Introduction
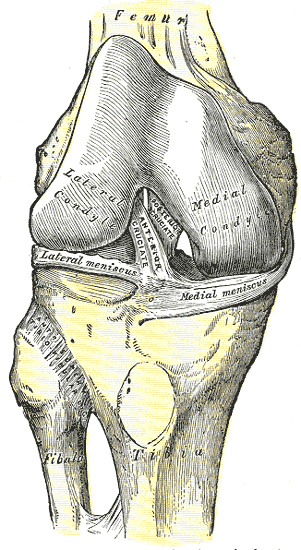
The knee is the largest joint in the body. It is a compound synovial joint that consists of the tibiofemoral joint and the patellofemoral joint. It primarily serves as a hinge joint which allows flexion and extension as well as various other movements. It joins the lower leg and thigh bilaterally and is an essential component of efficient bipedal movements such as walking, running, and jumping. The anatomical function and stability of the knee depend on muscles, bones, ligaments, cartilage, synovial tissue, synovial fluid, and other connective tissues. The 4 main stabilizing ligaments of the knee are the anterior cruciate (ACL), posterior cruciate (PCL), medial collateral (MCL), and lateral collateral (LCL). The ACL attaches at the lateral condyle of the femur and the intercondyloid eminence of the tibia and functions to prevent anterior translation of the tibia on the femur. The PCL attaches at the medial condyle of the femur and the posterior intercondylar area of the tibia and functions to prevent forward displacement of the femur on the tibia.[1][2][3][4]
The MCL attaches at the medial epicondyle of the femur and the medial condyle of the tibia and functions to prevent valgus stress on the knee. The LCL attaches at the lateral epicondyle of the femur and the head of the fibula and functions to prevent varus stress on the knee. The medial and lateral menisci are 2 separate fibrocartilage structures that are located between the articular surfaces of the tibia and femur. They function as shock absorbers, static stabilizers, and friction reducers during articulation. The knee’s bony structures include the distal end of the femur, proximal end of the tibia, and patella. The patella is the largest sesamoid bone in the body and functions as an attachment point for the quadriceps tendon and patellar ligament. It also protects the anterior articular surface of the femoral portion of the knee. The knee contains multiple bursas, which serve to reduce friction between structures of the knee. Bursas are small sacs made up of synovial membranes and contain synovial fluid. Many of these structures mentioned above are part of the articular capsule, which serves to stabilize the knee further and contain synovial fluid. Synovial fluid is made by synovial membranes and serves to reduce friction between articular surfaces of the knee.
Structure and Function
The knee is a weight-bearing joint that serves to allow flexion and extension of the lower leg around a transverse axis in a sagittal plane. During this motion, the tibial condyles articulate with the femoral condyles as well as the medial and lateral menisci. Also, the patella articulates with the femoral trochlear groove. The knee secondarily allows for internal and external rotation, compression and distraction, anterior and posterior translation, medial and lateral translation, and varus and valgus movements. The tendonous and ligamentous structures of the knee are lubricated by bursae. The names of the bursae correspond with their location within the knee. The prepatellar bursa is located between the patella and the overlying subcutaneous tissue. The infrapatellar bursa has a superficial and deep component. The superficial infrapatellar bursa is located between the tibial tubercle and the overlying skin. The deep infrapatellar bursa is located between the posterior aspect of the patellar tendon and the tibia. The suprapatellar bursa is located between the quadriceps tendon and the femur. The pes anserinus bursa is located on the anteromedial aspect of the tibia, on the medial tibial epicondyle. Within the layers of the medial collateral ligament is the medial collateral ligament bursa. The iliotibial bursa is located on the distal iliotibial band by its insertion on the Gerdy tubercle. The popliteal bursa is located in the popliteal hiatus by the proximal popliteal tendon. Although the knee is an inherently unstable joint, it has many dynamic stabilizers (muscles) and static stabilizers (ligaments).[5][6]
Embryology
At 2 weeks of development, the structures which make up the knee begin to develop from the mesoderm. Around the sixth week of development, chondrocytes have developed the cartilage form of the femur and tibia. Primary ossification centers are present in all long bones by twelve weeks of development. The ligaments, menisci, and other connective tissue develop from mesenchyme and become distinct from one another by week ten of development. The muscles and neurovascular components which contribute to the knee begin to develop from the mesoderm around week 4.
Blood Supply and Lymphatics
The structures of the knee receive much of their blood supply from a plexus of arteries with branches from the popliteal artery and femoral artery. The popliteal artery branches off the superficial femoral artery and runs posteriorly across the knee joint. The superior medial, inferior medial, superior lateral, and inferior lateral genicular arteries branch off the popliteal artery and travel anteriorly to anastomose with other parts of the plexus. Also, a descending genicular artery branches off the superficial femoral artery and anastomoses anteriorly with the other genicular arteries. The anterior and posterior tibial recurrent arteries travel laterally from the anterior tibial artery and also contribute to the plexus. The middle genicular artery travels directly into the joint. In addition, the sural arteries branch off the popliteal artery and travel inferiorly away from the midline. The flexor muscles are supplied mainly by the inferior gluteal, perforating, popliteal, deep femoral, and sural arteries. The femoral artery primarily supplies the extensor muscles.
Much of the lymphatic drainage from the knee and lower leg travel to the popliteal lymph nodes in the popliteal fossa. The popliteal nodes, along with other knee and lower limb lymphatics, drain into the deep inguinal and sub inguinal nodes. The lymphatic system primarily follows vasculature.
Nerves
The structures of the knee and most of the flexor muscles receive innervation from branches of the femoral nerve (L1, L2, L3). The extensor muscles receive innervation from the sciatic nerve (L4, L5, S1, S2, S3), which branches into the tibial nerve and common peroneal nerve.
Muscles
The flexors include the articularis genus, rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis. These muscles originate from various locations on the femur and anterior inferior iliac spine. The latter 4 conjoin to form the patellar tendon/ligament, which crosses the knee anteriorly and inserts on the patella and tibial tuberosity.
The extensors include the biceps femoris, semitendinosus, semimembranosus, gastrocnemius, plantaris, gracilis, and popliteus. These muscles originate from the ischial tuberosity, inferior pubic ramus, and different locations on the femur. They insert on various locations of the tibia, fibula, and calcaneus.
Physiologic Variants
Children often have genu varum (bowleg) or genu valgum (knock knee) which are considered normal during certain age ranges. If these conditions persist past a certain age, they are deemed pathologic and may require bracing and surgical treatment. Some individuals suffer from ligamentous laxity that is primary or secondary to connective tissue disorders such as Ehlers Danlos. These individuals are at an increased risk for knee dislocations and other hypermobility injuries that can lead to chronic knee pain. Skeletal dysplasia is often congenital and encompasses hundreds of different diseases that may affect structures of the knee significantly, luckily most of them are rare. There are variants of each knee structure that have the potential to alter the biomechanics of the entire knee.[7]
Surgical Considerations
Ligamentous and meniscal tears are among the most common knee injuries and typically require surgical intervention. Often, ligament repairs are done arthroscopically, with a number of different grafts such as hamstring, patellar, and allografts being used to repair the defect. Each graft poses advantages and disadvantages. Ligamentous repairs commonly require extensive rehabilitation, and athletes routinely wear a brace during an activity to prevent reoccurrence. Arthroscopy is also used to repair meniscal tears or, more commonly, to perform a meniscectomy on the damaged meniscus. Meniscectomy is a faster recovery but still requires some rehabilitation. One of the main functions of ligamentous structures and menisci is to provide stability to the joint. When these structures become compromised, the articular surfaces of the knee can be more prone to sustain damage that may lead to osteoarthritis. Osteoarthritis is another form of knee pathology that can be treated surgically. There are various factors such as genetics, weight, activity, and previous injury that may contribute to and predispose an individual to osteoarthritis. Ultimately, this condition can cause great pain and discomfort with a significant decrease in functionality and quality of life. A total knee arthroplasty can be performed to treat this condition. The surgery involves the replacement of all articular surfaces of the knee with prosthetics made of metal, ceramic, or plastic. This type of surgery is more prevalent in the older population and requires extensive rehabilitation as well.[8][9][10]
Clinical Significance
The ACL is the most commonly injured ligament and usually occurs during a non-contact event. The mechanism of injury often involves an athlete changing direction with a slight pivoting motion that introduces rotational force to a planted leg. Many patients that experience this injury report feeling and hearing a “pop” that accompanies immediate pain followed by effusion. The Lachman and anterior drawer tests are popular clinical tests used to assess for an ACL injury. MRI is the most useful imaging modality when trying to detect an ACL injury. In the young and active population, an ACL tear is usually repaired surgically to maintain stability when participating in athletic activities. In the older or less active population, an ACL tear can be treated conservatively with activity modification and physical therapy.
A meniscal tear is another very common knee injury that frequently has the same injury mechanism as an ACL tear, a pivoting motion on a planted foot. Meniscal tears may also occur in older patients as a result of degenerative changes. Sometimes the individual will notice when the injury occurs, and other times they may be unaware. It is common for a meniscal tear to accompany other knee injuries such as ligament tears. Typically, pain and effusion accompany the injury, and sometimes patients complain of knee clicking, locking, and catching during activity. Treatment is variable with each patient and ranges from conservative treatment to surgery. The McMurray test is the most used clinical technique to detect the presence of meniscal tears, with MRI being the most accurate imaging modality.
MCL injuries are also common ligamentous injuries of the knee but tend to have a different injury mechanism and treatment path. The MCL is usually injured when direct force to the lateral aspect of the knee induces excessive valgus stress. Pain usually accompanies the injury, and effusion often follows. Introducing valgus stress in a clinical setting reproduces pain with an MCL injury, along with history qualifies diagnosis. MRI can be used to confirm an MCL injury and to rule out associated injuries. Treatment frequently is conservative, with the use of a brace and non-weight-bearing activity.
The PCL is the largest and strongest ligament in the knee and is uncommonly involved in an isolated injury. A great amount of force is usually required to injure the PCL, often injuring other structures as well. The mechanism of injury entails a direct posterior force applied to a flexed knee and commonly occurs in high-energy trauma. The posterior drawer test is an examination technique used to assess for a PCL injury. Management is much like the ACL, and it can be treated conservatively or surgically depending on the patient.
Osteoarthritis of the knee is another very prevalent disease in the older population but can be seen in middle-aged patients as well. As discussed in the previous section, there are a number of factors that contribute to the timing and severity of osteoarthritis. The disease is usually chronic, and patients often complain of stiffness and pain with activity that gradually worsens over time. X-ray is the most commonly used imaging modality, and patients will often have pain with ROM testing on clinical exam. Treatment is usually started conservatively with bodyweight reduction, NSAIDS, physical therapy, and steroids. As these remedies begin to fail, a total knee arthroplasty can be performed. Although a total knee arthroplasty is a big procedure, it is overall very successful at improving the quality of life of patients that suffer from debilitating osteoarthritis.
The patellar femoral joint can often be another source of knee pathology. Patellar-femoral pain syndrome is one of the most common presenting knee complaints to sports medicine and primary care providers. This is pain that is located on the anterior aspect of the knee, and it's often aggravated by flexion of the weight-bearing knee during activities such as running, climbing stairs, or jumping. The pathophysiology of the condition is not clearly understood but is thought to be related to factors such as overuse, muscle imbalance, and improper patellar tracking. The diagnosis is made clinically, and imaging is typically only done to rule out other conditions. Treatment involves rest, stretching, physical therapy, and gradual return to activity.
Knee dislocations occur at the patellar-femoral joint and tibiofemoral joint. The latter is a much more severe injury and requires emergency medical treatment. A tibiofemoral dislocation is the result of a large amount of force and results in multiple knee structures being severely damaged. X-ray and MRI are used to assess the extent of the injury. Popliteal artery damage is the most urgent complication and must be repaired quickly to prevent irreversible deficits. Pulse, ankle-brachial index and ultrasound should be used initially to assess for artery damage. A closed or open reduction can be performed depending on the extent and details of the dislocation. The reduction may also occur spontaneously. Treatments vary; however, surgery is commonly required for the repair of the associated structures.
Other Issues
With the prevalence of knee injuries, there are constant attempts to introduce new and effective treatments. Platelet-rich plasma (PRP) is one of these new controversial treatments being investigated. Data is limited, and research remains early in the process, but it is already being used to treat a variety of different knee injuries. PRP is thought to contain concentrated growth factors and other growth-promoting cytokines. It is produced by centrifuging whole blood to remove the red blood cells with the remaining PRP injected into the injury site in a series of injections. The concentrated growth factors are supposed to promote better and faster healing.