose CTS, because alone, each has a poor or weak association with ruling in or ruling out the condition
- Independent history interview topics should not be used to diagnose CTS, because alone, each has a poor or weak association with ruling in or ruling out the condition: sex/gender, ethnicity, bilateral symptoms, diabetes mellitus, worsening symptoms at night, duration of symptoms, patient localization of symptoms, hand dominance, symptomatic limb, age, and body mass index
- Magnetic resonance imaging (MRI) should not be a routine for the diagnosis of CTS
- Diagnostic questionnaires and/or electrodiagnostic studies can be used to aid the diagnosis of CTS
- The following factors are associated with an increased risk of developing CTS: peri-menopausal, wrist ratio/index, rheumatoid arthritis, psychosocial factors, distal upper extremity tendinopathies, gardening, assembly line work, computer work, vibration, tendonitis, workplace forceful grip/exertion
- Physical activity/exercise is associated with a decreased risk of developing CTS
- The use of immobilization (brace/splint/orthosis) should improve patient-reported outcomes
- The use of steroid (methylprednisolone) injection should improve patient-reported outcomes
- There is no benefit to oral CTS treatments (diuretic, gabapentin, astaxanthin capsules, nonsteroidal anti-inflammatory drugs [NSAIDs], or pyridoxine) over placebo
- Oral steroids could improve patient-reported outcomes in comparison with placebo
- The surgical release of the transverse carpal ligament should relieve CTS symptoms and improve function
- Surgical treatment of CTS should have a greater therapeutic benefit at 6 and 12 months in comparison with splinting, NSAIDs/therapy, and a single steroid injection
- There is no benefit to routine postoperative immobilization after carpal tunnel release
Differential Diagnosis
The presentation of carpal tunnel syndrome mimics many other disorders of the musculoskeletal and nervous systems. Following differentials should be considered while assessing a patient with carpal tunnel syndrome:
- Cervical disc disease
- Cervical myofascial pain
- Cervical spondylosis
- Mononeuritis multiplex
- Multiple sclerosis
- Diabetic neuropathy
- Cervical radiculopathy
- Overuse injury
- Traumatic brachial plexopathy
- Radiation-induced brachial plexopathy
- Neuropathies
- Tendonitis
- Tenosynovitis
- Thoracic outlet syndrome
Prognosis
Carpal tunnel syndrome (CTS) is usually progressive over time and can cause permanent median nerve damage. The syndrome recurs to some degree even after surgical management in up to one-third of the patients after 5 years. Almost 90% of mild to moderate CTS cases respond to conservative management. However, many patients progress to requiring surgery. Patients with CTS secondary to diabetes or wrist fracture tend to have a less favorable prognosis than do those with no apparent underlying cause. Patients who have normal electrophysiologic studies have much less favorable operative outcomes than do individuals with abnormalities on these tests and also more complications. Axonal loss on electrophysiologic testing is also a poor prognostic factor.
Complications
Complications of carpal tunnel syndrome are divided into two groups:
Complications due to Carpal Tunnel Syndrome
- Carpal tunnel syndrome may cause irreversible median nerve damage, leading to permanent impairment and disability.
- Chronic wrist and hand pain with or without reflex sympathetic dystrophy.
- CTS can cause atrophy and weakness of the muscles at the base of the thumb in the palm of the hand. This can lead to a lack of dexterity of the affected fingers.
Complications due to Carpal Tunnel Surgery
- The most frequent complication is neuroma of the palmar cutaneous branch of the median nerve.
- Hypertrophic scars
- Dysesthesias after multiple procedures to release the carpal tunnel
- Wrist Joint stiffness
- Failure to relieve symptoms
Deterrence and Patient Education
Patients suffering from carpal tunnel syndrome should be educated about the nature of the disease, precautions that they need to take, and rehabilitative activities. These include:
- Avoid repetitive hand motions, holding onto vibrating tools, heavy grasping and positioning, or working with your wrist bent down and out.
- Quit smoking
- Lose weight if overweight
- Reduce caffeine intake
- A wrist brace will sometimes decrease the symptoms. A brace keeps the wrist in a resting position, not bent back or bent down too far. A brace can be especially helpful for relieving the numbness and pain felt at night because it can keep your hand from curling under as you sleep. The wrist brace can also be worn during the day.
- Consult with a physical or occupational therapist. Therapist may check the workstation and the way the patient does his/her work tasks. Therapist would give suggestions regarding the use of healthy body alignment and wrist positions, helpful exercises, and tips on how to prevent future problems.
Pearls and Other Issues
The carpal tunnel includes the median nerve and nine flexor tendons. The flexor tendons include the four tendons from the flexor digitorum profundus, four tendons from the flexor digitorum superficialis, and one tendon from the flexor pollicis longus. The transverse carpal ligament (flexor retinaculum) makes up the superior boundary, and the carpal bones form the inferior border.
Enhancing Healthcare Team Outcomes
The diagnosis and management of carpal tunnel syndrome are done with an interprofessional team that includes the primary care provider, nurse practitioner, physical therapist, neuro/orthopedic/plastic surgeon, and the emergency department provider. The initial treatment is usually conservative combined with limiting repetitive activities. A properly fitted nighttime wrist splint can be offered. An occupational therapist trained in hand therapy also may be a beneficial referral. Combined therapy may be more beneficial than any single treatment. A short course of nonsteroidal anti-inflammatory medication can relieve symptoms but some do not feel it is of adequate benefit.
Many other treatments are available to treat carpal tunnel syndrome including surgery. An orthopedic specialty nurse can assist at all phases of care, regardless of whether treatment is conservative or surgical. While surgery can relieve symptoms, recurrence is not uncommon. The patient must be fully educated about the potential complications of surgery which should only be undertaken after conservative treatments have failed. An interprofessional team approach will lead to better outcomes for patients with CTS.[13][14] [Level 5]