Introduction
The D-dimer is a by-product of the blood clotting and break-down process that can be measured via analysis of a blood sample. D-dimer is released when a blood clot begins to break down.[1][2][3]
More specifically, platelets in the blood are connected to a D subunit. When blood clots form, the D group between two platelets form a bond. Many platelets bound together via D-Dimers (along with other factors, such as fibrin) form a clot. As part of the healing process of the body, clots that are formed begin to break down almost as soon as they are formed. When the clot bonds break, the D-dimer (D==D) breaks apart from the platelet (P):
D--P--D + D--P--D → D--P--D==D--P--D → D--P + D==D + P--D
Sensitivity and specificity vary based on the type of assay ordered. However, D-dimers have a high sensitivity but low specificity for detecting pulmonary embolism or deep vein thrombosis in low-risk populations.
Specimen Collection
Blood is collected from the patient via phlebotomy into a sodium citrate-containing vial and inverted to mix to preserve the blood sample for analysis by the lab.
Potential Diagnosis
Potential diagnoses include pulmonary embolism (PE), deep vein thrombosis (DVT), or disseminated intravascular coagulation (DIC).
Normal and Critical Findings
A normal D-dimer is considered less than 0.50. A positive D-dimer is 0.50 or greater. Since this is a screening test, a positive D-Dimer is a positive screen.[4][5][6][7] There is not necessarily a critical level for a D-dimer.
Interfering Factors
False negatives and false positives can occur. Due to the incidence of false negatives, a D-dimer should only be used in the setting of low suspicion for pulmonary embolism (PE) or low suspicion for deep vein thrombosis (DVT) and also known as venous thromboembolism (VTE). It also plays a role in the workup of disseminated intravascular coagulation (DIC).[8][9] Of note, there are several physiologic states or medical conditions that may cause patients to have an elevated D-dimer in the absence of PE, DVT, or DIC. These include but are not limited to pregnancy, malignancy, cigarette smoking, trauma, or infection, or sepsis. Furthermore, elderly patients, immobilized patients, patients with autoimmune disorders, or those who have had recent surgery may have an elevated D-dimer. Of note, there is emerging research to suggest using age-adjusted cut-off values for D-dimers, as a D-dimer can increase with age, even in the absence of pathology.
Clinical Significance
D-Dimer for Pulmonary Embolism (PE)
A pulmonary embolism refers to a blood clot located within the pulmonary vasculature resulting in a decrease in blood flow downstream of the clot. While some patients can have small pulmonary emboli that cause few symptoms, others can have large pulmonary emboli blocking the main pulmonary artery or arteries. When a pulmonary embolism is located in the main pulmonary arteries bilaterally, it is referred to as a saddle embolus. A patient with a saddle embolus is at high risk of cardiopulmonary arrest and death. Obtaining a D-dimer can help in exploring the differential diagnosis in patients who present with symptoms or signs such as chest pain, shortness of breath, or hypoxia.
Based on the Wells Criteria, patients can be risk-stratified into low-risk, moderate-risk, or high-risk for PE. The Wells Criteria takes into account various risk factors or symptoms of PE, including signs or symptoms of deep vein thrombosis (DVT), clinical suspicion for PE, the presence of tachycardia, recent immobilization (recent surgery), previously diagnosed PE or DVT, hemoptysis, and malignancy. Another scoring system is the Geneva Score or revised Geneva Score (rGeneva). It classifies patients as low-risk, intermediate-risk, or high-risk for PE. This score takes into account patient age (if older than 65 years), previous PE or DVT, recent surgery or lower extremity fracture, active malignancy, hemoptysis, unilateral extremity subjective pain, unilateral extremity tenderness to palpation, and elevated heart rate.
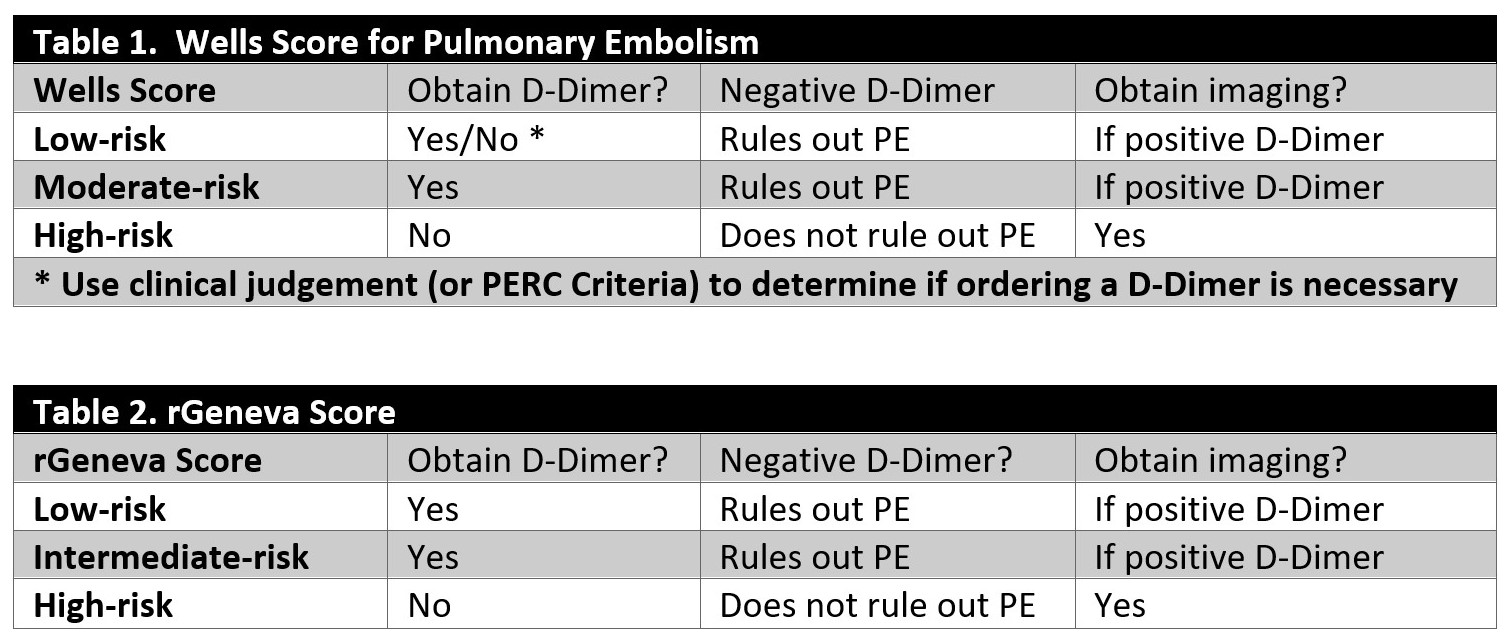
Regarding whether or not to order a D-dimer after you have scored a patient with Wells Criteria or Geneva/rGeneva scores and what to do with results, please see attached Tables 1 and 2.
In summary, though, a D-dimer should be ordered on low-risk patients, and a negative D-dimer can reasonably rule out PE in low-risk patients. In high-risk patients (which includes those in whom you have high clinical suspicion for PE), imaging should be obtained rather than going through the D-dimer as a screening test. In moderate-risk patients, one can either obtain a D-dimer (negative D-dimer would rule out PE) or go straight to imaging if clinical suspicion remains high.
Imaging for further evaluation in the case of a patient who is high-risk for PE or a patient that has a positive D-dimer should include either a CT angiogram or ventilation-perfusion scan.
There is an additional scoring system designed to rule out pulmonary embolism in those who are determined to be at low risk for PE called the Pulmonary Embolism Rule-Out (PERC) rule. If a patient does not have any of the characteristics or signs listed on the PERC rule, one need not obtain a D-dimer to rule out PE. Eliminating the need for obtaining a D-dimer in these patients will decrease the number of false positives and thus decrease the number of patients necessitating radiation exposure for radiographic rule out of pulmonary embolism.
D-Dimer for Deep Vein Thrombosis (DVT)
A DVT is a blood clot located in the deep venous system in the arms or legs. They are most commonly located in the legs. Symptoms of DVT can include erythema, pain, swelling, and increased warmth of the affected extremity. There is also a risk-stratification score for DVT, which is the Wells Criteria for DVT. This scoring system considers recent malignancy, recent immobilization (including recent surgery), asymmetric leg swelling, the presence of collateral veins, tenderness along the location of suspected vein, previously diagnosed DVT, and high clinical suspicion for DVT. With this scoring system, one can either be classified as DVT “likely” or “unlikely” or further divided into low-risk, moderate-risk, or high-risk. Either way, a DVT can be ruled out with a negative D-Dimer in the low-risk or “unlikely” groups. In the moderate-risk, high-risk, or “likely” groups, a positive D-Dimer necessitates imaging with Ultrasound to evaluate for DVT. Again, however, if there is high clinical suspicion for DVT, one can order an ultrasound without obtaining a D-Dimer.
D-Dimer for Disseminated Intravascular Coagulation (DIC)
Disseminated intravascular coagulation results from a problem with the coagulation cascade. This can either lead to excessive clot formation if it evolves slowly or to bleeding if the process is acute in onset. DIC has a high rate of mortality. A D-dimer is among the many different studies that can be ordered in the diagnostic workup of DIC. A D-dimer will be significantly elevated if a patient is in DIC. Other labs one might consider ordering would include fibrinogen (depressed to normal), platelet count (low), PT/INR (normal to prolonged), and PTT (normal or elevated). These labs can also help one monitor response to treatment of DIC as they should trend back toward normal values with improvement and hopefully DIC.