Continuing Education Activity
Chiari II malformation is a relatively common congenital malformation of the posterior fossa and the spine characterized by beaked midbrain, downward displacement of the tonsils and cerebellar vermis, and spinal myelomeningocele. This disorder can have severe morbidity and mortality if it is not identified and treated promptly. This activity highlights the role of the interprofessional team in evaluating and managing patients with this condition.
Objectives:
- Describe the etiology of Chiari II malformation.
- Review the appropriate evaluation of Chiari II malformation.
- Outline the management options available for Chiari II malformation.
- Summarize the importance of the interprofessional team to improve outcomes for patients affected by Chiari II malformation.
Introduction
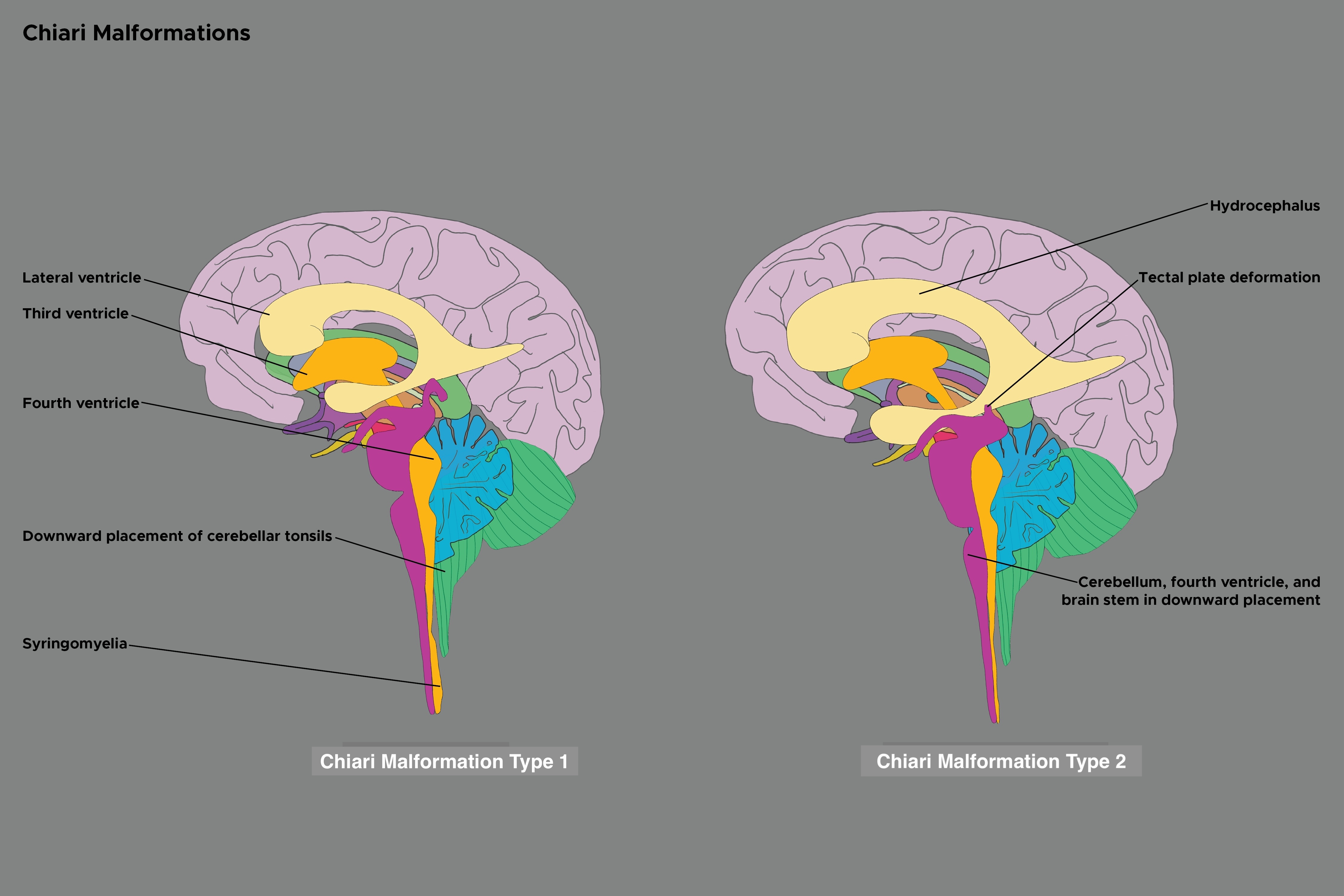
Chiari II malformation (CM-II), commonly known as Arnold-Chiari malformation, is a relatively common congenital malformation characterized by beaked midbrain, downward displacement of the tonsils, and cerebellar vermis, and spinal myelomeningocele.[1] This malformation is frequently misunderstood as a more severe version of Chiari I malformation (CM-I). However, these are two distinct diseases with overlapping imaging findings. Interestingly, most patients who have myelomeningocele also have CM-II and are typically associated with hydrocephalus. There are many additional findings associated with CM-II, including cerebellar dysplasia, elongation of the lower pons and the medulla, and the fourth ventricle displacing into the cervical canal. The diagnosis is primarily based on the patient’s neuroanatomy on MRI. The treatment is typically centered upon surgical interventions. Prognosis is dependent on the extent of the malformations and the symptoms of the patient.
Etiology
The exact etiology of CM-II is not well understood. Many theories have been described; however, none explain all the features. Overall it is thought that CM-II occurs because of an in utero malformation of the cranial structures and the spine. This then results in the displacement of the cerebellum, medulla, and fourth ventricle through the foramen magnum. The associated myelomeningocele is thought to arise from an in utero CSF leak.
Epidemiology
CM-II is encountered relatively common, with an incidence of about 1 in 1000 live births. However, the true frequency is difficult to determine. It is commonly associated with neural tube defects in nearly 100% of cases, with myelomeningocele being the most common defect. Furthermore, if a child is found to have myelomeningocele at birth, most (about 95%) are associated with CM-II. CM-II is the most common Chiari malformation type that presents in childhood.
History and Physical
CM-II's clinical presentation varies wildly. This is largely due to the wide range of severity of the malformation and the numerous associated abnormalities that are not uncommonly encountered. However, because myelomeningocele is typically present, CM-II can usually be detected at birth.[2] The patient's presentation varies by age, as described below:
- Neonatal
- Patients typically present with myelomeningocele. Other manifestations include arm weakness, stridor, dysphagia, aspiration, and apneic spells.
- Child
- Patients will usually have progressive hydrocephalus
- Young adult
Evaluation
When evaluating a patient with CM-II, the diagnose is primarily based on the neuroanatomy seen on imaging. There are currently no biomarkers in the cerebrospinal fluid, cultured tissue, or blood to confirm the diagnosis. As such, neuroimaging with magnetic resonance imaging (MRI) is the most important modality in evaluating patients. For patients who can not tolerate an MRI, a CT can aid in the diagnosis of CM-II. If fetal ventriculomegaly is present, the diagnosis of CM-II can be made with fetal ultrasound in some cases.
- Antenatal ultrasound – classic findings[3][4]
- Lemon sign – describes the frontal bone indentation depicting a lemon
- Banana cerebellum sign – describes the cerebellum wrapping around the brain stem
- MRI - posterior fossa classic findings
- Small posterior fossa
- Brainstem appearing downward displaced
- Low-lying and elongated fourth ventricles
- Beaked tectal plate
- Inferior displaced cerebellar tonsil and vermis through the foramen magnum
- MRI - spine classic findings
- Spina bifida aperta
- Myelomeningocele
- Tethered cord
Overall, the diagnosis of CM-II requires careful evaluation if there is evidence of spinal myelomeningocele. MRI can be useful in diagnosing CM-II by showing a downward displacement of the medulla and cerebellum vermis, among other findings as described above.
Treatment / Management
Management of CM-II depends on the extent of the malformation and the neurological impairments associated with it. Often, surgical interventions are required. Some procedures include treatment for hydrocephalus, closure of open neural tube defects, and decompression of posterior fossa structures. Certain medical problems such as neonatal feeding difficulties, apnea, respiratory failure, and neurogenic bowel require nonsurgical management.
Surgical intervention to repair myelomeningocele is commonly required. Some evidence has demonstrated benefits in performing the procedure on the in utero fetus.[5] For infants with a myelomeningocele diagnosis who did not have a fetal intervention performed, delivery should ideally occur in a hospital with a level III neonatal ICU. Initial management following the delivery includes providing prophylactic antibiotics and covering the lesion. Within the first 72 hours, the back lesion should be closed surgically.[6] Post-surgery, the patient requires close evaluation for the development of hydrocephalus.[7] Serial evaluation for abnormal neurological function is required throughout life. Importantly in patients with myelomeningocele, nearly all will have a neurogenic bladder. This typically requires intermittent catheterization to decrease the risk of renal disease. Importantly, a change in function may suggest an acute neurological complication.[8]
Hydrocephalus is a common problem encountered in the management of CM-II. The timing and need for surgical intervention in patients are primarily determined by neuroimaging findings and the severity of symptoms. Urgent surgical intervention is required in patients with rapidly progressive hydrocephalus. Another important indication for surgery is if a patient is symptomatic and has hydrocephalus. Some symptoms include vomiting, developmental delays, headaches, focal neurologic deficits, and papilledema. An additional indication includes progressive ventriculomegaly and clear evidence of an obvious obstruction on imaging. The most common surgical intervention is the placement of a shunt. This prevents the CSF from accumulating, allowing the CSF to flow from the ventricles to the peritoneum and then get absorbed. This procedure helps improve neurological function.[9]
Surgery to restore normal CSF flow by decompressing the craniocervical junction may also be required. Posterior decompression is the most common procedure using a suboccipital craniectomy with or without duraplasty. Most surgeons favor a posterior fossa decompression with the duraplasty. Potential complications include CSF leak, meningitis, pseudomeningocele formation, and acute postoperative hydrocephalus. Another possible procedure includes anterior foramen magnum decompression (typically via transoral odontoidectomy), an alternative surgical technique typically used when posterior decompression fails.[10] An additional procedure utilizes multiple shunts but is predominately utilized for patients with Chiari I malformation.
Differential Diagnosis
- Chiari I malformation, which has no myelomeningocele, may have brainstem descent
- Isolated myelomeningocele with no posterior fossa abnormality
- Spinal astrocytoma
- Chordoma
- Encephalocele
However, the diagnosis is usually straightforward if imaging reveals a brainstem descent and myelomeningocele.
Prognosis
The prognosis of CM-II is variable, dependent on the extent of the malformations and the patient's symptoms. Typically the symptoms of the patient are improved after surgery, though results vary from patient to patient. If nerve damage was present prior to the surgery, this could be long-term and difficult to treat. Some patients may require repeat surgeries. Large retrospective studies have demonstrated postoperative stabilization or improvement for the majority of patients.
Complications
The complications of a CM-II include:
- Development or worsening of a syrinx
- Permanent damage to nerves or muscles
- Paralysis
- Respiratory failure
- It may be fatal in some cases
Deterrence and Patient Education
Chiari II malformation (CM-II), commonly known as Arnold-Chiari malformation, is a relatively common congenital malformation characterized by a downward displacement of the tonsils and cerebellar vermis and spinal myelomeningocele.[1] Most patients who have myelomeningocele also have CM-II and are typically associated with hydrocephalus. Diagnosis is primarily made based upon the patient’s neuroanatomy through MRI. The treatment is typically centered upon a surgical intervention but is complex because of the variability of the malformation. Prognosis is dependent on the extent of the malformations and the symptoms of the patient.
Enhancing Healthcare Team Outcomes
The management of patients with CM-II is best when using an interprofessional team that includes primary care doctors, neurosurgeons, and radiologists. CM-II trained nurses, physical therapists, and pharmacists should also assist in the case. The patients typically present early in their clinical course because of the associated abnormalities, including myelomeningocele. Utilizing clinical and radiographic findings, the diagnosis can be made. Treatment of CM-II often requires intervention from neurosurgery. Attention must also be given to neonatal feeding difficulties, apnea, respiratory failure, and neurogenic bowel. If there is residual impairment, rehabilitation is essential to regain mobility and function. Long-term follow-up is essential to evaluate for worsening symptoms and whether additional treatment is necessary. Open communication between interprofessional team members is essential for improving outcomes. [Level 5]
This research was supported (in whole or part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author and do not necessarily represent the official view of HCA healthcare or any of its affiliated entities.