[1]
Gale R, Seidman DS, Stevenson DK. Hyperbilirubinemia and early discharge. Journal of perinatology : official journal of the California Perinatal Association. 2001 Jan-Feb:21(1):40-3
[PubMed PMID: 11268867]
[2]
Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. British journal of hospital medicine (London, England : 2005). 2017 Dec 2:78(12):699-704. doi: 10.12968/hmed.2017.78.12.699. Epub
[PubMed PMID: 29240507]
[3]
Kaplan M, Renbaum P, Levy-Lahad E, Hammerman C, Lahad A, Beutler E. Gilbert syndrome and glucose-6-phosphate dehydrogenase deficiency: a dose-dependent genetic interaction crucial to neonatal hyperbilirubinemia. Proceedings of the National Academy of Sciences of the United States of America. 1997 Oct 28:94(22):12128-32
[PubMed PMID: 9342374]
[4]
Moncrieff MW, Dunn J. Phototherapy for hyperbilirubinaemia in very low birthweight infants. Archives of disease in childhood. 1976 Feb:51(2):124-6
[PubMed PMID: 944021]
[5]
Bhutani VK, Wong R. Bilirubin-induced neurologic dysfunction (BIND). Seminars in fetal & neonatal medicine. 2015 Feb:20(1):1. doi: 10.1016/j.siny.2014.12.010. Epub 2015 Jan 7
[PubMed PMID: 25577656]
[6]
Ip S, Chung M, Kulig J, O'Brien R, Sege R, Glicken S, Maisels MJ, Lau J, American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004 Jul:114(1):e130-53
[PubMed PMID: 15231986]
[7]
Leung AK, Sauve RS. Breastfeeding and breast milk jaundice. Journal of the Royal Society of Health. 1989 Dec:109(6):213-7
[PubMed PMID: 2513410]
[8]
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004 Jul:114(1):297-316
[PubMed PMID: 15231951]
[9]
Shahid R, Graba S. Outcome and cost analysis of implementing selective Coombs testing in the newborn nursery. Journal of perinatology : official journal of the California Perinatal Association. 2012 Dec:32(12):966-9. doi: 10.1038/jp.2012.26. Epub 2012 Mar 22
[PubMed PMID: 22441112]
[10]
Desjardins L, Blajchman MA, Chintu C, Gent M, Zipursky A. The spectrum of ABO hemolytic disease of the newborn infant. The Journal of pediatrics. 1979 Sep:95(3):447-9
[PubMed PMID: 469673]
[11]
. ACOG practice bulletin. Prevention of Rh D alloimmunization. Number 4, May 1999 (replaces educational bulletin Number 147, October 1990). Clinical management guidelines for obstetrician-gynecologists. American College of Obstetrics and Gynecology. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 1999 Jul:66(1):63-70
[PubMed PMID: 10458556]
[12]
Gómez-Manzo S, Marcial-Quino J, Vanoye-Carlo A, Serrano-Posada H, Ortega-Cuellar D, González-Valdez A, Castillo-Rodríguez RA, Hernández-Ochoa B, Sierra-Palacios E, Rodríguez-Bustamante E, Arreguin-Espinosa R. Glucose-6-Phosphate Dehydrogenase: Update and Analysis of New Mutations around the World. International journal of molecular sciences. 2016 Dec 9:17(12):
[PubMed PMID: 27941691]
[13]
Grace RF, Zanella A, Neufeld EJ, Morton DH, Eber S, Yaish H, Glader B. Erythrocyte pyruvate kinase deficiency: 2015 status report. American journal of hematology. 2015 Sep:90(9):825-30. doi: 10.1002/ajh.24088. Epub 2015 Aug 14
[PubMed PMID: 26087744]
[14]
Da Costa L, Galimand J, Fenneteau O, Mohandas N. Hereditary spherocytosis, elliptocytosis, and other red cell membrane disorders. Blood reviews. 2013 Jul:27(4):167-78. doi: 10.1016/j.blre.2013.04.003. Epub 2013 May 9
[PubMed PMID: 23664421]
[15]
Perrotta S, Gallagher PG, Mohandas N. Hereditary spherocytosis. Lancet (London, England). 2008 Oct 18:372(9647):1411-26. doi: 10.1016/S0140-6736(08)61588-3. Epub
[PubMed PMID: 18940465]
[16]
Gallagher PG, Weed SA, Tse WT, Benoit L, Morrow JS, Marchesi SL, Mohandas N, Forget BG. Recurrent fatal hydrops fetalis associated with a nucleotide substitution in the erythrocyte beta-spectrin gene. The Journal of clinical investigation. 1995 Mar:95(3):1174-82
[PubMed PMID: 7883966]
[17]
McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. The Cochrane database of systematic reviews. 2013 Jul 11:2013(7):CD004074. doi: 10.1002/14651858.CD004074.pub3. Epub 2013 Jul 11
[PubMed PMID: 23843134]
Level 1 (high-level) evidence
[18]
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, Simes J, Tarnow-Mordi W. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. American journal of obstetrics and gynecology. 2018 Jan:218(1):1-18. doi: 10.1016/j.ajog.2017.10.231. Epub 2017 Oct 30
[PubMed PMID: 29097178]
Level 1 (high-level) evidence
[19]
Fenton C, McNinch NL, Bieda A, Dowling D, Damato E. Clinical Outcomes in Preterm Infants Following Institution of a Delayed Umbilical Cord Clamping Practice Change. Advances in neonatal care : official journal of the National Association of Neonatal Nurses. 2018 Jun:18(3):223-231. doi: 10.1097/ANC.0000000000000492. Epub
[PubMed PMID: 29794839]
Level 2 (mid-level) evidence
[20]
Nakagawa M, Ishida Y, Nagaoki Y, Ohta H, Shimabukuro R, Hirata M, Yamanaka M, Kusakawa I. Correlation between umbilical cord hemoglobin and rate of jaundice requiring phototherapy in healthy newborns. Pediatrics international : official journal of the Japan Pediatric Society. 2015 Aug:57(4):626-8. doi: 10.1111/ped.12583. Epub 2015 Mar 25
[PubMed PMID: 25533043]
[21]
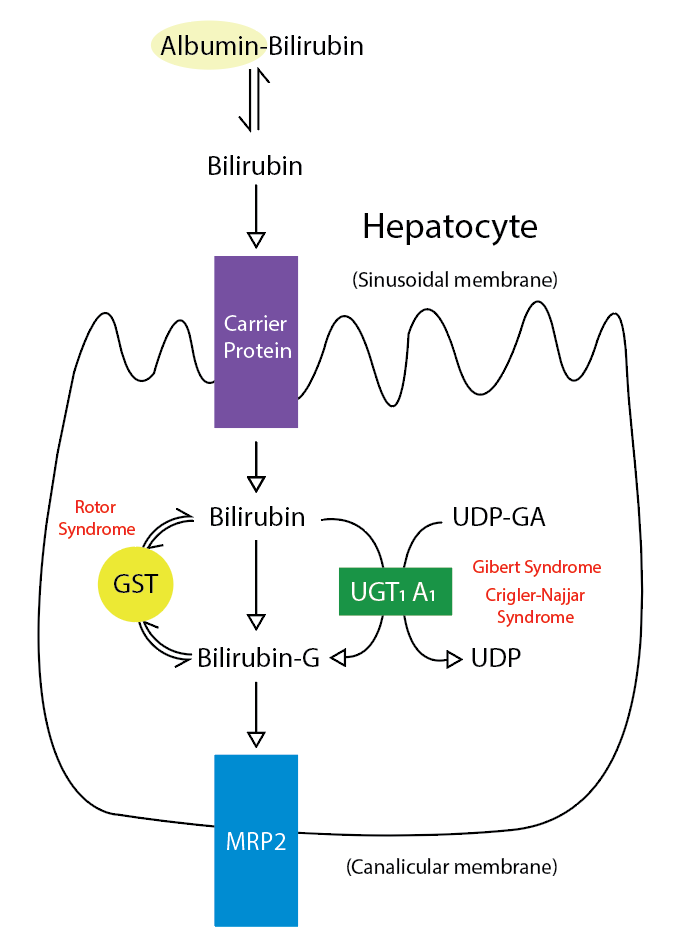
Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, Lindhout D, Tytgat GN, Jansen PL, Oude Elferink RP. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert's syndrome. The New England journal of medicine. 1995 Nov 2:333(18):1171-5
[PubMed PMID: 7565971]
[22]
Anderson NB, Calkins KL. Neonatal Indirect Hyperbilirubinemia. NeoReviews. 2020 Nov:21(11):e749-e760. doi: 10.1542/neo.21-11-e749. Epub
[PubMed PMID: 33139512]
[23]
Maruo Y, Nakahara S, Yanagi T, Nomura A, Mimura Y, Matsui K, Sato H, Takeuchi Y. Genotype of UGT1A1 and phenotype correlation between Crigler-Najjar syndrome type II and Gilbert syndrome. Journal of gastroenterology and hepatology. 2016 Feb:31(2):403-8. doi: 10.1111/jgh.13071. Epub
[PubMed PMID: 26250421]
[24]
Flaherman VJ, Maisels MJ, Academy of Breastfeeding Medicine. ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant 35 Weeks or More of Gestation-Revised 2017. Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine. 2017 Jun:12(5):250-257. doi: 10.1089/bfm.2017.29042.vjf. Epub 2017 Apr 10
[PubMed PMID: 29624434]
[25]
Grunebaum E, Amir J, Merlob P, Mimouni M, Varsano I. Breast mild jaundice: natural history, familial incidence and late neurodevelopmental outcome of the infant. European journal of pediatrics. 1991 Feb:150(4):267-70
[PubMed PMID: 2029918]
[26]
Preer GL, Philipp BL. Understanding and managing breast milk jaundice. Archives of disease in childhood. Fetal and neonatal edition. 2011 Nov:96(6):F461-6. doi: 10.1136/adc.2010.184416. Epub 2010 Aug 5
[PubMed PMID: 20688866]
Level 3 (low-level) evidence
[27]
Rubarth LB. Infants of diabetic mothers. Neonatal network : NN. 2013 Nov-Dec:32(6):416-8. doi: 10.1891/0730-0832.32.6.416. Epub
[PubMed PMID: 24195802]
[28]
Amin SB. Clinical assessment of bilirubin-induced neurotoxicity in premature infants. Seminars in perinatology. 2004 Oct:28(5):340-7
[PubMed PMID: 15686265]
[29]
Maisels MJ, Kring E. Risk of sepsis in newborns with severe hyperbilirubinemia. Pediatrics. 1992 Nov:90(5):741-3
[PubMed PMID: 1408547]
[30]
Hansen TW. Therapeutic approaches to neonatal jaundice: an international survey. Clinical pediatrics. 1996 Jun:35(6):309-16
[PubMed PMID: 8782955]
Level 3 (low-level) evidence
[31]
Maisels MJ, Watchko JF, Bhutani VK, Stevenson DK. An approach to the management of hyperbilirubinemia in the preterm infant less than 35 weeks of gestation. Journal of perinatology : official journal of the California Perinatal Association. 2012 Sep:32(9):660-4. doi: 10.1038/jp.2012.71. Epub 2012 Jun 7
[PubMed PMID: 22678141]
[33]
Hegyi T, Goldie E, Hiatt M. The protective role of bilirubin in oxygen-radical diseases of the preterm infant. Journal of perinatology : official journal of the California Perinatal Association. 1994 Jul-Aug:14(4):296-300
[PubMed PMID: 7965225]
[34]
Beal JA. American Academy of Pediatrics' Updated Clinical Guidelines for Managing Neonatal Hyperbilirubinemia. MCN. The American journal of maternal child nursing. 2023 Jan-Feb 01:48(1):49. doi: 10.1097/NMC.0000000000000874. Epub
[PubMed PMID: 36469895]
[35]
Fawaz R, Baumann U, Ekong U, Fischler B, Hadzic N, Mack CL, McLin VA, Molleston JP, Neimark E, Ng VL, Karpen SJ. Guideline for the Evaluation of Cholestatic Jaundice in Infants: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. Journal of pediatric gastroenterology and nutrition. 2017 Jan:64(1):154-168. doi: 10.1097/MPG.0000000000001334. Epub
[PubMed PMID: 27429428]
[36]
Plosa EJ, Esbenshade JC, Fuller MP, Weitkamp JH. Cytomegalovirus infection. Pediatrics in review. 2012 Apr:33(4):156-63; quiz 163. doi: 10.1542/pir.33-4-156. Epub
[PubMed PMID: 22474112]
[37]
Roelofsen H, van der Veere CN, Ottenhoff R, Schoemaker B, Jansen PL, Oude Elferink RP. Decreased bilirubin transport in the perfused liver of endotoxemic rats. Gastroenterology. 1994 Oct:107(4):1075-84
[PubMed PMID: 7926459]
[38]
Pan DH, Rivas Y. Jaundice: Newborn to Age 2 Months. Pediatrics in review. 2017 Nov:38(11):499-510. doi: 10.1542/pir.2015-0132. Epub
[PubMed PMID: 29093118]
[39]
The NS, Honein MA, Caton AR, Moore CA, Siega-Riz AM, Druschel CM, National Birth Defects Prevention Study. Risk factors for isolated biliary atresia, National Birth Defects Prevention Study, 1997-2002. American journal of medical genetics. Part A. 2007 Oct 1:143A(19):2274-84
[PubMed PMID: 17726689]
[40]
Takamizawa S, Zaima A, Muraji T, Kanegawa K, Akasaka Y, Satoh S, Nishijima E. Can biliary atresia be diagnosed by ultrasonography alone? Journal of pediatric surgery. 2007 Dec:42(12):2093-6
[PubMed PMID: 18082715]
[41]
Serinet MO, Wildhaber BE, Broué P, Lachaux A, Sarles J, Jacquemin E, Gauthier F, Chardot C. Impact of age at Kasai operation on its results in late childhood and adolescence: a rational basis for biliary atresia screening. Pediatrics. 2009 May:123(5):1280-6. doi: 10.1542/peds.2008-1949. Epub
[PubMed PMID: 19403492]
[42]
Balistreri WF, Bezerra JA. Whatever happened to "neonatal hepatitis"? Clinics in liver disease. 2006 Feb:10(1):27-53, v
[PubMed PMID: 16376793]
[43]
Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, Pawlik TM. Choledochal cysts: presentation, clinical differentiation, and management. Journal of the American College of Surgeons. 2014 Dec:219(6):1167-80. doi: 10.1016/j.jamcollsurg.2014.04.023. Epub 2014 Jun 27
[PubMed PMID: 25442379]
[44]
Amedee-Manesme O, Bernard O, Brunelle F, Hadchouel M, Polonovski C, Baudon JJ, Beguet P, Alagille D. Sclerosing cholangitis with neonatal onset. The Journal of pediatrics. 1987 Aug:111(2):225-9
[PubMed PMID: 3612394]
[45]
Ljung R, Ivarsson S, Nilsson P, Solvig J, Wattsgård C, Borulf S. Cholelithiasis during the first year of life: case reports and literature review. Acta paediatrica (Oslo, Norway : 1992). 1992 Jan:81(1):69-72
[PubMed PMID: 1600308]
Level 3 (low-level) evidence
[46]
Jesina D. Alagille Syndrome: An Overview. Neonatal network : NN. 2017 Nov 1:36(6):343-347. doi: 10.1891/0730-0832.36.6.343. Epub
[PubMed PMID: 29185945]
Level 3 (low-level) evidence
[47]
Emerick KM, Rand EB, Goldmuntz E, Krantz ID, Spinner NB, Piccoli DA. Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology (Baltimore, Md.). 1999 Mar:29(3):822-9
[PubMed PMID: 10051485]
[48]
Li L, Wang NL, Gong JY, Wang JS. [Infantile cholestasis caused by CFTR mutation: case report and literature review]. Zhonghua er ke za zhi = Chinese journal of pediatrics. 2016 Nov 2:54(11):851-855. doi: 10.3760/cma.j.issn.0578-1310.2016.11.013. Epub
[PubMed PMID: 27806795]
Level 3 (low-level) evidence
[49]
Townsend S, Newsome P, Turner AM. Presentation and prognosis of liver disease in alpha-1 antitrypsin deficiency. Expert review of gastroenterology & hepatology. 2018 Aug:12(8):745-747. doi: 10.1080/17474124.2018.1477589. Epub 2018 May 28
[PubMed PMID: 29768056]
[50]
Karadag N, Zenciroglu A, Eminoglu FT, Dilli D, Karagol BS, Kundak A, Dursun A, Hakan N, Okumus N. Literature review and outcome of classic galactosemia diagnosed in the neonatal period. Clinical laboratory. 2013:59(9-10):1139-46
[PubMed PMID: 24273939]
[51]
Chinsky JM, Singh R, Ficicioglu C, van Karnebeek CDM, Grompe M, Mitchell G, Waisbren SE, Gucsavas-Calikoglu M, Wasserstein MP, Coakley K, Scott CR. Diagnosis and treatment of tyrosinemia type I: a US and Canadian consensus group review and recommendations. Genetics in medicine : official journal of the American College of Medical Genetics. 2017 Dec:19(12):. doi: 10.1038/gim.2017.101. Epub 2017 Aug 3
[PubMed PMID: 28771246]
Level 3 (low-level) evidence
[52]
Jacquemin E. Progressive familial intrahepatic cholestasis. Genetic basis and treatment. Clinics in liver disease. 2000 Nov:4(4):753-63
[PubMed PMID: 11232355]
[53]
Davit-Spraul A, Gonzales E, Baussan C, Jacquemin E. Progressive familial intrahepatic cholestasis. Orphanet journal of rare diseases. 2009 Jan 8:4():1. doi: 10.1186/1750-1172-4-1. Epub 2009 Jan 8
[PubMed PMID: 19133130]
[54]
Bull LN, Roche E, Song EJ, Pedersen J, Knisely AS, van Der Hagen CB, Eiklid K, Aagenaes O, Freimer NB. Mapping of the locus for cholestasis-lymphedema syndrome (Aagenaes syndrome) to a 6.6-cM interval on chromosome 15q. American journal of human genetics. 2000 Oct:67(4):994-9
[PubMed PMID: 10968776]
[55]
Strassburg CP. Hyperbilirubinemia syndromes (Gilbert-Meulengracht, Crigler-Najjar, Dubin-Johnson, and Rotor syndrome). Best practice & research. Clinical gastroenterology. 2010 Oct:24(5):555-71. doi: 10.1016/j.bpg.2010.07.007. Epub
[PubMed PMID: 20955959]
[56]
Lauriti G, Zani A, Aufieri R, Cananzi M, Chiesa PL, Eaton S, Pierro A. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: a systematic review. JPEN. Journal of parenteral and enteral nutrition. 2014 Jan:38(1):70-85. doi: 10.1177/0148607113496280. Epub 2013 Jul 26
[PubMed PMID: 23894170]
Level 1 (high-level) evidence
[57]
Buchman AL, Iyer K, Fryer J. Parenteral nutrition-associated liver disease and the role for isolated intestine and intestine/liver transplantation. Hepatology (Baltimore, Md.). 2006 Jan:43(1):9-19
[PubMed PMID: 16374841]
[58]
Duerksen DR, Van Aerde JE, Chan G, Thomson AB, Jewell LJ, Clandinin MT. Total parenteral nutrition impairs bile flow and alters bile composition in newborn piglet. Digestive diseases and sciences. 1996 Sep:41(9):1864-70
[PubMed PMID: 8794808]
[59]
Pan X, Kelly S, Melin-Aldana H, Malladi P, Whitington PF. Novel mechanism of fetal hepatocyte injury in congenital alloimmune hepatitis involves the terminal complement cascade. Hepatology (Baltimore, Md.). 2010 Jun:51(6):2061-8. doi: 10.1002/hep.23581. Epub
[PubMed PMID: 20512994]
[60]
Feldman AG, Whitington PF. Neonatal hemochromatosis. Journal of clinical and experimental hepatology. 2013 Dec:3(4):313-20. doi: 10.1016/j.jceh.2013.10.004. Epub 2013 Nov 27
[PubMed PMID: 25755519]
[61]
Bhutani VK, Stark AR, Lazzeroni LC, Poland R, Gourley GR, Kazmierczak S, Meloy L, Burgos AE, Hall JY, Stevenson DK, Initial Clinical Testing Evaluation and Risk Assessment for Universal Screening for Hyperbilirubinemia Study Group. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. The Journal of pediatrics. 2013 Mar:162(3):477-482.e1. doi: 10.1016/j.jpeds.2012.08.022. Epub 2012 Oct 5
[PubMed PMID: 23043681]
[62]
Bhutani VK. Editorial: building evidence to manage newborn jaundice worldwide. Indian journal of pediatrics. 2012 Feb:79(2):253-5. doi: 10.1007/s12098-011-0631-6. Epub 2011 Dec 20
[PubMed PMID: 22183759]
Level 3 (low-level) evidence
[63]
Alkhotani A, Eldin EE, Zaghloul A, Mujahid S. Evaluation of neonatal jaundice in the Makkah region. Scientific reports. 2014 Apr 25:4():4802. doi: 10.1038/srep04802. Epub 2014 Apr 25
[PubMed PMID: 24763104]
[64]
Winfield CR, MacFaul R. Clinical study of prolonged jaundice in breast- and bottle-fed babies. Archives of disease in childhood. 1978 Jun:53(6):506-7
[PubMed PMID: 686778]
[65]
Sgro M, Campbell D, Shah V. Incidence and causes of severe neonatal hyperbilirubinemia in Canada. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2006 Sep 12:175(6):587-90
[PubMed PMID: 16966660]
[66]
Ding G, Zhang S, Yao D, Na Q, Wang H, Li L, Yang L, Huang W, Wang Y, Xu J. An epidemiological survey on neonatal jaundice in China. Chinese medical journal. 2001 Apr:114(4):344-7
[PubMed PMID: 11780450]
Level 2 (mid-level) evidence
[67]
Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, Bell J, Mori R, Slusher TM, Fahmy N, Paul VK, Du L, Okolo AA, de Almeida MF, Olusanya BO, Kumar P, Cousens S, Lawn JE. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatric research. 2013 Dec:74 Suppl 1(Suppl 1):86-100. doi: 10.1038/pr.2013.208. Epub
[PubMed PMID: 24366465]
[68]
Moore LG, Newberry MA, Freeby GM, Crnic LS. Increased incidence of neonatal hyperbilirubinemia at 3,100 m in Colorado. American journal of diseases of children (1960). 1984 Feb:138(2):157-61
[PubMed PMID: 6695871]
[69]
Drew JH, Barrie J, Horacek I, Kitchen WH. Factors influencing jaundice in immigrant Greek infants. Archives of disease in childhood. 1978 Jan:53(1):49-52
[PubMed PMID: 626518]
[70]
. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants (35 or more weeks' gestation) - Summary. Paediatrics & child health. 2007 May:12(5):401-18
[PubMed PMID: 19030400]
[71]
Watchko JF, Tiribelli C. Bilirubin-induced neurologic damage--mechanisms and management approaches. The New England journal of medicine. 2013 Nov 21:369(21):2021-30. doi: 10.1056/NEJMra1308124. Epub
[PubMed PMID: 24256380]
[72]
Dick MC, Mowat AP. Hepatitis syndrome in infancy--an epidemiological survey with 10 year follow up. Archives of disease in childhood. 1985 Jun:60(6):512-6
[PubMed PMID: 3874604]
Level 2 (mid-level) evidence
[73]
Gottesman LE, Del Vecchio MT, Aronoff SC. Etiologies of conjugated hyperbilirubinemia in infancy: a systematic review of 1692 subjects. BMC pediatrics. 2015 Nov 20:15():192. doi: 10.1186/s12887-015-0506-5. Epub 2015 Nov 20
[PubMed PMID: 26589959]
Level 1 (high-level) evidence
[74]
D'Alessandro AM, Knechtle SJ, Chin LT, Fernandez LA, Yagci G, Leverson G, Kalayoglu M. Liver transplantation in pediatric patients: twenty years of experience at the University of Wisconsin. Pediatric transplantation. 2007 Sep:11(6):661-70
[PubMed PMID: 17663691]
[75]
Dennery PA, Seidman DS, Stevenson DK. Neonatal hyperbilirubinemia. The New England journal of medicine. 2001 Feb 22:344(8):581-90
[PubMed PMID: 11207355]
[76]
Poland RL, Odell GB. Physiologic jaundice: the enterohepatic circulation of bilirubin. The New England journal of medicine. 1971 Jan 7:284(1):1-6
[PubMed PMID: 4922346]
[78]
Chuniaud L, Dessante M, Chantoux F, Blondeau JP, Francon J, Trivin F. Cytotoxicity of bilirubin for human fibroblasts and rat astrocytes in culture. Effect of the ratio of bilirubin to serum albumin. Clinica chimica acta; international journal of clinical chemistry. 1996 Dec 30:256(2):103-14
[PubMed PMID: 9027422]
[79]
Amato MM, Kilguss NV, Gelardi NL, Cashore WJ. Dose-effect relationship of bilirubin on striatal synaptosomes in rats. Biology of the neonate. 1994:66(5):288-93
[PubMed PMID: 7873694]
[80]
Hoffman DJ, Zanelli SA, Kubin J, Mishra OP, Delivoria-Papadopoulos M. The in vivo effect of bilirubin on the N-methyl-D-aspartate receptor/ion channel complex in the brains of newborn piglets. Pediatric research. 1996 Dec:40(6):804-8
[PubMed PMID: 8947954]
[81]
Benchimol EI, Walsh CM, Ling SC. Early diagnosis of neonatal cholestatic jaundice: test at 2 weeks. Canadian family physician Medecin de famille canadien. 2009 Dec:55(12):1184-92
[PubMed PMID: 20008595]
[82]
Trauner M, Meier PJ, Boyer JL. Molecular pathogenesis of cholestasis. The New England journal of medicine. 1998 Oct 22:339(17):1217-27
[PubMed PMID: 9780343]
[83]
Chen HL, Wu SH, Hsu SH, Liou BY, Chen HL, Chang MH. Jaundice revisited: recent advances in the diagnosis and treatment of inherited cholestatic liver diseases. Journal of biomedical science. 2018 Oct 26:25(1):75. doi: 10.1186/s12929-018-0475-8. Epub 2018 Oct 26
[PubMed PMID: 30367658]
Level 3 (low-level) evidence
[84]
Hamza A. Kernicterus. Autopsy & case reports. 2019 Jan-Mar:9(1):e2018057. doi: 10.4322/acr.2018.057. Epub 2019 Jan 14
[PubMed PMID: 30863731]
Level 3 (low-level) evidence
[85]
Vij M, Rela M. Biliary atresia: pathology, etiology and pathogenesis. Future science OA. 2020 Mar 17:6(5):FSO466. doi: 10.2144/fsoa-2019-0153. Epub 2020 Mar 17
[PubMed PMID: 32518681]
[86]
Matthai J, Paul S. Evaluation of cholestatic jaundice in young infants. Indian pediatrics. 2001 Aug:38(8):893-8
[PubMed PMID: 11521001]
[87]
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Stark AR, Watchko JF. Hyperbilirubinemia in the newborn infant } or =35 weeks' gestation: an update with clarifications. Pediatrics. 2009 Oct:124(4):1193-8. doi: 10.1542/peds.2009-0329. Epub 2009 Sep 28
[PubMed PMID: 19786452]
[88]
Johnson L, Bhutani VK. Guidelines for management of the jaundiced term and near-term infant. Clinics in perinatology. 1998 Sep:25(3):555-74, viii
[PubMed PMID: 9779334]
[89]
Kemper AR, Newman TB, Slaughter JL, Maisels MJ, Watchko JF, Downs SM, Grout RW, Bundy DG, Stark AR, Bogen DL, Holmes AV, Feldman-Winter LB, Bhutani VK, Brown SR, Maradiaga Panayotti GM, Okechukwu K, Rappo PD, Russell TL. Clinical Practice Guideline Revision: Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. Pediatrics. 2022 Sep 1:150(3):. pii: e2022058859. doi: 10.1542/peds.2022-058859. Epub
[PubMed PMID: 35927462]
Level 1 (high-level) evidence
[90]
Wainer S, Rabi Y, Parmar SM, Allegro D, Lyon M. Impact of skin tone on the performance of a transcutaneous jaundice meter. Acta paediatrica (Oslo, Norway : 1992). 2009 Dec:98(12):1909-15. doi: 10.1111/j.1651-2227.2009.01497.x. Epub 2009 Sep 17
[PubMed PMID: 19764923]
[91]
Casnocha Lucanova L, Matasova K, Zibolen M, Krcho P. Accuracy of transcutaneous bilirubin measurement in newborns after phototherapy. Journal of perinatology : official journal of the California Perinatal Association. 2016 Oct:36(10):858-61. doi: 10.1038/jp.2016.91. Epub 2016 Jun 9
[PubMed PMID: 27279078]
[92]
Hulzebos CV, Dijk PH, van Imhoff DE, Bos AF, Lopriore E, Offringa M, Ruiter SA, van Braeckel KN, Krabbe PF, Quik EH, van Toledo-Eppinga L, Nuytemans DH, van Wassenaer-Leemhuis AG, Benders MJ, Korbeeck-van Hof KK, van Lingen RA, Groot Jebbink LJ, Liem D, Mansvelt P, Buijs J, Govaert P, van Vliet I, Mulder TL, Wolfs C, Fetter WP, Laarman C, BARTrial Study Group. The bilirubin albumin ratio in the management of hyperbilirubinemia in preterm infants to improve neurodevelopmental outcome: a randomized controlled trial--BARTrial. PloS one. 2014:9(6):e99466. doi: 10.1371/journal.pone.0099466. Epub 2014 Jun 13
[PubMed PMID: 24927259]
Level 1 (high-level) evidence
[93]
Steinborn M, Seelos KC, Heuck A, von Voss H, Reiser M. MR findings in a patient with Kernicterus. European radiology. 1999:9(9):1913-5
[PubMed PMID: 10602975]
[94]
McKiernan PJ, Baker AJ, Kelly DA. The frequency and outcome of biliary atresia in the UK and Ireland. Lancet (London, England). 2000 Jan 1:355(9197):25-9
[PubMed PMID: 10615887]
[95]
Morotti RA, Jain D. Pediatric Cholestatic Disorders: Approach to Pathologic Diagnosis. Surgical pathology clinics. 2013 Jun:6(2):205-25. doi: 10.1016/j.path.2013.03.001. Epub 2013 May 4
[PubMed PMID: 26838972]
[96]
Bhutani VK, Committee on Fetus and Newborn, American Academy of Pediatrics. Phototherapy to prevent severe neonatal hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2011 Oct:128(4):e1046-52. doi: 10.1542/peds.2011-1494. Epub 2011 Sep 26
[PubMed PMID: 21949150]
[97]
Yetman RJ, Parks DK, Huseby V, Mistry K, Garcia J. Rebound bilirubin levels in infants receiving phototherapy. The Journal of pediatrics. 1998 Nov:133(5):705-7
[PubMed PMID: 9821435]
[98]
Newman TB, Wu YW, Kuzniewicz MW, Grimes BA, McCulloch CE. Childhood Seizures After Phototherapy. Pediatrics. 2018 Oct:142(4):. pii: e20180648. doi: 10.1542/peds.2018-0648. Epub
[PubMed PMID: 30249623]
[99]
Newman TB, Wickremasinghe AC, Walsh EM, Grimes BA, McCulloch CE, Kuzniewicz MW. Retrospective Cohort Study of Phototherapy and Childhood Cancer in Northern California. Pediatrics. 2016 Jun:137(6):. pii: e20151354. doi: 10.1542/peds.2015-1354. Epub
[PubMed PMID: 27217477]
Level 2 (mid-level) evidence
[100]
Auger N, Laverdière C, Ayoub A, Lo E, Luu TM. Neonatal phototherapy and future risk of childhood cancer. International journal of cancer. 2019 Oct 15:145(8):2061-2069. doi: 10.1002/ijc.32158. Epub 2019 Feb 8
[PubMed PMID: 30684392]
[101]
Wang J, Guo G, Li A, Cai WQ, Wang X. Challenges of phototherapy for neonatal hyperbilirubinemia (Review). Experimental and therapeutic medicine. 2021 Mar:21(3):231. doi: 10.3892/etm.2021.9662. Epub 2021 Jan 20
[PubMed PMID: 33613704]
[102]
Itoh S, Okada H, Kuboi T, Kusaka T. Phototherapy for neonatal hyperbilirubinemia. Pediatrics international : official journal of the Japan Pediatric Society. 2017 Sep:59(9):959-966. doi: 10.1111/ped.13332. Epub 2017 Aug 7
[PubMed PMID: 28563973]
[104]
Pearson CH. Replacement transfusion as a treatment of erythroblastosis fetalis, by Louis K. Diamond, MD, Pediatrics, 1948;2:520-524. Pediatrics. 1998 Jul:102(1 Pt 2):203-5
[PubMed PMID: 9651427]
[105]
Hansen TWR, Maisels MJ, Ebbesen F, Vreman HJ, Stevenson DK, Wong RJ, Bhutani VK. Sixty years of phototherapy for neonatal jaundice - from serendipitous observation to standardized treatment and rescue for millions. Journal of perinatology : official journal of the California Perinatal Association. 2020 Feb:40(2):180-193. doi: 10.1038/s41372-019-0439-1. Epub 2019 Aug 16
[PubMed PMID: 31420582]
[106]
DIAMOND LK, ALLEN FH Jr, THOMAS WO Jr. Erythroblastosis fetalis. VII. Treatment with exchange transfusion. The New England journal of medicine. 1951 Jan 11:244(2):39-49
[PubMed PMID: 14785788]
[107]
Jackson JC. Adverse events associated with exchange transfusion in healthy and ill newborns. Pediatrics. 1997 May:99(5):E7
[PubMed PMID: 9113964]
[108]
Patra K, Storfer-Isser A, Siner B, Moore J, Hack M. Adverse events associated with neonatal exchange transfusion in the 1990s. The Journal of pediatrics. 2004 May:144(5):626-31
[PubMed PMID: 15126997]
[109]
Alpay F, Sarici SU, Okutan V, Erdem G, Ozcan O, Gökçay E. High-dose intravenous immunoglobulin therapy in neonatal immune haemolytic jaundice. Acta paediatrica (Oslo, Norway : 1992). 1999 Feb:88(2):216-9
[PubMed PMID: 10102158]
[110]
Gottstein R, Cooke RW. Systematic review of intravenous immunoglobulin in haemolytic disease of the newborn. Archives of disease in childhood. Fetal and neonatal edition. 2003 Jan:88(1):F6-10
[PubMed PMID: 12496219]
Level 1 (high-level) evidence
[112]
Karthik SV, Campbell-Davidson D, Isherwood D. Carotenemia in infancy and its association with prevalent feeding practices. Pediatric dermatology. 2006 Nov-Dec:23(6):571-3
[PubMed PMID: 17156001]
[113]
Riskin A, Tamir A, Kugelman A, Hemo M, Bader D. Is visual assessment of jaundice reliable as a screening tool to detect significant neonatal hyperbilirubinemia? The Journal of pediatrics. 2008 Jun:152(6):782-7, 787.e1-2. doi: 10.1016/j.jpeds.2007.11.003. Epub 2008 Jan 22
[PubMed PMID: 18492516]
[114]
Khurshid F, Rao SP, Sauve C, Gupta S. Universal screening for hyperbilirubinemia in term healthy newborns at discharge: A systematic review and meta-analysis. Journal of global health. 2022 Dec 29:12():12007. doi: 10.7189/jogh.12.12007. Epub 2022 Dec 29
[PubMed PMID: 36579719]
Level 1 (high-level) evidence
[115]
Rand EB, Karpen SJ, Kelly S, Mack CL, Malatack JJ, Sokol RJ, Whitington PF. Treatment of neonatal hemochromatosis with exchange transfusion and intravenous immunoglobulin. The Journal of pediatrics. 2009 Oct:155(4):566-71. doi: 10.1016/j.jpeds.2009.04.012. Epub 2009 Jun 28
[PubMed PMID: 19560784]
[116]
Hankø E, Hansen TW, Almaas R, Lindstad J, Rootwelt T. Bilirubin induces apoptosis and necrosis in human NT2-N neurons. Pediatric research. 2005 Feb:57(2):179-84
[PubMed PMID: 15611354]
[117]
Olusanya BO, Slusher TM, Imosemi DO, Emokpae AA. Maternal detection of neonatal jaundice during birth hospitalization using a novel two-color icterometer. PloS one. 2017:12(8):e0183882. doi: 10.1371/journal.pone.0183882. Epub 2017 Aug 24
[PubMed PMID: 28837635]