Continuing Education Activity
Restoration of satisfactory digital function after an unrepaired flexor tendon laceration or failed repair remains one of the most challenging clinical and operative dilemmas in hand surgery. This article will review the anatomic relationships of flexor tendons within the hand, describe associated intricacies of hand physiology, explain the critical components of a thorough hand examination in diagnosing flexor tendon injuries, highlight diagnostic modalities and adjuncts, and summarize operative principles correspondent to various zones of flexor tendon injuries while outlining the optimal healthcare team relations and establishing individualized postoperative rehabilitation protocols for enhanced patient outcomes.
Objectives:
- Review the anatomic relationships of flexor tendons within the hand and describe the associated intricacies of hand physiology.
- Explain the key components of a thorough hand examination in diagnosing flexor tendon injuries; highlight diagnostic modalities and adjuncts to flexor tendon injury diagnoses.
- Summarize operative principles corresponding to various zones of flexor tendon injuries.
- Outline the optimal healthcare team inter-relations in treating flexor tendon injuries and establish individualized postoperative rehabilitation protocols to enhance patient outcomes.
Introduction
Since initial reports suggesting primary tendon repair as possible and even desirable emerged in the 1960s, significant advancements in the understanding of flexor tendon anatomy, biology, mechanisms of response to injury, and methods of repair, have been made. Recent research highlights enhanced improvements in operative techniques and rehabilitative care that have made primary flexor tendon repair a preferred operative approach for lacerations and can successfully achieve a reliable flexor tendon repair site, optimizing digital motion. The formative goals of surgical treatment for lacerated flexor tendons have remained constant: accurate smooth coaptation of tendons ends to allow application of a postoperative rehabilitation protocol that encourages tendon gliding, prevents peritendinous adhesion formation without gapping, stimulates gliding surface restoration while optimizing opportunity for primary site healing, and ultimately, achieves satisfactory strength to allow early range of motion to the finger.
Flexor digitorum profundus (FDP), flexor digitorum superficialis (FDS), and flexor pollicis longus (FPL) muscles power flexion of the fingers and thumb. Within the forearm, FDS tendons share a common muscle belly, while each FDP tendon has its own individual muscle belly. At the metacarpal head (Camper’s chiasma), FDS tendons divide into two halves, where then each head rotates laterally (180 degrees) around the associated FDP tendon. FDS then slips dorsally to rejoin the opposite head deep to the FDP tendon at the distal aspect of the proximal phalanx, prior to volarly and laterally inserting on the middle phalanx as two separate slips.
- FDS tendons flex the proximal interphalangeal (PIP) joints. FDS originates from the medial epicondyle, coronoid process of the ulna, and proximal shaft of radius and inserts on the middle phalanx. The median nerve innervates FDS; its vascular source is from the radial and ulnar arteries.
- FDP originates on the proximal ulna and interosseous membrane and inserts on the volar base of the distal phalanx. FDP tendons flex the distal interphalangeal (DIP) joint. While the FDP tendons of the index and middle fingers are innervated by the anterior interosseous branch of the median nerve, the ring and small finger FDP tendons are innervated by the ulnar nerve. Blood supply to FDP is mainly from the ulnar artery.
- FPL flexes the thumb interphalangeal (IP) joint. FPL originates from the proximal radius, radial head of the interosseous membrane, and medial epicondyle or accessory head of the coronoid process. It inserts on the volar base of the thumb distal phalanx. FPL is innervated by the anterior interosseous nerve branch of the median nerve. Blood supply is predominantly from the radial artery.
In the distal forearm, the most superficial FDS tendons to long and ring fingers overlay the FDS tendons to index and little fingers. In the deeper layers remain 4 FDP tendons and FPL. The relationship between these nine digital flexors remains relatively constant in their orientation and relationship as they enter the proximal aspect of carpal tunnel.
Each of the tendons mentioned above lies within a tendon sheath, subsequently reinforced by thickened areas known as pulleys, which hold tendons close to the phalanges at all positions through extension and flexion. Pulleys permit tendon excursion while maximizing mechanical competence and improving the overall efficiency of the flexor apparatus. Each layer of the pulley system has a strategic purpose: the innermost secrete hyaluronic acid is designed to facilitate gliding, the middle is rich in collagen to resist palmar translation, and the outer facilitates nutrition of the pulley system. There are five annular (A) pulleys and three cruciate (C) pulleys. Odd-numbered A pulleys are at the joint level: A1 at the metacarpophalangeal (MP) joint, A3 at the PIP joint, and A5 at the DIP joint. The A2 pulley is at the proximal portion of the proximal phalanx, and the A4 pulley lies at the middle portion of the middle phalanx. A2 and A4 pulleys are the most critical components for proper flexor function; injury to either of these precludes bowstringing of the flexor tendon. The pulley system within the thumb is unique in that it only contains two annular pulleys (A1, A2) and an intervening oblique pulley. Injury to the oblique pulley within the thumb can lead to bowstringing of the FPL tendon, as it is an extension of the adductor pollicis aponeurosis.[1]
The fingers and thumb flexor tendon zones can be subdivided via universal nomenclature called Verdans, initially developed by Kleinert and colleagues, and Verdan; repair techniques and prognoses vary within each zone.
- Five zones for fingers:
- Zone 1 - distal to FDS insertion; only the FDP resides here
- Zone 2 - from A1 pulley (proximally) to FDS insertion (distally) (within the sheath = “no man’s land”); contains both FDS and FDP
- Zone 1 & Zone 2 are described by the fibro-osseous digital sheath. Within this sheath, the tendons are covered by a layer of flattened fibroblasts termed epitenon - a crucial gliding surface that must be restored for flexor tendon repair to be successful.
- Zone 3 - from the distal end of carpal tunnel to A1 pulley; denotes the origin of lumbricals from FDP
- Zone 4 - within the carpal tunnel, under the flexor retinaculum
- Zone 5 - proximal to the carpal tunnel[1][2]
- Five zones for thumb:
- Zone T1 - distal to interphalangeal (IP) joint
- Zone T2 - from A1 pulley to IP joint
- Zone T3 - over the thenar eminence
- Zone T4 - within the carpal tunnel
- Zone T5 - proximal to carpal tunnel
Etiology
Hand injuries constitute approximately 20% of emergency room visits.[3] Flexor tendon injuries frequently complicate lacerations to the palmar surface of the digit and hand and can be subcategorized as partial lacerations, complete lacerations, and tendon avulsion injuries. Flexor tendon injuries can occur secondary to a sharp object (i.e., glass or knife) or result from blunt trauma in strength-based sports (i.e., football, basketball, wrestling), where injuries occur at tendinous attachments to the bone.[3] In developed and industrialized countries, flexor tendon injuries may occur more commonly following workplace accidents. In contrast, regions of lower socioeconomic levels see flexor tendon injuries resulting from knife or glass incisions secondary to quarrels.[3]
Dependent upon the severity and degree of laceration, patients may present with loss of active digital flexion or painful digital flexion. Decreased or absent digital sensibility and motor strength can also be appreciated. Closed injuries associated with loss of finger motion often present with a loss of distal interphalangeal (DIP) joint movement following injury. A painful nodule in the region of tendon retraction may be appreciated in patients with closed tendon avulsion injuries. Flexor tendon injuries occur in greater prevalence within zones II-V, most commonly in the index or small finger.[3][4]
Epidemiology
The epidemiology of flexor tendon injuries is not well understood; however, they remain a causative injury of significant morbidity throughout the working-aged (20 to 45 years) young male population. They are frequently known to involve nerve injuries. The dominant hand is affected more often than the non-dominant hand and is usually injured when using a sharp object or catching a falling object.[4]
Flexor tendon injuries occur at an estimated rate of 30 to 42 per 100,000 persons, accruing a total direct and indirect cost of tendinous injuries within the United States alone of $240 to $409 million.[5]
Histopathology
The histologic basis of tendons is formed via a biological interplay of elastin and mucopolysaccharides that provide the ground substance, further composed of specialized fibroblasts called tenocytes, containing type I collagen as a matrix.
Endotenons are fascicular arrangements with bundles of tenocytes and collagen fibers held together by a fine layer of connective tissue. Epitenon describes septa of endotenon joined together externally to form fibrous outer layers. Paratenons are tendons covered by a loose layer of adventitial tissue proximal to the tendon sheath.
Tendon healing can be divided into intrinsic and extrinsic components. Intrinsic healing involves the tenocytes within the tendon, on the epitenon layer. The inflammatory cells and fibroblasts from the overlying sheath are implicated in extrinsic healing. The extrinsic healing component is the purported culprit of adhesion formation between the tendon and its sheath. Like other variations of wound healing, tendon repair progresses through 4 phases: hemostasis, inflammation, proliferation, and remodeling. Although earlier stages see greater quantities of type III collagen, type I collagen dominates as healing progresses.[3]
Each flexor tendon has a proximal region that is extrasynovial and a distal region that is intrasynovial. It is known that well-vascularized extrasynovial tendons (flexor tendons of the wrist and forearm - zones III, IV, and V) typically exhibit a robust wound-healing process following injury and subsequent repair, achieving 85-100% of normal digital motion with a low incidence of tendon rupture. This phenomenon is secondary to extrasynovial tendinous enrichment of inflammatory inhibitors and oxidative phosphorylation enzymes that prompt a rapid neovascularization response and increased expression of complement proteins. In contrast, intrasynovial tendons (digital flexor tendons) demonstrate minimal vascularity with muted inflammatory and metabolic responses.[6]
Environmental factors, additionally, influence the healing capacity of connective tissues.
History and Physical
A thorough and detailed history and physical examination of the injured hand should be performed as part of the initial clinical assessment. Evaluation should be completed prior to administration of local anesthesia or sedation to accurately detect any potential neurological or vascular injury. Collecting a patient's history should include age, handedness, occupation, mechanism of injury (including how the hand was positioned during insult), time of injury, previous attempts at treatment, history of tobacco use, and tetanus vaccine/booster dose status.
Physical examination should characterize and document the location and depth of any/all wounds, evaluate the hand's resting position, assess the arterial supply to the digit, utilize a handheld Doppler probe when unable to obtain palpable pulses, and carefully perform neurological testing. Learning the finger position at the time of injury may provide insight into the position of the distal tendon stump. If the finger was in flexion during injury, the level of the tendinous insult would be distal to the associated skin laceration, while a finger injured in the extended position will reveal a tendon stump close to the overlying skin violation.
Evaluation
Detailed assessment mandates systemic examination, including complete integumentary, musculoskeletal, neurological, and vascular evaluations.
Integumentary: the integrity of overlying volar and dorsal skin should be examined to rule out or diagnose concomitant injuries, ensuring documentation of each skin injury.
Musculoskeletal: obvious angular or rotational deformities of the digits warrant further investigation for fracture or ligamentous injury, with appropriate realignment or reduction prior to evaluating flexor tendon integrity or neurovascular sequelae. Should a completely lacerated flexor tendon be appreciated, one could expect the digit to assume extension at the proximal interphalangeal (PIP) joint and distal interphalangeal (DIP) joint. Individual tendons should be inspected on each finger. Flexor digitorum profundus (FDP) can be isolated by blocking PIP flexion and assessing active DIP flexion, as FDP is the only flexor tendon to traverse the DIP joint. Flexor digitorum superficialis (FDS) is examined by preventing flexion of other digits and evaluating isolated PIP flexion, as all FDS tendons share a common muscle belly. Loss of digital flexion and normal “flexor cascade” (tenodesis effect) is consistent with complete tendon transection, where there is an absence of normal flexor tone with passive wrist extension. Painful digital flexion is suggestive of a partial tendon injury. FDP avulsion injuries may present with a clinically painful nodule indicative of a retracted tendon.
Neurological: sensation should be evaluated with static and moving 2-point discrimination tests before injecting a local anesthetic. Loss of sensation in a digital nerve distribution after sharp laceration portends a nerve transection until proven otherwise.
Vascular: capillary refill of the volar pulp and nail bed should be assessed. Delayed capillary refill or poor turgor suggests digital artery laceration. An Allen test can be performed in this circumstance.
Inquire as to the status of tetanus vaccination and the timeline since the last booster dose.
Obtaining anterior-posterior/lateral/oblique radiographs to rule out fractures or retained foreign bodies is a useful adjunct to primary history and physical examination. When the continuity of a flexor tendon is in question or to assess a suspected partial laceration, an ultrasound can be considered. Intraoperative fluoroscopic images may be utilized, pending the findings during surgical exploration.
Physical exam findings will often suggest the presence or absence of flexor tendon injury, conferring clinical correlation of the laceration, overlying skin injury, and/or mechanism, which could subsequently benefit from elective surgical exploration and possible repair. After a complete evaluation of the skin, skeleton, tendons, nerves, and vascular supply, judgment regarding the need, timing, and nature of surgical repair can be confidently formulated.
Treatment / Management
Before discussing surgical options and timing, it is important to note that not every flexor tendon laceration is expedited to the operating room on initial presentation. As patients present to the clinic, the emergency department, urgent care, or other primary settings, initial treatment usually consists of IV antibiotic administration, thorough debridement of the wound basin with the removal of foreign debris and inspection of tissue viability, followed by loose skin closure, appropriate splint application to limit proximal tendon retraction, and education on the importance of compliance with early follow-up.
Primary repair (<24 hours) is the preferred option when medically and surgically feasible. However, it is otherwise contraindicated in the setting of gross contamination, or when the injury is secondary to a human bite, there is obvious evidence of active infection (cellulitis, purulence, etc.), and/or there is a lack of stable soft tissue coverage.
Delayed primary repair (>24 hours, yet <2 weeks) constitutes a reasonable approach for heavily contaminated wounds and provides functional results comparable to initial primary repair.
Secondary repair can occur in either an early (2 to 5 weeks) or late (>5 weeks) fashion. Early repair within 2-5 weeks is performed before significant muscle contraction, with results similar to delayed primary repair. It is important to note the increased risk of infection and prolonged edema with progressive delay in definitive repair. Late secondary repair after five weeks is often faced with the presence of tendon edema and softening in the setting of a scarred flexor tendon sheath that reduces the likelihood of good tendon gliding. The best options for late repair are tendon graft or transfer, as repair is often inhibited by significant muscular contraction. Significantly, the FDP tendon may be advanced up to, but not more than, 1 cm; excessive advancement can induce a flexion deformity in the repaired digit which subsequently limits active flexion in adjacent digits.
Zone 1 injuries: FDP tendon laceration distal to the insertion of the FDS tendon or avulsion from its insertion at the base of the proximal aspect of the distal phalanx.
- Avulsion injuries or "Rugger jersey finger" are most common in young male athletes participating in contact sports during forced extension with maximal profundus contraction. The ring finger is most commonly involved, as it is the longest digit when the PIP joints are fully flexed. The following types of avulsion injuries are categorized under the Leddy classification:
- Type I - FDP retracts into the palm; requires repair within one week, as the myotendinous unit will shorten and the tendon will weaken without nutrition[7]
- There is a concomitant rupture of the vincula, compromising the blood supply[7]
- Type II - FDP tendon avulses with a small fragment of the distal phalanx, and the tendon retracts to the level of the PIP joint (A3 pulley); repair can be delayed up to 6 weeks[7]
- The long vinculum is spared, thus preserving bloody supply[7]
- Type III - large bony fragment is avulsed with the tendon to the level of A4 pulley and is prevented from retracting beyond the middle phalanx[7]
- Type IV - a combination of tendon avulsion from a fragment of tendon retraction and avulsion fracture of the distal phalanx ("double avulsion")
- If the tendon is lacerated and the distal tendon stump is <1 cm, FDP tendon advancement and primary tendon-to-bone repair is usually indicated; if >1 cm remains, primary tendon repair can be performed to avoid unnecessary shortening of the flexor tendon.
- Either suture anchors or pull-out button technique can be orchestrated, with several studies demonstrating superior arc of motion, patient-rated outcomes, lower complications, and shorter return to work following anchor repair versus buttons.[2][8] Furthermore, data has shown that anchors represent a biomechanically superior construct that can withstand the stresses of early active motion protocols.[9]
Zone 2 injuries: historically associated with poor results. Secondary to the risk of adhesion formation, the difficulties encountered during treatment, and the lack of satisfactory clinical outcomes, the term no man's land was originally used by Bunnell to describe zone 2 tendinous injuries. Most advocate repairing FDP and FDS should more than 60% of the cross-sectional tendon area be disrupted. However, in cases of massive injury (i.e., replantation), an FDP-only repair is acceptable. If emergent repair is not performed, the wound should be thoroughly irrigated and skin loosely approximated, with the administration of tetanus prophylaxis and antibiotics, following which it is advised the patient be placed in a dorsal splint. The repair can generally be completed up to 3 weeks following injury; however, delay in treatment beyond three weeks is associated with less satisfactory outcomes.
- It is imperative to restore the appropriate anatomic relationship in which FDP passes through slips of FDS. Repairing the FDS may warrant smaller sutures to decrease bulkiness and minimize trauma to the individual slips. In cases where a bulky repair does not permit gliding within the flexor sheath, one slip of the FDS can be excised without compromising results.
Throughout the literature, zone 2 injuries are most common, perhaps resulting from being the longest zone, confining tendons to a narrow area without protective tissues.[10][4] The high rate of complications is largely attributed to poor vascular supply. Adhesion formation is considered a sequela of the tight tunnel in which two tendons must pass.[2]
Zone 3 injuries: although the operative repair technique remains the same as for zone 2, the prognosis is better than for zone 2, with functional outcomes primarily dictated by the extent of associated nerve repair. Given its lack of sheath, zone 3 injuries generally preclude a good prognosis when not linked with neurovascular trauma.[2]
- Injuries to the deep motor branch of the ulnar nerve and/or deep palmar arch must be repaired before addressing flexor tendons.
- A lumbrical plus finger can result from repair in this region, secondary to excessive advancement, and results in paradoxical IP joint extension with attempted forceful flexion.
Zone 4 injuries: operative repair is similar to zone 2, with recommendations for transverse carpal ligament repair after tendon repair to prevent bowstringing. Most tendinous injuries are combined with median (as it is the most superficial structure in the carpal tunnel) or ulnar nerve injury; pure tendon injuries are rare, in part due to the protection of the flexor retinaculum. Direct tendon repair is the gold standard in zone 4 injury management.[2]
- If possible, tendons should be repaired proximal or distal to the carpal tunnel without releasing the transverse carpal ligament (TCL).
Zone 5 injuries: disability here is more commonly a sequela of associated median or ulnar nerve injury and results in more disability as opposed to isolated tendon injuries. Acute injuries within zone 5 may be repaired within three weeks, after which permanent shortening occurs, and reconstruction or tendon transfers may be required. The most crucial factor in repair for zone 5 injuries is suture strength.[2]
- Here, should the distal tendon ends have retracted into the carpal tunnel, the TCL should be released to permit exposure.
- For injuries >7 days old, the surgeon should be prepared to perform nerve grafting for median nerve injuries.
Simple lacerations, lacerations with an isolated tendon injury, and lacerations with associated nerve injuries can be debrided and closed in the emergency room in the setting of a well-vascularized digit. After establishing local or block anesthesia and tourniquet application, thorough debridement and wound cleansing should include exploration of the wound base to exclude the possibility of an open joint and further assess tendons. Follow-up should be established within the week to remove the monofilament suture placed at the time of repair.
Flexor tendon injuries may undergo definitive treatment on the day of injury if they are associated with concomitant major nerve injury or circulatory compromise or per surgeon preference. Repairs for injuries within the synovial sheath should employ a suture method strong enough to allow early digital mobilization while permitting a smooth repair, allowing the tendon to glide through the narrow fibro-osseous tunnel, optimizing early digital mobilization.
The optimal treatment of flexor tendon injuries is primary repair; however, this technique is not always feasible in severe hand trauma. Despite significant improvements in reconstructive techniques, the inconsistencies of primary repair prompt surgeons to consider reconstruction with tendon implants as an alternative method.[11]
Tendon Grafting is used to repair segmental tendon loss or muscular contracture.
- Indications for tendon grafting include failure of flexor tendon repair, injuries resulting in segmental tendon loss, delay in repair that obviates primary repair, severe crush injuries with segmental tendon loss, lacerations that have been neglected for more than 3-6 weeks, patients in whom the surgeon believes delayed grafting is the better treatment alternative, suspicion of wound infection, a closed rupture in zone 1 to zone 3, or for delayed presentation of FDP avulsion injuries associated with significant tendon retraction.
- Single-stage repairs require adequate tendon sheath and pulleys, soft tissue coverage, and supple joints.
- The injured tendons are excised and replaced with a suitable tendon graft secured to the base of the distal phalanx at FDP insertion and joined to a proximal motor in the palm or distal forearm.
- Two-stage repair is used when tendon sheath is scarred or unusable, in cases of pulley incompetence, joint contracture, inadequate passive range of digital motion, or following crush injuries with extensive soft tissue damage and underlying fractures; the native tendon is excised during the 1st stage, while the graft is sutured and subsequent tension is adjusted during the 2nd stage.[11]
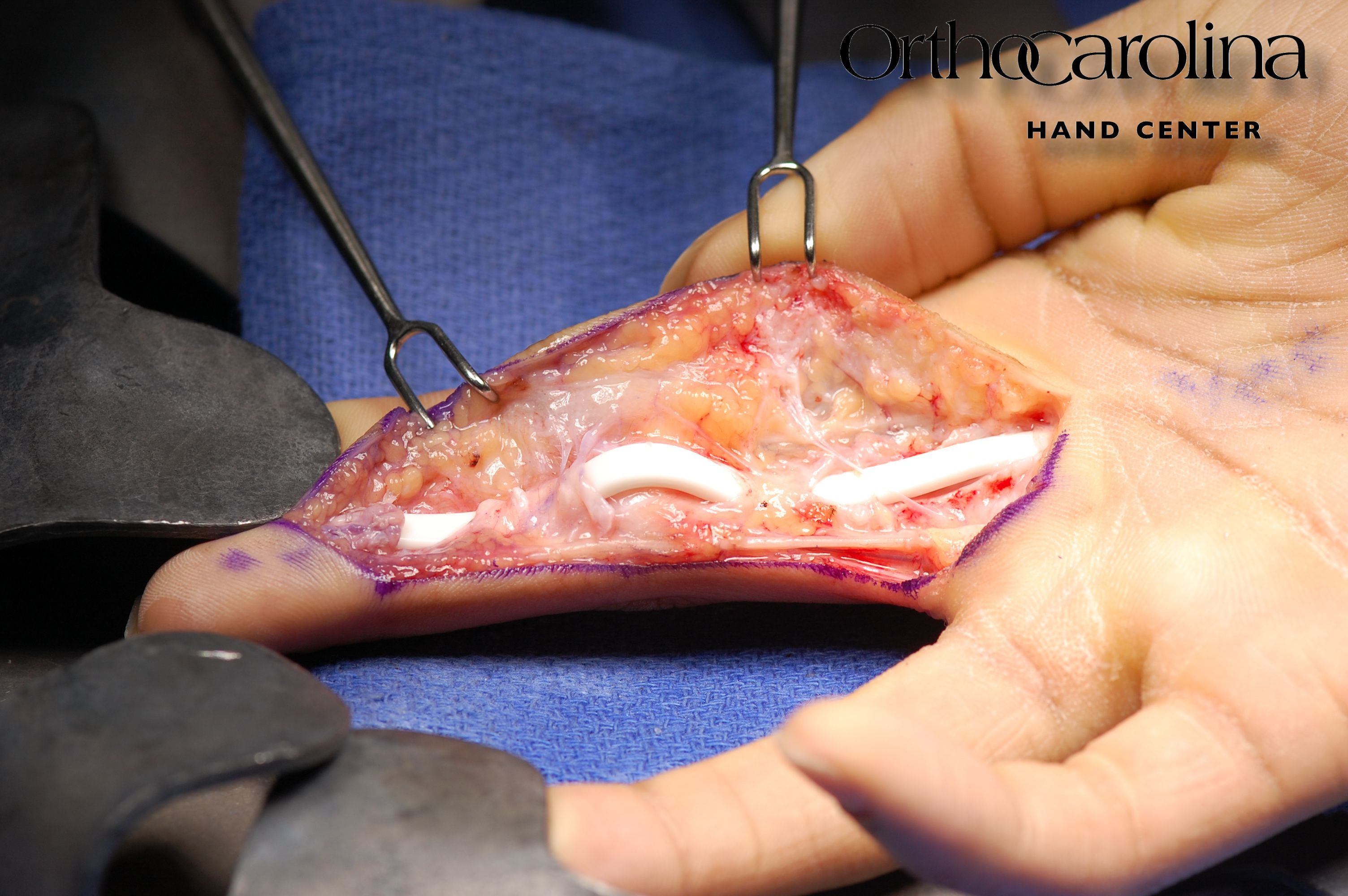
- The first procedure consists of thorough digital exploration, reconstruction of associated injuries, and placement of a passive silicone tendon implant that allows for correction of joint contracture, reconstruction of pulleys, and formation of a pseudosheath.[11][12] The index operation is subsequently followed by therapy to regain and maintain PROM for 6 to 12 weeks. The second stage proceeds thereafter, with the placement of an extrinsic-free donor tendon graft that is fixed to the distal end of the previously implanted rod and pulled proximally through pseudosheath; the implant is then removed, and the tendon graft is sutured to the proximal flexor stump with corrective tensioning. This salvage/reference option is termed the Hunter technique [Figures 1, 2, 3].
- Potential sources for donor graft include palmaris longus, plantaris, extensor digiti minimi, extensor indicis proprius, or toe tendons.[11]
- Intrasynovial tendon grafts may afford distinct advantages over extrasynovial tendons. Their association with less tenocyte death and fewer peri-tendinous adhesions has been well documented. However, since Leversedge et al. first reported outcomes of their 8-case flexor tendon injury pilot study that suggested intrasynovial tendon grafting offers an improved alternative for grafting to digital synovial spaces, there has not been considerable evidence to substantiate these basic biological principles.[13]
Tendon Transfer has limited indications for flexor tendon repair; however, it can be considered when proximal musculature is deemed unusable because of denervation, direct injury, or contraction.
Operative Principles:
Before proceeding with surgery, the nature and number of expected procedures and the extent of postoperative rehabilitation should be outlined to the patient's level of understanding. Patient selection and education are essential for the success of flexor tendon reconstruction. As it has been previously proven that most patients will underestimate the impact of the reconstruction process, the patient must be willing and able to comply and demonstrate adherence to their aftercare program and therapy protocol(s).
Younger patients typically have better outcomes than the elderly; however, technical difficulties and compliance with rehabilitation may compromise this statistic in very young patients. Crush injuries, fractures, joint disruption, nerve and artery damage, associated skin loss, and infections preclude a poorer prognosis after tendon reconstruction—tendons injured outside of the digital flexor sheath yield greater results than those injured within zone 2. The patient's innate healing response to injury ultimately influences the end result.
For simplicity in operative visualization, profundus tendons are generally flat and multistranded, while superficialis tendons, FPL, and index profundus are oval. Profundus tendons should be repaired first, followed by FPL, and finally, superficialis.
Flexor tendon repairs should be performed under loupe magnification in the operating room while maintaining the viability of skin flaps, permitting wide exposure, and prohibiting the formation of scar contractures, with minimal traumatic handling of the tendon surfaces to limit subsequent adhesion formation. It is important to recognize the location of the skin laceration may be different than the site of the tendon injury based on the extension/flexion position of the digit at the time of injury. The initial strength of repair is proportional to the size and number of suture strands crossing the repair site.
The Pulvertaft weave technique interloops the proximal and distal tendon ends and is suitable for tendon grafts or transfers. The added bulk provided by weaving prohibits using this technique outside zones 3/4. As the strongest method, it is capable of withstanding immediate active motion.
Every effort should be employed to preserve or reconstruct at least A2 and A4 pulleys. An incompetent pulley system leads to volar translation or "bowstringing." [12][1] Pulley reconstruction should ensure the sufficient length and tension to hold tendons near the bone but not restrict tendon excursion while restoring the position of flexor tendons in the tendon sheath. Several authors recommend preserving or reconstructing at least three pulleys, for the system is important in bowstringing prevention, improving effective excursion, and decreasing the degree of flexion contracture. In support of the aforementioned, Wehbe et al. previously identified a clear association between the number of intact pulleys and final flexion contractures.[11] Although, this operative principle has recently been called into question with studies declaring it more essential to achieve quality tendon repair and, if needed, permit some degree of pulley release.
Optimized outcomes were reported amongst slightly tensioned multistrand repairs that underwent judicious venting of pulleys which then proceeded to early active motion - all widely accepted principles. In addition, tailoring the repair according to intraoperative active movement examinations in a wide-awake local anesthesia no tourniquet (WALANT) surgical setting is recommended for improved results.[14] The flexor tendon should be approximated utilizing 3-0 or 4-0 core suture via locking 4- to 6-strand repair technique with 0.7-1.0 cm purchase, creating slight bulk (20-30% tendon size) over the repair site. This constructs a slightly tensioned flexor tendon repair that encourages early active rehabilitation and has largely replaced the previous 2-strand or tension-free repairs with weak core sutures.[14][1]
Conversely, increasing the number of core sutures to achieve greater strength inevitably adds more volume to the tendon, resulting in a bulky repair that further leads to increased resistance to gliding, thus must be balanced with the surgeon's ability to suture the tendon atraumatically between bulk and repaired tendon gliding.[15] The addition of a running Prolene epitendinous 5-0 or 6-0 circumferential suture adds upwards of 50% to the total strength of the repair, irrespective of operative technique.[1] For improved dexterity, one slip of the FDS should be repaired. Before skin closure, tendon gliding through A2 and A4 pulleys should be assessed via passive flexion. Minimization of skin incisions assists with decreasing finger edema and potential adhesion formation. In animal models, bipolar coagulators and CO2 lasers were shown to be associated with significantly increased adhesion formation resulting from thermal damage when compared with sharp scalpel dissection alone.[14]
A Journal of Clinical Orthopedics and Trauma recent study revealed 4-stranded cruciate technique had greater functional outcomes and decreased risk of complications compared to modified Kessler repair. The 4-strand cruciate repair demonstrated an excellent (defined as a tip-to-palm distance of less than 1 cm and total active motion of more than 200 degrees) result in 66.6% of patients, while modified Kessler had excellent results in 45.8%.[16]
WALANT surgical technique for flexor tendon repair is recommended to permit necessary adjustments of tendon repairs. There are numerous advantages to employing the WALANT technique: reduced costs, no tourniquet, no sedation nor need for an anesthesiologist, intraoperative patient education, and a direct view of repair.[2] The advent of WALANT has proved enormously advantageous in managing patients with flexor tendon injuries, as it permits dynamic movement during surgery, allowing visualization and understanding of correctly repaired tendon(s) before exiting the operating room.[2] The patient is asked to actively flex and extend their finger to observe free tendon gliding and visualize the presence of gapping. If appreciable gapping, the repair can be strengthened with additional core suture, while constricting pulleys blocking smooth gliding can be judiciously vented.[14]
Differential Diagnosis
Flexor tendon injuries frequently complicate lacerations to the palmar surface of the digit and hand and can be subcategorized as partial lacerations, complete lacerations, and tendon avulsion injuries.
Pertinent Studies and Ongoing Trials
Although the two-strand suture method still employs widespread acceptance, newer multi-strand techniques are increasingly used because they are more robust and have increased resistance to repair site gapping. More modern core tendon suture placement methods have shown greater initial repair site tensile strength while improving strength through six weeks postoperatively.
Vitamin C is an antioxidant previously examined in flexor tendon repair. Tissue damage and hemorrhage can disturb redox regulation, favoring a fibrotic response at the tendon repair site.[17] Hung et al. used a chicken model to examine the effects of local vitamin C following flexor tendon injury and repair, with resultant improved gliding resistance, reduced fibrotic size, and fewer adhesions six weeks following repair, compared to normal saline controls.[17] Other authors have reported oral ibuprofen, 5-fluorouracil, local vitamin E analogs, and hyaluronic acid therapy limit adhesion formation in animal models.[18][19][20]
Recent research has described the use of ibuprofen at anti-inflammatory doses (2400 mg/day) to decrease peritendinous adhesions following zone 2 flexor tendon repairs, with increased range of motion when compared to control groups, and demonstrated no complications.[21]
Literature has additionally demonstrated that methylene blue (MB) decreases levels of inflammatory cytokines and harbors anti-inflammatory and antioxidant properties while reducing the harmful effects of nitric oxide. This finding precludes the understanding that MB will accelerate the tendon healing process while reducing postoperative adhesions. Histopathological and biomechanical data of such studies have revealed fewer adhesions, with more comfortable movement, introducing a novel, cost-effective local therapy with important advantages.[3]
Although well-known throughout various surgical procedures as a hemostatic agent while promoting tissue bonding, fibrin glue-augmented tendinous repairs have been reported throughout animal model studies to reveal an improved range of motion in the early postoperative phase.
Individual flexor tendons have a proximal region (i.e., proximal aspect of the palm, wrist, and forearm) that is extrasynovial and a distal region (i.e., the distal aspect of palm and finger) that is intrasynovial. Uninjured intrasynovial tendons are avascular and contain high levels of proteoglycans while expressing inflammatory factors, complement proteins, and glycolytic enzymes. In contrast, extrasynovial tendons are well vascularized, contain low levels of proteoglycans, and are enriched in inflammatory inhibitors and oxidative phosphorylation enzymes. Thus, the response to injury and repair are distinctly different between the two tendonous regions. Extrasynovial tendons display a robust and rapid neovascularization response, increasing the expression of complement proteins while exhibiting an acute shift in metabolism to glycolysis. As biomolecular modulation and tissue engineering for tendon repair are highlights of ongoing research, future treatment strategies may opt to promote features of extrasynovial healing, focusing on enhanced vascularization and modulation of the complement system and/or glucose metabolism.[6]
Treatment Planning
The optimal flexor tendon repair timing depends on the findings of a thorough history and physical exam. Preoperative planning should account for the possible need for microsurgical nerve and arterial repair. Only in the setting of compromised digital artery perfusion is an emergent repair of the lacerated tendon(s) indicated. If the mechanism suggests arterial injury or digital perfusion is altered, urgent exploration and tendon repair with concomitant microvascular digital artery and nerve repair is warranted.
Primary repair done within the first few days following injury, on a non-emergent basis, allows for adequate patient preparation, education on postoperative therapy regimens, postoperative protocols, and optimal operative conditions. In addition, the wound is easier to manage, and the tendon ends are fresh for repair.
When the interval between injury and diagnosis is unknown, the patient provides an unreliable history, or otherwise, a delayed presentation, preoperative consideration should be given to the potential indication for tendon reconstruction and repair. More complicated cases may warrant primary tendon graft or tendon spacer, with secondary reconstruction.
Although repair of both tendons is preferable for optimal gliding and strength, in cases of severely injures, unclean/jagged tendon ends, or evidence of insufficient tendon volume for repair, repair of both tendons may be unfeasible; rather, FDS tendon excision and isolated FDP repair may be the best alternative. Simpler fingers subsequent to isolated FDP repair in a severely traumatized digit may result in decreased adhesion formation.
Staging
In addition to understanding and confidently identifying the five flexor zones and further sub-categorizing zone 1 into the Leddy classification system, it is essential to be knowledgeable of the Boyes preoperative classification, denoting preoperative conditions of the tendon under concern.
Grade 1 - good: minimal scarring with mobile joints and no trophic changes
- At this stage, tendon reconstruction is considered, if indicated, as the soft tissues should be healed, mobile, stable, free of joint contracture, and demonstrate full passive motion.
Grade 2 - cicatrix: heavy skin scarring secondary to injury or prior surgery; deep scarring because of failed primary repair or infection
Grade 3 - joint damage: injury to joint with restricted range of motion
Grade 4 - nerve damage: injury to digital nerves resulting in trophic changes in finger
Grade 5 - multiple sites of damage: involvement of multiple fingers with a combination of the above problems[12]
If the indications for a single-stage repair (Boyes grade 1) are not satisfactorily appreciated (Boyes grade 2 to 5), patients are generally considered candidates for two-stage reconstruction.[12]
Prognosis
Outcomes after flexor tendon repair are variable and dependent upon the nature of the disease, the patient’s individual biological response to injury, timing, and method of repair, and patient compliance with the postoperative therapy regimen. Good functional outcomes result from satisfactory tendon repair with full participation and compliance in tendon repair aftercare programs. Early initiation of postoperative mobilization protocols promotes intrinsic tendon healing, increases tensile strength, decreases adhesion formation and edema, and improves tendon gliding, thus optimizing flexor tendon repair prognosis. The most common complication is digital stiffness. Repair site ruptures are, fortunately, uncommon; however, they generally indicate non-compliance with suggested therapy protocols.
Age, language barriers, smoking, mechanism and extent of injury, additional associated injuries, zone of injury, the time elapsed from insult to surgery, surgical technique, postoperative rehabilitation protocol, and adherence to therapy are factors implicated in the outcome of flexor tendon repair.[10] Outcomes may differ between individuals, in part, due to a lack of resources, higher postoperative infection rates, and lower levels of education. Postoperative functional outcomes may be further influenced by nosocomial infections, which contribute to the disproportionately high burden of infection in clinical facilities with limited resources.[10]
Additionally, in high-volume, specialized hand centers, patients are likely to undergo surgery sooner after the injury than in lower-volume facilities; therefore, a difference in postoperative functional outcomes between patients treated in either type of facility may exist.[10] Language barriers may limit communication of postoperative instructions and the importance of rehabilitation, causing patients to be unintentionally non-compliant, thus negatively impacting their outcome after flexor tendon repair.[10]
Zone 2 injury is a well-documented risk factor for poorer outcomes, likely secondary to the challenging anatomy containing both FDS and FDP within a narrow fibro-osseous sheath.[4]
Complications
Despite continual improvement in surgical care and rehabilitation of flexor tendon injuries, complications still occur; their effects on hand function can be devastating and long-lasting.
- Ruptures are slightly more common in flexor pollicis longus than other tendons, occurring in approximately 5% of all total repairs. Rupture warrants immediate exploration and re-repair before scarring and retraction prevent successful repeat repair.[1] Recurrent rupture is optimally treated via secondary tendon reconstruction, tendon transfer, or arthrodesis.
- The greatest protection against repair site rupture is a well-performed multistrand core suture, with a concomitant running circumferential repair and early initiation of high-quality hand therapy.
- Reports have demonstrated that 2-stranded methods are not strong enough for controlled active motion or early postoperative use of the hand, with a rupture rate of 11.7%.[15]
- By allowing surgeons to identify and repair tendon gaps prior to skin closure, the WALANT approach to flexor tendon repair has decreased the rupture rate by 7%. Eliminating the gap with full fist flexion and extension testing intraoperatively gives the team confidence to hold to true active movement-based therapy protocols post-operatively.[22]
- Adhesions result from a limited range of motion subsequent to postoperative and postinjury scarring, with an increased likelihood of adhesion formation following periods of prolonged immobilization or after severe injuries. It is here where the tendinous extrinsic healing component acts as the culprit of adhesion formation between the tendon and its surrounding fibro-osseous sheath. Adhesions with resultant digital stiffness remain one of the most common complications after flexor tendon repair.
- Adhesion formation with subsequent restriction of tendon excursion prompting the need for tenolysis has been reported in rates varying from 12-47%.[11]
- Tenolysis can be considered if 3-6 months have elapsed since still-intact tendon repair; however, the active range of motion remains significantly less than the passive range of motion, or there has been no appreciable improvement in the range of motion after aggressive hand therapy.
- 17% of tendon repairs progress to develop contractures; their prevention is primarily via splinting, with operative treatment proceeding to either open or closed capsulotomy for recalcitrant cases.
- Only after the near complete restoration of PROM should patients be considered for tenolysis to secondarily improve AROM.[23]
- Infection, skin flap necrosis, mechanical failure of an implant (if used), pulley disruption, swan neck deformity, infection, and synovitis are also possible complications following operative therapy for flexor tendon injuries.
- Disruption of the distal implant juncture after stage one, rupture of the graft, a graft that is too loose or too tight, development of an intrinsic plus phenomenon, reflex dystrophy, nail deformity, scar sensitivity, triggering, and flexion deformities are complications considered in the case of staged tendon reconstruction[11]
Postoperative and Rehabilitation Care
Extension block-splints should position the wrist in 30 degrees of flexion to take tension off flexor tendon repairs and minimize the risk of postoperative tendon rupture, with metacarpophalangeal joints in 45-70 degrees of flexion, maintaining interphalangeal joints in near full-extension or slight flexion (15 degrees). Sutures are removed after two weeks.
Through advancements in biomechanical and clinical research, there is a general understanding that early therapy-guided tendon excursion is more beneficial than strict immobilization in efforts to achieve maximal functional recovery. Mobilization promotes intrinsic tendon healing, increases tensile strength, and decreases adhesion formation while improving tendon gliding - all benefits which translate into optimized joint motion, fewer flexion contractures, and overall, enhanced functional outcomes. Tendon repair rehabilitation programs are ideally constructed to improve the function of the entire hand while facilitating the differential incorporation of soft tissue injuries. Although each patient’s situation is generally similar, the therapy program must be individualized. Thus, there is no alternative to a knowledgeable, experienced, energetic, meticulous hand therapist. Early controlled mobilization protocols are now the standard of care; passive rehabilitation protocols have been largely abandoned.[14] Various recommendations include early, controlled passive range of motion with a goal of at least 2 to 4 mm of differential gliding between FDS and FDP and/or elastic band traction for active extension and passive flexion, with multiple variations and modifications of these protocols in place.
Once such, the Saint John Protocol, describes a regimen of up to one-half fist of protected true active finger flexion initiated 3 to 5 days following flexor tendon repair. Waiting 3 to 5 days before movement allows the swelling, work of flexion, and friction to decrease, thus minimizing the risk of rupture.[22] The protocol then proceeds through “warm up” passive flexion of all digits before advancing to active flexion. Active IP joint extension while in MP flexion block prevents IP joint flexion contracture. True active flexion up to one-third to one-half a fist is established throughout day 4 to week 2. From 2 to 4 weeks, patients are engaged in an active synergistic exercise program, working towards half to full active fist position with 45 degrees of wrist extension while continuing IP joint extension. Ideally, it aims to achieve a full fist position in 6 weeks. Patients are generally cleared to begin light activity at six weeks.[22]
Support of early therapy was additionally favored via a study by Johnson et al. in which 56% of their cohort started therapy within one week of tendon repair. Given the known clinical benefits of early hand therapy, with no difference in complication rate, tendon rupture, or secondary surgeries based on the timing of hand therapy initiation, their study supports the initiation of hand therapy in the early-to-mid part of postoperative week 1, specifically, for zone 2 injuries.[5]
If immobilized, repair strength is 50% less than the original repair following the first postoperative week. After three weeks of continued immobilization, the strength decreases by 30%. On the other hand, following a synergistic wrist protocol with mobilization, the repair site strength increases by a factor of 2 or more between 4 to 6 weeks postoperatively. After 3 to 4 months, patients have recovered approximately 90% of their ultimate range of motion.
As soon as possible, patients begin a graded rehabilitation protocol under the supervision of a qualified therapist while using a molded, protective aftercare splint and synergistic wrist motion to increase repair site excursion. The therapist will frequently monitor compliance by having the patient attend therapy at least twice weekly for the first 6 to 8 weeks. Progression through the postoperative therapeutic regimen is based on the injury and the patient’s physiologic response. Anticipate the patient returning to full activity 4 to 6 months postoperatively, pending full and motivated compliance to their postoperative regimen.
While the up-to-date techniques in flexor tendon repair have caused an evolution in rehabilitation practice, prompting a transition from passive methods to early, controlled, more active ones, optimal flexor tendon surgery, and therapy results are dependent upon a patient-centered rather than strictly structured protocol.[14]
Consultations
The method of postoperative rehabilitation is significantly influenced by the compliance of the patient, the nature of the wound, and the method/location of repair. Surgeons and hand therapists have to work side-by-side to optimize outcomes following tendon repair and to best facilitate compliance with therapeutic protocols. Clear communication is vital, so much so that often postoperative therapy scheduling is coordinated at the same time as operative boarding to permit a seamless initiation of rehabilitation without unnecessary delay. With the advent of WALANT, intraoperative therapist participation allows patient education to start intraoperatively; the patient will then meet a familiar face in the upcoming therapy sessions, and it further affords the therapist confidence in the repair to move the finger postoperatively. Before beginning therapy, it is essential that therapists receive information from the operative surgeon regarding the type of repair and whether other structures were found to be injured. At some institutions, hand therapists are involved pre- and even intra-operatively, thus permitting the patient to interact with the entire team and allowing them to meet a familiar face in their postoperative sessions. A total active movement examination, performed intraoperatively before skin closure, assists the therapist in gaining confidence to move the repaired finger early.[14]
Individualized therapy regimens typically begin 1 to 5 days following surgical repair. Patient compliance, edema, suture size and configuration, wound complications, dressings, systemic conditions, and concomitant injuries are influential factors in the makings of aftercare protocols. Therapists are encouraged to optimize their postoperative programs by controlling the force applied to the repair site while promoting tendon excursion. It is believed that improvements in range of motion and overall patient outcomes are secondary to optimal tendon excursion.
Deterrence and Patient Education
Postoperative rehabilitation is largely influenced by patient compliance. Although general guidelines are implemented for various therapeutic interventions, regimens are accelerated and decelerated based on individualized adherence and subsequent response to therapy. Return to work can take several months. Approximately 10% of patients may require secondary surgeries for complications. Thus, adherence to postoperative therapy must be stressed to optimize functional outcomes.[14]
Pearls and Other Issues
A smooth tendon suture is important for restoring a low-friction gliding surface and facilitating tendon rehabilitation. Mastering a method that allows for atraumatic suture placement with stable, accurate coaptation of the tendon ends that is strong enough to allow early digital mobilization while preventing gapping is a focus for improving the strength and efficacy of flexor tendon repairs while optimizing patient outcomes.
Limited skin incisions, gentle handling of the tendons, and sharp dissections are important surgical tips to minimize postoperative adhesion formation, in addition to lessening the use of cautery around tendons while permitting minor bleeding to coagulate naturally.[14] There are well-documented benefits achieved from intraoperative active movement that permits tailoring of the repair to establish free tendon gliding. Therapist-supervised early active rehabilitation and close interdisciplinary communication are the mainstays of the postoperative period.[14]
Enhancing Healthcare Team Outcomes
Restoration of satisfactory digital function after an unrepaired flexor tendon laceration or failed repair remains one of the most challenging clinical and operative dilemmas in hand surgery. Tendinous injuries may permanently impair hand function, negatively impacting productivity and diminishing quality of life. Thus, maximizing the restoration of hand function is crucial. The best results are associated with early repair. Flexor tendon repair should be performed in an operating room under optical magnification with extensile exposure, thus permitting the injury to be defined in its entirety. Tendon retrieval is done via atraumatic techniques, accurately orienting the tendon while minimizing direct handling and manipulation. The FDP tendon should not be advanced more than 1 cm.
Subsequent sutures should be placed to allow for accurate coaptation of the tendon ends, with chosen suture method delivering a stable, smooth repair that feely glides within the tendon sheath. Completing the repair with a circumferential suture adds strength. Postoperative hematoma formation is prevented by accurate and thorough hemostasis. At the time of repair, ensuring full excursion of the flexor tendon repair is useful in guiding therapy and can be facilitated by performing the tendon repair using local anesthesia in an awake setting. Proper splint placement and postoperative rehabilitation are as crucial as the initial operative technique. The primary objective in treating flexor tendon injuries should be for the patient to return to work and day-to-day functions as early as possible, with minimal loss of function.[3] Goals in flexor tendon repair can be achieved via a combination of surgery and well-led rehabilitation, optimizing outcomes by way of differential tendon gliding and minimization of adhesions while preventing tendon gapping and tendon rupture.[2]
There is no alternative to a dedicated hand therapist in this environment. Clear communication by way of surgeons, nurses, and hand therapists working as an interprofessional team to optimize patient-centered care, and postoperative therapies, increase patient safety, and improve team performance, is of the utmost importance. Thie interprofessional paradigm will result in optimal patient outcomes. [Level 5]
This educational activity reviewed the anatomic relationships of flexor tendons within the hand, described the associated intricacies of hand physiology, explained the key components of a thorough hand examination in diagnosing flexor tendon injuries, highlighted diagnostic modalities and adjuncts, and summarized operative principles correspondent to various zones of flexor tendon injuries while outlining the optimal healthcare team relations and establishing individualized postoperative rehabilitation protocols for enhanced patient outcomes.