Continuing Education Activity
Tibial eminence fractures are very common in the pediatric population. Appropriate diagnosis and treatment are important to avoid the numerous associated complications. This activity reviews the evaluation and management of pediatric tibial eminence fractures and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
- Identify the etiology of pediatric tibial eminence fracture and other associated conditions.
- Outline the appropriate evaluation of pediatric tibial eminence fractures.
- Review the treatment options available for pediatric tibial eminence fractures.
- Describe the interprofessional team strategies for improving care coordination and communication to advance pediatric tibial eminence fractures and improve outcomes.
Introduction
Tibial eminence fractures are not common injuries. Most commonly, these fractures are found in the pediatric population and rarely occur in adults. Pediatric patients are most commonly affected due to the weakness of the subchondral bone, which causes the bone to fail before the ACL.[1] This fracture pattern is considered an anterior cruciate ligament (ACL) equivalent injury in children. In regards to the anatomy, the tibial eminence is non-articular and is located between condylar surfaces of tibial plateaus. The ACL inserts 10 to 14 mm posterior to the anterior border of the tibia and is deeply attached on the subchondral plate.[2] Fracture through the tibial eminence may cause the knee to lose biomechanical function and cause instability as the fracture is an ACL injury equivalent and can have other associated ligament injuries.
Etiology
Historically, tibial eminence fractures most commonly occurred in pediatric patients that fell off of a bike. As athletic participation has become more common, sports-related injuries have become another common cause of injury as the mechanism of injury is similar to that of a mid-substance ACL tear in young adult athletes. Other possible causes include motor vehicle accidents or from low impact injuries where the knee is flexed, and an internal rotation moment occurs through the tibia.[1] In this injury, the bone fails before the ACL, causing a fracture through the cancellous bone below the subchondral plate. Failure of bone prior to ligaments historically was described by Skak et al. in his article regarding distal femoral fractures identifying that the strength of the ligaments increases as more deformation stress is put through them along with a pre-existing compressive force from the mechanism of injury, which in turn takes stress off the side of the ligaments and increases stress through the compressed bone.[3]
Epidemiology
Tibial eminence fractures are very rare injuries affecting 3 in every 100,000 children who sustain injuries to the knee per year.[4] This fracture type most commonly affects patients from the age of 8 to 14 years old. Bone fails before ligament due to incomplete ossification of the tibial eminence. 40% of the time, there are other injuries associated with tibial eminence fractures. These can include meniscal, collateral ligament, capsular, and osteochondral fragment injuries. Proper imaging should be obtained to rule out these injuries as they can affect the treatment approach.[1]
History and Physical
Historically, patients most commonly present for evaluation after a fall off of a bicycle onto the involved knee. Patients will present to their primary care physician, pediatrician, or at the emergency department after having trouble with ambulation secondary to pain and knee effusion. As with any injury or fracture, the skin should first be assessed to ensure there is no evidence of open fractures. If there are associated ligamentous injuries, a knee effusion from a hemarthrosis will not be present as there will be a disruption in the capsule, which allows the effusion to dissipate out of the joint.[1] Patients may have laxity with varus/valgus stress that indicates a disruption in the lateral collateral ligament (LCL) or medial collateral ligament (MCL). Anterior and posterior drawer exams can be performed on the knee to assess the laxity of the ACL and PCL, as well as a Lachman's test to evaluate the ACL. The range of motion should also be assessed and is usually decreased/limited secondary to pain. There may also be a positive McMurray indicating a possible meniscal tear. It is important to examine for injuries to the meniscus as there is a high rate of meniscal entrapment with these types of fractures. According to Kocher et al., entrapment of the anterior horn of the medial or lateral meniscus or the intermeniscal ligament is seen in about 26% of cases of type 2 tibial eminence fractures versus 65% of type 3 tibial eminence fractures. 3.8% of patients present with an associated meniscal tear.[5]
Evaluation
Radiographs of the knee should be obtained to assess the knee for bony injury. Fractures through the tibial eminence should be visible on x-ray. MRI and CT can be obtained for further characterization of the injury.[6] These imaging modalities can be used to assess fracture displacement and comminution. MRI allows detailed evaluation of any soft tissue involvement with the injury (meniscal injury, cartilage, ligaments, etc.) and can also identify any pieces of chondral fracture of the tibial spines that have not yet ossified.[4]. A study by Kocher et al., as well as Mitchell et al., showed that in type II and III fractures, there was a high association of meniscal tears as well as meniscal entrapment. Mitchell et al. also found 7% were found to have associated chondral injuries. Mitchel et al. found type III fractures in 8% had an associated chondral injury, 12% had associated meniscal tears, and 52% had a meniscal entrapment.[7]
Based on imaging review, in 1959 the Meyers and McKeever classification was published:
1. Non-displaced fracture (bony apposition)
2. Partially displaced fracture (posterior hinge)
3. Completely displaced - broken down into (A) not rotated, (B) rotated
4. Comminuted (later added by Zaricznyj in 1977)[2]
Classification of these fractures is important as treatment algorithms are based on the amount of displacement and comminution.
Treatment / Management
Fracture Types
Type 1: Non-operative treatment is in a cylinder cast or knee immobilizer in a position of comfort (either about 20 degrees of flexion or full extension). Consider drainage of hemarthrosis for symptomatic relief. Keep the knee immobilized for 6 to 12 weeks (once radiographic union) and then transition to weight-bearing and range of motion.[2]
Hemarthrosis drainage can also be considered in cases where closed reduction will be performed to assist in reduction.
Type 2 and 3: Treatment is controversial. There is increasing popularity for reduction and internal fixation. Arthroscopic excision of the fracture fragment is also a possible consideration. Consideration for non-operative management can be used for type 2 fractures when a successful closed reduction is performed. If displacement is still present after closed reduction, this can cause issues with obtaining full extension due to impingement in the femoral notch, and operative management should be pursued. In fractures where there is any intra-articular extension, surgical intervention should be considered.[2][1]
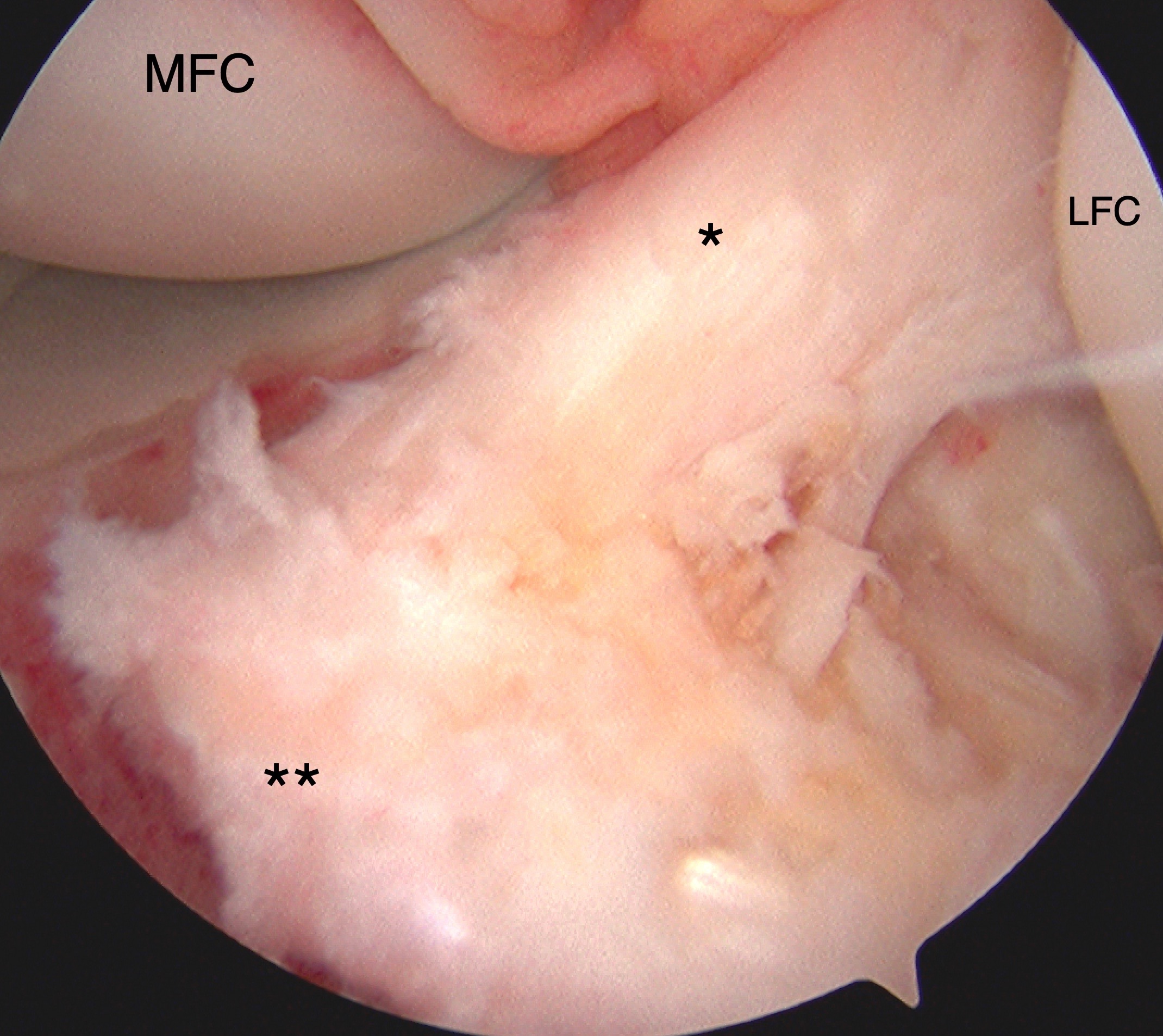
Type 3 and 4: Historically, open reduction and internal fixation of type 3 and 4 fractures were performed through a knee arthrotomy. Due to advances in knee arthroscopy, many recommend arthroscopic reduction and internal fixation of these fracture types. Some combine arthroscopy with arthrotomy to first characterize concomitant intra-articular soft tissue injuries and then perform an arthrotomy to perform internal fixation of the fracture. Performing the entire procedure arthroscopically can be technically challenging, but leads to less soft tissue damage. Arthroscopic fixation is usually by screw or suture after fracture hematoma debridement. Any interposed soft tissue is removed or debrided. Due to the age of the patient population involved, the surgeon must be careful not to disrupt the tibial physis.[1]
Surgical Fixation Techniques
Suture fixation: The benefit of using suture fixation for fracture fixation is there is no need for future hardware removal; however, the technique is technically difficult. First, the tibial tunnel at the ACL footprint is made. Next, the ACL is addressed. There are various ways to perform the technique and a wide variety of devices on the market. Using synthetic absorbable monofilament suture or braided, non-absorbable, monofilament, surgical, single stitch versus a whipstitch is put into the ACL. Absorbable sutures are preferred due to the theoretical tethering of the physis with permanent suture. Metalic sutures can also be used and removed outpatient once there is evidence of radiographic fracture healing in the office. After a stitch is placed through the ACL, the ends of the suture are pulled through the tibial tunnel, and the knee is extended while applying tension to reduce the fragment. The suture is then tied over the bony bridge. Some surgeons use a bone-tendon-bone fixation device to hold temporary fixation to hold reduction prior to tensioning.[8] This is a good technique to consider for comminuted fractures or fractures that are too small for screw fixation as the suture through the ACL can capture these small pieces. If the fragment is big enough, the suture can be passed through the fragment. This technique avoids placing hardware across the physis.[1][9]
Screw Fixation: There are two options with screw fixation: it can be placed either anterograde or retrograde. Cannulated screws are more popular for fixation due to the ease of correct placement. There has been a trend toward suture fixation due to the risk of hardware irritation and the possible need for repeat surgery for screw removal. If screws are not placed deep enough, they can cause issues with impingement or damage the articular cartilage. With screw fixation, there is also a concern for growth disturbance when crossing the tibial physis. The size of the fractured piece also limits screw fixation.
-Anterograde fixation: First, reduce the fracture. Next, flex the knee to 90 degrees, and, using the anteromedial portal, insert the guidewire superoanterior to inferoposterior. Last, place a cannulated screw over the guidewire to fixate the fracture.
-Retrograde fixation: Considered to be less invasive. The fragment must be greater than 15 mm in size to obtain a good purchase. The guidewire should be inserted through the anterior tibial cortex and directed toward tibial eminence. The cannulated screw should be placed over the guidewire, and the fracture fixated.
Comparing the two techniques for fixation, screws provide a more rigid fixation; however, using 3 No.2 multi-strand, long-chain ultra-high molecular weight polyethylene sutures has a higher load to failure than cannulated screw fixation. Studies looking at cyclic loading of constructs comparing screw fixation versus suture fixation have shown that suture fixation has greater strength.[1]
Differential Diagnosis
ACL tear, meniscal tear, LCL or MCL sprain, patella fracture, osteochondral fragment, femoral condyle fracture, tibial plateau fracture.
Differential diagnosis can be ruled in or out by obtaining radiographs of the knee and using further diagnostic imaging such as CT or MRI to assist in the diagnosis.
Staging
1959 the Meyers and McKeever Classification was published:
1. Non-displaced fracture (bony apposition)
2. Partially displaced fracture (posterior hinge)
3. Completely displaced - broken down into (A) not rotated, (B) rotated
4. Comminuted (later added by Zaricznyj in 1977)[2]
Prognosis
In displaced fractures, without surgical intervention, there is a high incidence of knee instability.[10] In a study by Pailhe et al., there were better functional outcomes in patients treated surgically. Patients who undergo surgical reduction and internal fixation generally have good results with an average Lysholm score of 84.6. 81% of patients had satisfactory to very satisfied results when asked. Return to sporting activities was 20 weeks in this study.[11] In regards to patients treated with arthroscopic reduction internal fixation versus open reduction internal fixation, a study performed by Pailhe et al. showed no difference in patient outcomes. They also found no difference in patients treated with screw fixation versus suture fixation.[11]
Complications
Complications that can be encountered with this type of fracture can include loss of motion, malunion, disuse quadriceps atrophy, nonunion, physeal disruption/growth disturbance (recurvatum deformity, distal femoral valgus deformity, limb length discrepancy), laxity, hardware irritation/impingement (most common with metal suture and screw fixation), mechanical impingement, arthrofibrosis, chondral injury.[1]
Another complication that can occur is interposed soft tissue within the fracture site. This can impede fracture reduction and prevent fracture healing or lead to malunion and subsequent impingement of the malreduced fracture. Soft tissue that can become interposed includes the transverse intermeniscal ligament and the anterior horn of the medial or lateral meniscus.
In regards to arthrofibrosis after surgical management, Watts et al. found there was no difference in the incidence based on the surgical approach independently; however, they found in their study that patients that underwent arthroscopic fixation had more risk factors for arthrofibrosis (time to referral to a pediatric orthopedic surgeon who performs the technique, length of surgery). Watts et al. advocated that time to surgery greater than 7 days from injury and that prolonged operative time greater than 120 minutes put patients at an increased risk for arthrofibrosis.[12]
Postoperative and Rehabilitation Care
Each surgeon has a different postoperative protocol. For non-displaced fractures, immobilization should be for 6 weeks or until evidence of radiographic fracture union for type 1 tibial eminence fractures. Isometric closed chain hamstring and quadricep exercises should be introduced early in rehab to prevent atrophy. Fractures treated surgically are at increased risk for stiffness, so early range of motion is important. Early range of motion is determined on a patient to patient basis.[1] For postoperative rehabilitation, the knee should be immobilized in extension for 2 weeks, with a gradual range of motion being initiated at this time. Partial weight-bearing is allowed at two weeks with crutches. Quadriceps exercises should be initiated at all time points after surgery to avoid atrophy postoperatively.[8]
Deterrence and Patient Education
It is essential to educate the patient and family on the possibility of growth disturbance with fixation of these fractures. Patients and families should be educated on the complications of surgery, including possible secondary surgery for hardware irritation, surgeries related to growth disturbances, the possibility of leg length inequality, risk of infection, risk of damage to surrounding structures, and possible non-union. The importance of postoperative rehabilitation should be emphasized to avoid complications from delayed motion due to patient pain tolerance. Patients should be educated about the risk of arthrofibrosis and quadriceps atrophy and the importance of working hard with physical therapy to get motion and strength back. It is also important to educate the patient and family that there may still be knee instability after treatment as the injury itself can stretch the fibers of the ACL and cause elongation of the fibers.[4]
Enhancing Healthcare Team Outcomes
Appropriate diagnosis and evaluation of patients with tibial eminence fractures are important to provide the best care for patients. Delay in treatment can lead to further injury to other structures within the knee. Primary care, pediatric, and emergency department physicians need to recognize this injury and to refer the patient appropriately for further treatment. Associated injuries should be recognized early to allow earlier evaluation to optimize treatment. For non-operative treatment, communicating appropriate cast care to caregivers and nursing is important to avoid any skin related complications from casting. Proper directions regarding weight-bearing status are important regarding any physical or occupational therapy the patient receives during their fracture rehabilitation. Communicating with the patient and the interprofessional team's expectations of treatment is important to optimize treatment and to address all concerns that may arise for the patient.