Continuing Education Activity
Erysipelas is a skin infection involving the dermis layer of the skin, but it may also extend to the superficial cutaneous lymphatics. It is characterized by an area of erythema that is well demarcated, raised, and often affects the lower extremities, with the face being the second most commonly affected site. This activity reviews the cause and presentation of Erysipelas and highlights the role of the interprofessional team in its management.
Objectives:
- Recall the cause of erysipelas.
- Describe the presentation of erysipelas.
- Summarize the treatment options for erysipelas.
- Outline the importance of coordination among interprofessional team members to improve outcomes for patients affected by erysipelas.
Introduction
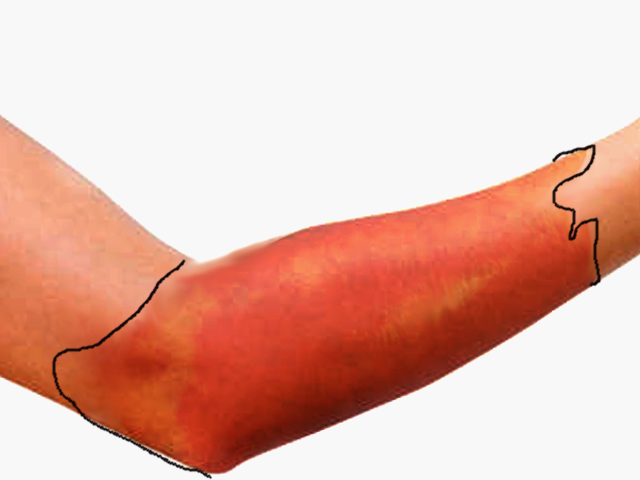
Erysipelas is a skin infection involving the dermis layer of the skin, but it may also extend to the superficial cutaneous lymphatics. It is characterized by an area of erythema that is well-demarcated, raised, and often affects the lower extremities, with the face being the second most commonly affected site. Erysipelas is also referred to as “St. Anthony’s Fire” due to its intense fiery rash. Its diagnosis can overlap with cellulitis, and often a definite diagnosis cannot be made. Cellulitis has ill-defined borders and is slower to develop, while erysipelas has better-defined borders and faster development. Erysipelas can be serious but rarely fatal. It has a rapid and favorable response to antibiotics. Local complications are more common than systemic complications.
The most common cause is group A streptococci.
Etiology
The primary inciting infection involves streptococci. Most facial infections are due to Group A streptococcus while non-group A streptococcus involves more of the lower extremity. In a prospective study in Norway, researchers concluded that beta-hemolytic streptococci were the leading cause of facial cellulitis.[1] In neonates, Group B streptococcus is the leading cause of postpartum erysipelas. Erysipelas starts with skin breaks and leads to the inoculation of the eliciting bacteria. Surgical incisions, insect bites, stasis ulcerations, and venous stasis are among the many entry portals. In addition, facial erysipelas may be caused by a recent infection in the nasopharynx passage.
There is little supporting evidence that staphylococcus plays a role in erysipelas. [2]
Risk factors for erysipelas include the following:
- Excising the saphenous vein for bypass
- Lymphatic edema (major risk factor)
- Lymphatic obstruction
- Arteriovenous fistula
- Status post-surgery (eg mastectomy)
- Nephrotic syndrome
- Immunocompromised state
Epidemiology
Most epidemiological studies on erysipelas have been done in different inpatient settings, across different countries. Erysipelas can affect people of all age groups, races, and sex. Some studies showed that erysipelas is more common in females. The incidence of erysipelas has decreased since the development of antibiotics and improved sanitation. Erysipelas can affect all age groups but is most common in the extremes of age. [3]
Pathophysiology
Skin infection spreads through a break in the skin, directly invading the lymphatic system and causing erysipelas. Insect bites, stasis ulceration, surgical incisions, and venous insufficiency have been reported as portals of entry to the skin. Some risk factors that predispose people to develop erysipelas are obesity, lymphedema, athlete’s foot, leg ulcers, eczema, intravenous drug abuse, poorly controlled diabetes, and liver disease. Recurrent erysipelas has also been reported, with the infection typically reoccurring in the same site. [4]
Histopathology
This histopathology will reveal significant vascular dilatation, dermal edema and invasion of bacteria into the lymphatics and connective tissue. Blood vessel invasion is rare.
History and Physical
Erysipelas remains a clinical diagnosis, and assessing a patient for any recent skin trauma or pharyngitis is important. Patients often experience systemic symptoms, such as malaise, fever, and chills 48 hours before the onset of the skin lesion. It has been well described that erysipelas presents as an area of skin erythema that is sharply demarcated with raised edges. Often patients will complain of burning, tenderness, and itchiness at the site. More severe disease can present with vesicles, bullae, and even frank necrosis.
The location of inflammation is very important. In lower extremity erysipelas, it is recommended to examine the interdigital toe spaces for fissures, scaling, or maceration. Redness and swelling involving a joint should raise suspicion for other more serious disease processes like septic arthritis.
Evaluation
No laboratory workup is required for the diagnosis of erysipelas. Leukocytosis, elevated ESR and C-reactive protein are common but will not change the management or the treatment plan for most otherwise healthy individuals. Blood cultures have a low yield and are not routinely obtained; however, consider blood work and culture in the immunocompromised, ill-appearing patient. Also, consider extensive workup in patients who may be intravenous drug abusers, patients with prosthetic heart valves, and those with other intravascular devices. Patients who are septic will require full workup and resuscitation.
Treatment / Management
Antibiotics against streptococci should be initiated when erysipelas is suspected. Penicillin as monotherapy remains the first-line antibiotic used for the treatment of erysipelas. Coverage against MRSA is controversial. The 2014 Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections[5] recommend coverage against methicillin-resistant Staphylococcus aureus (MRSA) in patients “whose cellulitis is associated with penetrating trauma, evidence of MRSA infection elsewhere, nasal colonization with MRSA, injection drug use, or SIRS.” Most patients with erysipelas can be discharged home on oral antibiotics. The recommended duration of antibiotic therapy is 5 days, but the period may be extended to 10 days if the infection does not improve. Hospitalization is recommended for concern of necrotizing infection, the immunocompromised, patients with poor adherence to medications and follow up, and for those whose outpatient treatment is failing.
A Cochrane review published in 2017, reviewed 5 trials assessing the prevention of recurrent episodes of cellulitis and erysipelas. They concluded that patients who were on preventative treatment with antibiotics, particularly penicillin, had a decreased risk of future episodes by 69%. In a retrospective study done in Prague, they have found that Benzathine penicillin G 1.2 MU once every 3 weeks was effective prophylaxis for recurrent erysipelas; however, they could not conclude the needed appropriate duration of prophylaxis treatment.[6] The 2014 practice guidelines for the diagnosis and management of skin and soft tissue infections recommend oral penicillin or erythromycin twice a day for 4 to 52 weeks, or intramuscular benzathine penicillin every 2 to 4 weeks, in patients who have 3 to 4 episodes of cellulitis per year, despite attempts to treat or control predisposing factors.
Other supportive treatments include hydration, cold compresses, acetaminophen for fever and extremity elevation.
If there is evidence of an abscess or gangrene, surgical debridement is necessary. Admission is usually required for infants, elderly and immunocompromised individuals.
Differential Diagnosis
There are diseases that can mimic erysipelas [7]; all of which present with erythema, warmth, edema, and pain. Some of the more serious diagnoses include septic bursitis, septic arthritis, necrotizing fasciitis, orbital cellulitis, deep vein thrombosis, phlegmasia cerulea dolens, flexor tenosynovitis, and toxic shock syndrome. Less serious diagnoses include cellulitis, abscess, felon, gout, and paronychia.
Prognosis
Generally, the prognosis of erysipelas is good and can be managed in the outpatient setting. It responds well to oral antibiotics. However, extra caution should be taken in the immunocompromised and those with poor adherence to medication. Hospitalization for intravenous antibiotics is recommended in severe cases affecting those who are immunocompromised, infants, and the elderly. Close monitoring and observation are also recommended for those who will most likely not comply with instructions or complete their antibiotic course secondary to psychological or social reasons.
Complications
Complications of erysipelas can be serious but rarely fatal. Some local complications include abscess formation, scarlet fever, pneumonia, meningitis, skin necrosis, hemorrhagic purpura, thrombophlebitis, and bullous formation. There has been a case report of erysipelas leading to bilateral lower limb and abdominal elephantiasis secondary to erysipelas.[8] A retrospective study of 152 cases of erysipelas evaluated for risk factors associated with local complications. They reported that prior empirical antibiotics and increased ESR at the time of admission were independent risk factors for the development of local complications of erysipelas.[9]
Local recurrence is reported in 5-20% of patients and can lead to scarring.
Deterrence and Patient Education
Patients should wear compression stockings if the extremity is affected. In some patients long term antibiotic therapy is required for cure.
Enhancing Healthcare Team Outcomes
Erysipelas is commonly encountered by the primary care provider and nurse practitioner. The diagnosis in most cases is clinical but if there is any doubt, the patient should be referred to a dermatologist. The infection does respond to antibiotics and patients are usually managed as outpatients. Hospitalization is recommended for concern of necrotizing infection, the immunocompromised, patients with poor adherence to medications and follow up, and for those whose outpatient treatment is failing. An infectious disease or wound care nurse should follow these patients to ensure cure. Those who undergo surgery for an abscess or gangrene may require long term wound care. The pharmacist should encourage medication compliance. The team should communicate with each other to ensure that the patient is responding to therapy.
The outcomes for patients with erysipelas are good as long as they remain compliant with antibiotic treatment.[10] (Level V)