Continuing Education Activity
Chlamydia trachomatis is responsible for the greatest number of sexually transmitted infections and the majority of infection-related of blindness worldwide. In the United States, it is the most commonly reported bacterial infection. This activity reviews the evaluation and management of Chlamydia trachomatis infections and highlights the role of the interprofessional team in the care of affected patients.
Objectives:
- Describe the global incidence and prevalence of chlamydia trachomatis.
- Describe the common presentations of chlamydia trachomatis infections.
- Describe the appropriate treatment of chlamydia trachomatis infections.
- Explain the importance of enhancing care coordination amongst the interprofessional team to improve outcomes for patients with chlamydia trachomatis infections.
Introduction
Chlamydia is a sexually transmitted infectious disease caused by the bacterium Chlamydia trachomatis. In the United States, it is the most commonly reported bacterial infection. Globally, it is the most common sexually transmitted infection. It causes an ocular infection called "trachoma," which is the leading infectious cause of blindness worldwide.
In females, the cervix is the anatomic site that is most commonly infected. This can manifest as cervicitis, urethritis, pelvic inflammatory disease, perihepatitis, or proctitis. Chlamydial infections in women, especially if untreated, increase the risk of infertility and ectopic pregnancy, leading to high medical costs.[1] There are also risks if a woman has an infection during pregnancy. Additionally, infants born vaginally to mothers infected with genital Chlamydia trachomatis may develop conjunctivitis and/or pneumonia.
In men, infection with Chlamydia trachomatis can lead to urethritis, epididymitis, prostatitis, proctitis, or reactive arthritis. Both men and women infected with C. trachomatis may also experience conjunctivitis, pharyngitis, and lymphogranuloma venereum. Lymphogranuloma venereum (LGV), caused by distinct serovars of Chlamydia trachomatis, is a less common disease characterized by enlarged lymph nodes or severe proctocolitis.[2]
Etiology
Chlamydia trachomatis is part of the chlamydophila genus. These bacteria are gram-negative, anaerobic, intracellular obligates that replicate within eukaryotic cells. C. trachomatis differentiates into 18 serovars (serologically variant strains) based on monoclonal antibody-based typing assays. These serovars correlate with multiple medical conditions as follows[3]:
-
Serovars A, B, Ba, and C: Trachoma is a serious ocular illness that is endemic in Africa and Asia. It is characterized by chronic conjunctivitis and has the potential to cause blindness
-
Serovars D-K: Genital tract infections, neonatal infections
-
Serovars L1-L3: Lymphogranuloma venereum (LGV), which correlates with genital ulcer disease in tropical countries.
Epidemiology
Urogenital chlamydia infections are the most commonly reported bacterial infections in the U.S and the most common cause of sexually transmitted infections in the world. The overall rate of urogenital infection amongst U.S. women is two times that of U.S. men, with a higher prevalence in women 15-24 years of age and a higher incidence in men between 20-24 years of age.
Pathophysiology
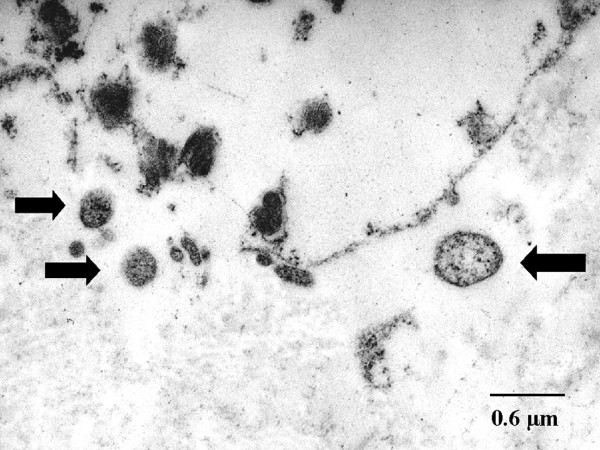
Chlamydia is unique among bacteria, having an infectious cycle and two developmental forms. These include the infectious form called the elementary body (EB) and the reticulate body (RB). The EB is metabolically inactive and is taken up by host cells. Within the host cell, the EB will differentiate into the metabolically active RB. The RB will then use host energy sources and amino acids to replicate and form new EB, which can then infect additional cells. C. trachomatis targets the squamocolumnar epithelial cells of the endocervix and upper genital tract in women, and the conjunctiva, urethra, and rectum in both men and women.
The bacterium is transmitted through direct contact with infected tissue, including vaginal, anal, or oral sex, and can even be passed from an infected mother to the newborn during childbirth.
Histopathology
Typical intracytoplasmic inclusions and free chlamydiae are identifiable in Giemsa-stained cell scrapings from the eye. Stained conjunctival scrapings are positive in 90% of infants with neonatal conjunctivitis, and 50% of adults with inclusion conjunctivitis. Cytology techniques can be used to evaluate endocervical scrapings, but the sensitivity and specificity are low.[4]
History and Physical
C. trachomatis can lead to many urogenital infections, including cervicitis, pelvic inflammatory disease, urethritis, epididymitis, prostatitis, and lymphogranuloma venereum. Extragenital infections caused by C. trachomatis include conjunctivitis, perihepatitis, pharyngitis, reactive arthritis, and proctitis.
More frequently, patients remain asymptomatic reservoirs of the disease. In the minority of patients who become symptomatic, clinical signs depend on the location of the infection. Below are the common signs and symptoms associated with C. trachomatis urogenital infections.
- Cervicitis: Approximately 70% of women will be asymptomatic or have mild symptoms such as vaginal discharge, bleeding, abdominal pain, and dysuria.[5] Only a minority of women have the classic presentation of mucopurulent cervicitis with discharge and easily-induced endocervical bleeding. Some women may complain of postcoital bleeding or intermenstrual bleeding.
- Pelvic Inflammatory Disease: This occurs when C. trachomatis ascends to the upper reproductive tract. Most commonly, these patients will have abdominal or pelvic pain with or without signs and symptoms of cervicitis. Other symptoms include nausea, vomiting, fevers, chills, low back pain, pain with intercourse, dysuria, or postcoital bleeding. [6]
- Urethritis: It is most commonly seen in men. There are subtle clinical differences between gonococcal urethritis and chlamydial urethritis, but making a reliable distinction without testing is not possible. It presents with dysuria and urethral discharge, which is typically white, gray, or sometimes clear, and may only be evident after penile "stripping" or during morning hours. Women with urethritis may complain of frequency or dysuria and may mistake their symptoms for a urinary tract infection. Urinalysis will reveal pyuria, but neither bacterial culture nor gram stain will reveal organisms.
- Perihepatitis: Also called Fitz-Hugh-Curtis syndrome, this syndrome occurs when chlamydia infection leads to inflammation of the liver capsule and the peritoneal surfaces nearby. This syndrome is most commonly seen in patients who have a pelvic inflammatory disease, and it is associated with right upper quadrant or pleuritic pain. Unlike other conditions that may affect the liver or cause right upper quadrant pain, abnormalities in liver enzymes are not typically found.
- Epididymitis: Typically, men will present with unilateral testicular pain and tenderness, possible hydrocele, palpable swelling of the epididymis, and fever.
- Proctitis: Rectal infection with chlamydia can be asymptomatic if caused by genital serovars D through K. However, if LGV serovars L1-L3 are the cause of proctitis, patients may complain of rectal pain, discharge, and bleeding in the setting of receptive anal intercourse. Patients may also present with a fever or malaise. This is seen almost exclusively in males who have sex with males; however, anal intercourse is not uncommon in heterosexual intercourse.
- Prostatitis: Symptoms include dysuria, urinary dysfunction, pelvic pain, and pain with ejaculation. Expressed secretions from the prostate may show increased leukocytes on microscopy.
- Reactive Arthritis: Approximately 1% of men who have urethritis from chlamydial infection also develop reactive arthritis, and a third will have the reactive arthritis triad (formerly known as Reiter syndrome).[7] The triad consists of arthritis, urethritis, and uveitis.
- Conjunctivitis: Direct inoculation with genital secretions infected with genital Chlamydia trachomatis serovars can lead to conjunctival infection. Symptoms typically include non-purulent conjunctivitis (erythematous injection of the surface epithelium). The conjunctiva may have a cobbled appearance. Conjunctivitis is the most common manifestation of chlamydial infection in newborns.
- Pneumonia: Infants born to mothers who have a cervical infection with Chlamydia trachomatis may develop pneumonia 5-30% of the time.[8] Recognition usually occurs between 4 to 12 weeks of age, though almost all infants have symptoms before eight weeks. Nasal congestion and cough are common, and some infants may have thick nasal secretions.[9] Infants usually have no fever or only a minimal fever, they may have tachypnea, and they may have a characteristic paroxysmal staccato cough. In preterm infants, apneic spells may be seen. Rales may be heard on auscultation of the lungs, but wheezing is uncommon.
- Pharyngitis: While not considered a significant cause of pharyngitis, C. trachomatis can be detected in the pharynx with nucleic acid amplified tests.
- Lymphogranuloma Venereum: Patients will present with painless genital ulcers. The ulcers typically have a small, stellate appearance. The development of inguinal lymphadenopathy typically follows the appearance of ulcers.
Evaluation
Among C. trachomatis infections, the only trachoma is diagnosable on clinical grounds. Other chlamydial infections are associated with specific clinical syndromes but require laboratory confirmation. The gold standard for the diagnosis of urogenital chlamydia infections is nucleic acid amplification testing (NAAT). This test is run on either the vaginal swabs for women or first-catch urine for men. Testing can also be performed on endocervical or urethral swabs. Swabs should have a wire or plastic shaft; the tip should be dacron or rayon or a cytobrush. Other materials may inhibit Chlamydia trachomatis. Alternative methods of testing include culture, rapid testing, serology, antigen detection, and genetic probes. If there is no testing available, treatment is recommended based on clinical presentation.
When a patient presents with suspected chlamydia infection, a workup for other STDs should be carried out. A complete blood count is essential if PID is suspected. One may consider testing for HIV, gonorrhea, and syphilis. The sexual partner must be tested for chlamydia. A pregnancy test should be done as it is a contraindication to doxycycline therapy.
Cytology is often used in patients with conjunctivitis and ocular trachoma. Cultures are usually not done for chlamydia as the organism is difficult to grow in the laboratory. However, in patients with anal and rectal involvement, cultures are ideal as other tests are difficult to interpret.
The United States Preventive Services Task Force (USPSTF) recommends regular screening for chlamydia in all sexually active women because if left untreated, the infection is associated with PID, infertility, and chronic pelvic pain. In males, the leucocyte esterase test in urine can be done and is diagnostic for gonorrhea or chlamydia in the absence of a UTI.
Treatment / Management
The goal of treatment is the prevention of complications associated with infection (e.g., PID, infertility), to decrease the risk of transmission, and the resolution of symptoms. Treatment for uncomplicated urogenital chlamydia infection is with azithromycin. Doxycycline is an alternative, but azithromycin is preferred as it is a single-dose therapy. Other alternatives include erythromycin, levofloxacin, and ofloxacin.
Chlamydial infection and gonococcal infections often coexist. In men, the co-treatment for urogenital gonococcal infection should occur on the basis of the detection of the organism on NAAT or gram stain. In women, the gram stain is less helpful due to the possibility of normal Neisseria species colonization within the vaginal flora. Therefore, co-treatment should be dependent on an assessment of individual patient risk and local prevalence rates.
Patients should have partners identified and tested. They should also be counseled on high-risk behaviors, avoid sexual activity for one week after initiating therapy, and should consider testing for HIV.
Verification of cure should occur three weeks after treatment completion, and retesting should be performed three months after treatment.
If symptoms persist after treatment, consider coinfection with a secondary bacterium or reinfection.
Follow up culture is not recommended in most people but may be considered in a pregnant female. [10][11][12][11][10]
Differential Diagnosis
Because Chlamydia trachomatis can lead to a broad spectrum of clinical diseases or manifestations, the differential diagnosis of various presenting complaints is also broad. One should consider other etiologies that may affect each body area or organ systems and may manifest similarly.
Dysuria:
- Gonorrhea
- Genital herpes
- Urinary tract infection
Abdominal Pain:
- Appendicitis
- Cholecystitis
- Constipation
Pelvic Pain:
- Endometriosis
- Ovarian cysts
- Adenomyosis
Vaginal Discharge:
- Bacterial vaginosis
- Trichomonas vaginalis
- Gonorrhea
- Vaginal candidiasis
- Foreign body
- Mycoplasma genitalium infection
- Ureaplasma infection
Rectal Discharge:
- Inflammatory bowel disease
- Gonorrhea
Conjunctivitis:
- Viral infection
- Allergy
- Gonococcal infection
Postcoital or Intermenstrual Bleeding:
- Cervical cancer
- Cervical or endometrial polyp
- Cervical ectropion
- Leiomyoma
- Pregnancy
Genital Ulceration:
- Herpes simplex
- Syphilis
- Chancroid
- Granuloma inguinale
Treatment Planning
Uncomplicated Genital Chlamydia:
The World Health Organization (WHO) recommendations for treatment of uncomplicated genital chlamydia infections are the following:
- Azithromycin 1000 mg orally as a single dose or
- Doxycycline 100 mg orally twice a day for seven days, or one of these alternatives: tetracycline 500 mg by mouth four times a day for seven days, erythromycin 500 mg orally twice daily for 7 days, or ofloxacin 200-400 mg orally twice daily for 7 days
Anorectal Chlamydial infection:
In anorectal chlamydial infections, the WHO recommendation is oral doxycycline 100 mg twice daily for 7 days over oral azithromycin 1 g as a single dose.
Chlamydial infection in pregnancy:
WHO recommends the following for the treatment of chlamydial infection in pregnancy:
- Azithromycin recommended over erythromycin, amoxicillin, and erythromycin
- Azithromycin 1 g orally as a single dose or
- Amoxicillin 500 mg orally three times daily for 7 days or
- Erythromycin 500 mg orally twice daily for 7 days
Lymphogranuloma Venereum:
The WHO recommends the following for the treatment of lymphogranuloma venereum (LGV):
- In adults and adolescents with lymphogranuloma venereum, the guidelines suggest doxycycline 100 mg orally twice a day for 21 days over azithromycin 1 g orally weekly for 3 weeks.
- Good practice dictates the treatment of LGV, particularly for men who have sex with men and for people with HIV infection.
- When contraindications to doxycycline are present, azithromycin should be the therapeutic choice.
- When no other treatment options are available, erythromycin 500 mg orally four times a day for 21 days is an alternative.
- Doxycycline should not be used in pregnancy.
Infant disease:
Oral erythromycin is the preferred treatment for both conjunctivitis and pneumonia in the neonate. Azithromycin is an acceptable alternative. Infants who fail an initial course of erythromycin are recommended to retreat with another fourteen-day course of erythromycin.
- Erythromycin 50 mg/kg by mouth in 4 divided doses for 14 days or
- Azithromycin 20 mg/kg by mouth daily for 3 days
Toxicity and Adverse Effect Management
In neonates being treated for chlamydial infection, both azithromycin and erythromycin are associated with a risk of infantile hypertrophic pyloric stenosis. This is particularly a concern for infants two weeks old or younger. Parents and physicians should observe infants closely for any signs of intestinal obstruction.
Prognosis
Antibiotic treatment has a 95% effectiveness rate for first-time therapy. The prognosis is excellent with prompt initiation of treatment early and with the completion of the entire course of antibiotics. Although treatment failures with primary therapies are quite rare, relapse may occur. Reinfection is common and is usually related to the nontreatment of infected sexual partners or acquisition from a new partner. Death is rare but can be caused by progression to salpingitis and tubo-ovarian abscess with rupture and peritonitis. The most significant morbidity occurs with repetitive infection with chlamydiae, which leads to scarring of the fallopian tubes and subsequent sterility.
Complications
Pelvic inflammatory disease confers a risk of ectopic pregnancy in women of childbearing age. Inflammation and scarring of the upper genital tract may also affect fertility or lead to chronic pelvic pain. Chlamydial infection in pregnancy can also increase the risk of prelabour rupture of membranes (PROM), premature prelabour rupture of membranes (PPROM), and preterm delivery.[13]
Deterrence and Patient Education
Asymptomatic infection with Chlamydia trachomatis is very common, whereas the consequences of undiagnosed or untreated infection can be far-reaching. It is for these reasons that screening is recommended. All pregnant women are recommended to be screened for C. trachomatis. All sexually active females younger than 25 should be screened annually. Women older than 25 should be screened if they have risk factors for sexually transmitted infections. Risk factors include sexual partners with multiple concurrent partners, new or multiple sexual partners, inconsistent use of condoms if the relationship is not monogamous, exchanging sex for money or drugs, or previous/coexisting STI. Men who have sex with men should also be screened for chlamydial infection. In individuals with HIV, screening should be done at the initial presentation and annually. For individuals entering a correctional facility, it is recommended to screen for chlamydia in women 35 years old or younger and men thirty years old or younger.
In the United States, C. trachomatis is considered a notifiable infection. Local and state laws regarding disease reporting apply. Sexual partners should be notified, examined, and treated if an STI is found in the index patient. Expedited partner therapy may also be available in certain settings. Expedited partner therapy allows providers to prescribe antibiotics to sexual contacts without establishing a physician-patient relationship.
Patients should be educated regarding the potentially serious consequences of chlamydia infections and the importance of screening. Patients also should be educated that screening can often be performed non-invasively with urine samples. Educated patients may then be agreeable to screening when they would otherwise hesitate out of fear of an uncomfortable exam.
Enhancing Healthcare Team Outcomes
In the United States and other developed countries, the prevention of sexually transmitted genital infections and complications mainly focuses on screening and treating nonpregnant sexually active women aged 25 years or younger on an annual basis. Screening for pregnant women is recommended, and screening and treatment of women over 25 years of age are recommendations if there are identifiable risk factors, such as new or multiple sexual partners. Screening of young men in high-risk settings (sexually transmitted infection and adolescent clinics, correctional facilities) should be a consideration if resources allow. Urine or endocervical NAAT are the recommended screening tests. The partner should be screened and treated at the same time.
Healthcare workers and nurse practitioners should educate patients on the importance of using a condom during sex, practicing safe sex or abstaining from sexual activity to prevent chlamydia.
Pharmacists should verify dosing and agent selection for antimicrobial therapy, check for drug interactions, and report any concerns to the prescriber.
The prognosis is excellent with prompt initiation of treatment early, and with the completion of the entire course of antibiotics, antibiotic treatment is 95% effective for first-time therapy.
No vaccine is currently available for either trachoma or chlamydial genital infections.
The healthcare team, including clinicians, nurses, and pharmacists, must work together to educate the patient on methods to avoid exposure and the importance of completing treatment. This approach will result in decreased incidence and improve outcomes. [Level 5]