Introduction
The muscles of the eye are integral to its function and motion. Muscles directly associated with the eye include the extraocular muscles which control the external movement of the eye; the intraocular muscles, which are responsible for pupil accommodation and reaction to light; and the protractor and retractors of the eyelids. Deficits in the muscles or the nerves innervating these muscles can result in functional impairment of the involved structures.
Structure and Function
The intraocular muscles include the ciliary muscle, the sphincter pupillae, and the dilator pupillae.[1] The ciliary muscle is a smooth muscle ring that controls accommodation by altering the shape of the lens, as well as controlling the flow of aqueous humor into Schlemm's canal. The ciliary muscle is attached to the zonular fibers, which suspend the lens. Upon contraction of the ciliary muscle, the tension on the lens becomes lessened, which causes it to adopt a more spherical shape to focus on near objects. Relaxation of the ciliary muscle has the opposite effect, optimizing distant focus. The sphincter pupillae and dilator pupillae are also composed of smooth muscle. The sphincter pupillae encircles the pupil and is responsible for the constriction of its diameter, while the dilator muscle is arranged radially and increases the pupillary diameter.
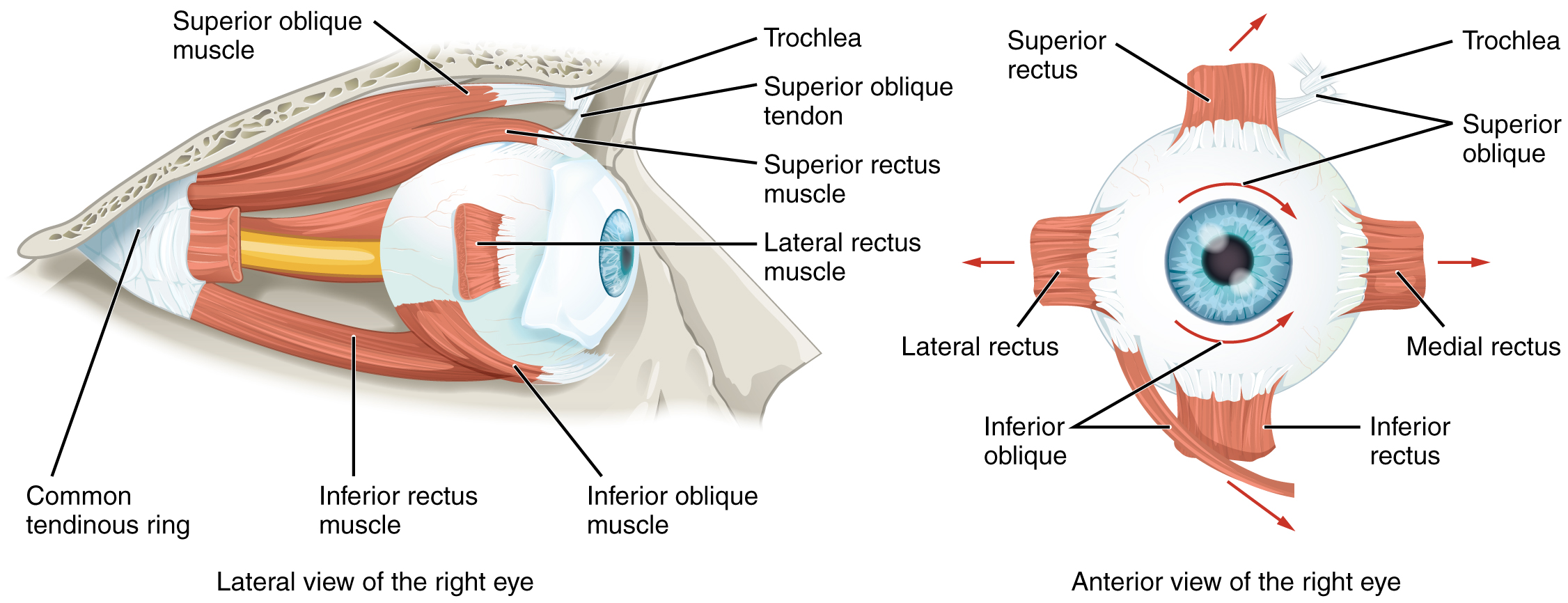
There are three primary axes of ocular movements: vertical, transverse, and anteroposterior. Rotation around the vertical axis results in either adduction (medial movement) or abduction (lateral movement) of the eye. Rotation around the transverse axis causes elevation (superior motion) or depression (inferior motion). The anteroposterior axis enables the movement of the superior pole of the eye medially (intorsion) or laterally (extorsion). The rotations around the anteroposterior axis allow the eye to adjust to the tilting of the head.
The medial rectus muscle is responsible for medial rotation around the vertical axis, and the lateral rectus lateral rotation. The superior rectus muscle primarily elevates the eye and contributes to adduction and intorsion. The inferior rectus depresses and laterally rotates the eye and contributes to adduction and extorsion. The superior oblique abducts, depresses, and medially rotates the eye, while the inferior oblique abducts, elevates, and laterally rotates the eye. The four rectus muscles originate from the Annulus of Zinn and are approximately 40mm in length. They insert onto the sclera a few millimeters from the limbus. The inferior oblique originates from the orbital floor and inserts on the sclera in the inferotemporal globe. The superior oblique originates in the posterior orbit and travels medially before inserting on the sclera in the superotemporal globe.[1]
The primary retractor of the upper eyelid is the levator palpebrae superioris, which is a skeletal muscle. The superior tarsal muscle (Müller's muscle) is comprised of smooth muscle and also contributes to the elevation of the upper eyelid. In the lower eyelid, the retractors are the capsulopalpebral fascia and the inferior tarsal muscle. The orbicularis oculi muscles are the main protractors (closure) of the eyelids. It is a flat, ringlike band of skeletal muscle surrounding the anterior orbit composed of three parts: the orbital portion, the palpebral portion, and the lacrimal portion.
Embryology
The ciliary muscle and both pupillary muscles are cranial neural crest derivatives and develop from the mesenchyme of the choroid.
The extraocular muscles, including the levator palpebrae superioris, are derivatives of periocular mesenchyme. Five of the six extraocular muscles originate at the annulus of Zinn (a tendinous ring), while the inferior oblique originates on the orbital portion of the bony maxilla. The annulus of Zinn overlies the superior orbital fissure and the optic foramen.[2] Three patriotic somites found anterior to the developing ear of the embryo are responsible for the development of the extraocular muscles. These three somites correspond with the distribution of cranial nerves III, IV, and VI.
The orbicularis oculi derive from mesenchyme of the second pharyngeal arch, and forms from mesoderm of the eyelid.
Blood Supply and Lymphatics
The majority of the blood supply to the orbit is supplied by the ophthalmic artery, which branches off of the internal carotid artery. A branch of the external carotid artery, the infraorbital artery, also contributes blood supply to the orbital floor. There are many branches of the ophthalmic artery, including the central retinal, supraorbital, supratrochlear, lacrimal, dorsal nasal, short posterior ciliary, long posterior ciliary, posterior ethmoidal, anterior ethmoidal, and anterior ciliary (off of the muscular branches of the ophthalmic artery) arteries. Except for the central retinal artery and the ciliary arteries, which supply intraocular structures, these branches, as well as the infra-orbital artery off of the external carotid, all contribute to the vascular supply of the extraocular muscles and structures. The superior and inferior ophthalmic veins are responsible for venous drainage of the orbit.
The existence and location of orbital and eyelid lymphatics are a current area of ongoing research and debate.
Nerves
The extraocular muscles are innervated by nerves that enter the orbit through the superior orbital fissure. The oculomotor nerve (CN III) divides into superior and inferior branches and innervates the superior, medial, and inferior recti, the levator palpebrae superioris, and the inferior oblique. It also carries presynaptic parasympathetic fibers to the ciliary ganglion. Sympathetic fibers of CN III contribute to upper eyelid retraction by innervation of the superior tarsal muscle (Müller's muscle). The trochlear nerve (CN IV) innervates the superior oblique, and the lateral rectus receives innervation from the abducens nerve (CN VI). Innervation to the orbicularis oculi is by the temporal and zygomatic branches of the facial nerve (CN VII).
The ophthalmic nerve (branch of CN V1) branches into the frontal, nasociliary, and lacrimal nerves. The ciliary ganglion is made up of postsynaptic parasympathetic nerve cell bodies associated with the ophthalmic nerve. The short ciliary nerves originate from the ciliary ganglion and carry parasympathetic and sympathetic fibers to the iris and ciliary body. The long ciliary nerves branch off of the nasociliary nerve and carry postsynaptic sympathetic fibers to the dilator pupillae and afferent fibers from the cornea and iris. The sphincter pupillae is parasympathetically-stimulated while the dilator pupillae is sympathetically-stimulated.
Surgical Considerations
Strabismus surgery is performed on the extraocular muscles and aims to correct the misalignment of the eyes. The main types of strabismus surgery involve loosening or weakening, tightening or strengthening, and transposition or repositioning. Permanent or adjustable sutures are both options. Adjustable suture surgery involves the placement of a stitch that can be shortened or lengthened during a short period following the surgery to adjust for proper alignment. Loosening procedures include recession or the movement of the insertion of an ocular muscle posteriorly toward its origin, tenotomy, tenectomy, myotomy, and myectomy. Tightening procedures include resection in which a distal portion of the ocular muscle is removed before reattachment of the muscle to the eye, advancement of the muscle insertion to a more anterior position, and tucking.
Clinical Significance
Strabismus occurs when the eyes are misaligned such that an object is not focused simultaneously on the fovea of each eye. A phoria is defined as the turning of an eye in (esophoria) or out (exophoria) upon occlusion of the opposite eye. Phorias are often asymptomatic but may degenerate into tropias. Tropia is a spontaneous eye turn in the absence of an ocular occlusion. Tropias are often more prevalent with tiredness as phorias become more pronounced, and the ability to compensate decreases. Certain drugs can result in temporary tropias.[3]
Amblyopia results when the vision in one of the eyes becomes reduced because the eye and the brain are not working together correctly. Strabismic amblyopia is the result of eye misalignment and is treated initially by patching the good eye to force the child to use the amblyopic eye, and may ultimately require strabismus surgery. After age five, it is difficult to reverse amblyopic vision.[4]
Extraocular muscle paralysis can occur due to disease or injury and may involve one or multiple muscles.[5] Oculomotor nerve palsy affects the majority of the extraocular muscles, as well as the sphincter pupillae and the levator palpebrae superioris. CN III palsy presents with a "down and out" positioning of the eyeball of the affected side with a fully dilated and non-reactive pupil. Abducens nerve palsy affects only the lateral rectus muscle. It presents as an inability to abduct the eye on the affected side, with the eye reverting to an adducted position due to the unopposed pull of the medial rectus.[6][7][8][9][10]