Continuing Education Activity
The lower extremity is innervated by the lumbosacral plexus, comprising the L1 to S4 nerve roots. Unlike the brachial plexus, the lumbosacral plexus is not easily blocked with a single-injection technique. As technological advancements have increased the number of outpatient procedures, previously-used neuraxial techniques have become less desirable. Simultaneously, ultrasound-guided techniques have improved the identification of individual nerves and the accuracy of lower extremity nerve blocks. Although two or more separate injections are usually required for a complete lower extremity block, this is often the best option for outpatients. Lower extremity nerve blocks have gained popularity and are widely used in situations requiring lower-extremity anesthesia or analgesia. This activity reviews the role of lower extremity nerve block in providing anesthesia and analgesia to the lower extremity and highlights the role of the interprofessional team in providing care to patients undergoing these procedures.
Objectives:
- Correlate the innervation of the lower extremity with the clinical application of lower extremity nerve blocks.
- Enumerate the steps in the administration of lower extremity nerve blocks.
- Delineate the potential complications of lower extremity nerve blocks.
- Outline the importance of improving care coordination among interprofessional team members to improve outcomes for patients undergoing lower extremity nerve blocks.
Introduction
The lower extremity is innervated by the lumbosacral plexus, comprising the L1 to S4 nerve roots. Unlike the brachial plexus, the lumbosacral plexus is not easily blocked with a single-injection technique. Consequently, neuraxial blocks were preferred in the past when lower extremity anesthesia or analgesia was desired.
As technological advancements have increased the number of outpatient procedures, neuraxial techniques have become less desirable.[1][2][3][4] Simultaneously, ultrasound-guided techniques have improved the identification of individual nerves and the accuracy of lower extremity nerve blocks. Although two or more separate injections are usually required for a complete lower extremity block, this is often the best option for outpatients. Lower extremity nerve blocks have gained popularity and are widely used in situations requiring lower-extremity anesthesia or analgesia.
Anatomy and Physiology
The lumbosacral plexus divides into the femoral, lateral femoral cutaneous, obturator, and sciatic nerves that innervate the entire lower extremity.
The femoral nerve provides sensation and motor function to the anterior thigh. It continues as the saphenous nerve, providing sensation to the ipsilateral medial leg and foot and a portion of the ipsilateral great toe.
The lateral femoral cutaneous nerve supplies sensation to the lateral thigh. The sensory component of the obturator nerve supplies the medial thigh; the motor component supplies the thigh adductors. Neither the lateral femoral cutaneous nor the obturator nerve have any sensory or motor input to the leg distal to the knee.
The sciatic nerve runs with the posterior cutaneous nerve of the thigh and provides sensory and motor innervation to the posterior thigh. The sciatic nerve continues posteriorly and divides into the tibial and common peroneal nerves, just cephalad to the popliteal fossa, and provides sensory and motor innervation to the anterior, lateral, and posterior lower leg.
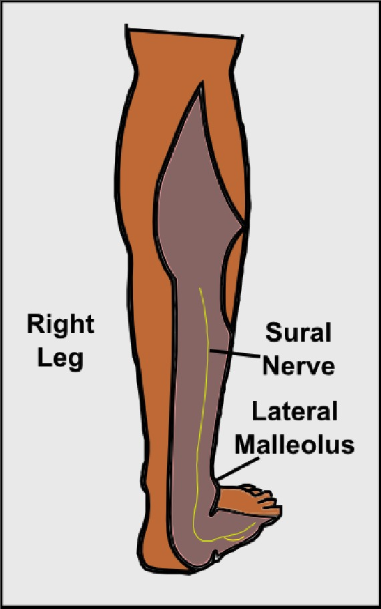
Five nerves provide sensory and motor to the foot. The saphenous nerve supplies sensation to the medial foot and a portion of the great toe. The deep peroneal nerve supplies the web space between the great toe and the second toe. The superficial peroneal nerve supplies the majority of the dorsum of the foot and toes, while the sural nerve supplies the lateral foot and a portion of the fifth toe. The posterior tibial nerve divides into the medial and lateral plantar nerves and supplies the sole and plantar surface of the toes.
Indications
Lower extremity blocks are useful in providing targeted anesthesia to the hip, knee, ankle, or foot, particularly in patients for whom general or neuraxial anesthesia is contraindicated. Furthermore, lower extremity blocks are frequently utilized postoperatively to improve pain control and lower the acute postoperative opioid burden.
Another benefit of lower extremity nerve blocks is the added effect of restoring mobility to patients who may otherwise be limited by pain in the early postoperative period. This early mobilization is important in minimizing complications such as venous thromboembolism and bedsores and promotes early progress in physical therapy.[5][6]
Contraindications
Complications of lower extremity nerve blocks are few.[7][8] Lower extremity nerve blocks should not be performed under the following conditions:
- Hypercoagulable state - lower extremity nerve blocks may blind practitioners to the early signs and symptoms of a deep venous thrombosis in patients at high risk for venous thromboembolism.
- Thrombocytopenia or anticoagulation may predispose to bleeding at the injection site and subsequent complications.
- Preexisting skin infections at the injection site frequently result in seeding the lower extremity or nerve, predisposing to deep infection.
- Patients with a demonstrated drug allergy to the anesthetic agent of choice should not undergo a lower extremity block due to the risk of anaphylaxis or other allergic response.
Equipment
The equipment used in lower extremity nerve blocks includes:
- Povidone iodine solution or chlorhexidine
- Sterile towels and gauze
- Sterile gloves
- Sterile gown for catheter placement only
- Pre-injection aspiration control syringe
- Needles: 18 or 20 G for drawing up the local anesthetic; 25 G for injection
- Local anesthetic with epinephrine or other additives such as dexamethasone or dexmedetomidine
Personnel
A lower extremity nerve block is a minor procedure with the potential to cause significant complications. Thus, the procedure should be performed in a designated area with standard American Society of Anesthesiologists monitors, intravenous access, and resuscitation drugs and equipment immediately available, including intralipid.
Technique or Treatment
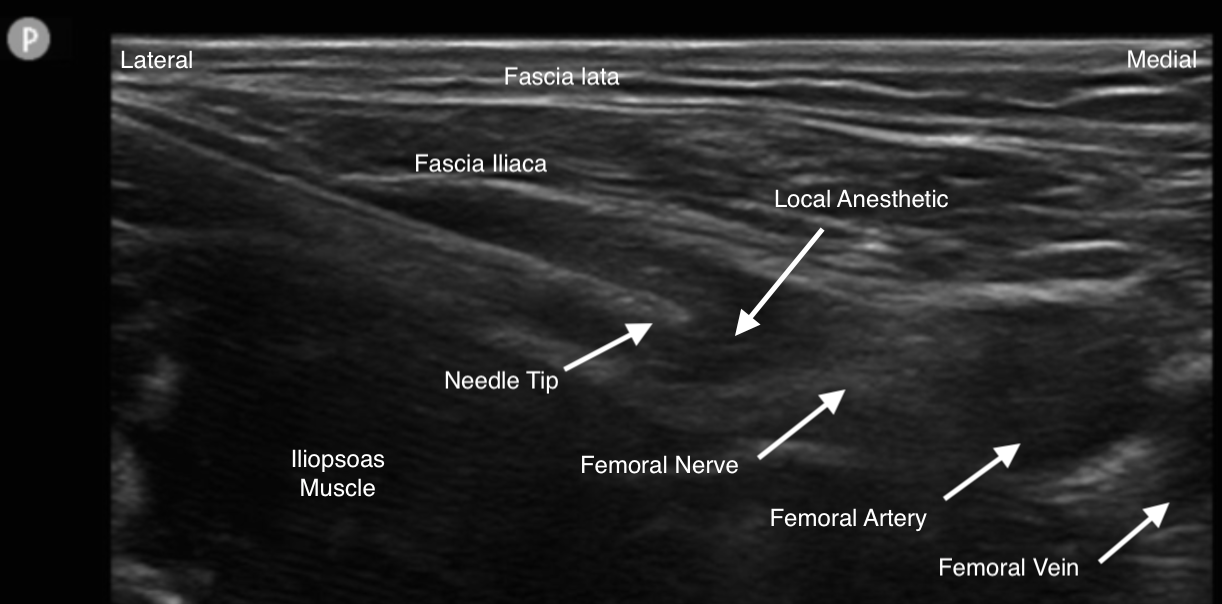
The femoral nerve can be blocked either deep to the fascia iliaca compartment caudad and medial to the anterior superior iliac spine or at the femoral crease. The fascia iliaca is a continuous band of fascia in this region, so local anesthetic injected under this fascia reliably produces a block of the femoral and lateral femoral cutaneous nerves. Anatomic, stimulator, and ultrasound-guided techniques have been described. The obturator nerve is less reliably blocked the more caudad the block is performed.
The saphenous nerve can be blocked at the mid-shaft femur in the adductor canal or with a field block at the tibial plateau. Saphenous nerve blocks have gained popularity because while sensation is blocked, motor function is spared, an ideal situation for physical therapy and rehabilitation.
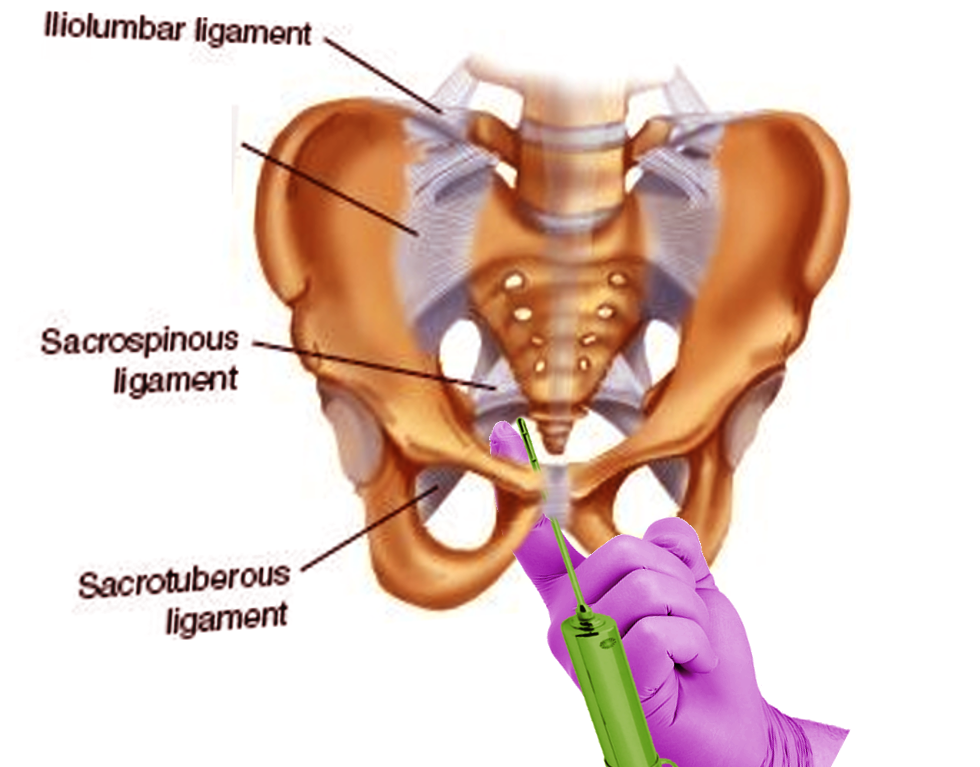
A sciatic nerve block can be achieved via multiple approaches. In the classical approach, the sciatic nerve is blocked in the gluteal region between the greater trochanter and ischial tuberosity, deep to the gluteus muscles and superficial to the quadratus femoris. The anterior sciatic approach blocks the nerve as it travels through the thigh adductors. Finally, in a popliteal block, the injection is administered approximately 6 cm above the popliteal fossa before the sciatic nerve divides into the tibial and common peroneal nerves. Anatomic and ultrasound-guided approaches have been described for the blockade of the sciatic nerve at these three main locations.
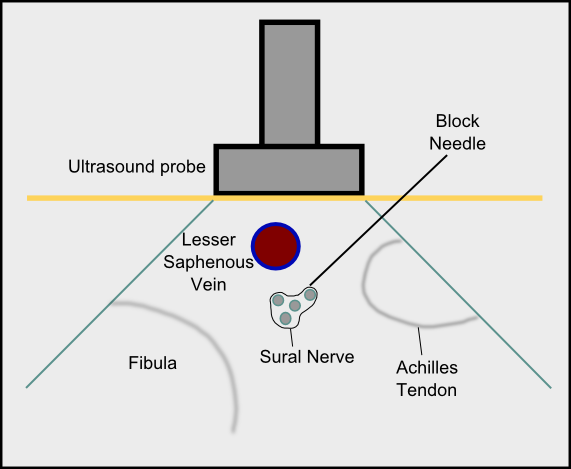
A complete block of the foot can be accomplished with five injections at the ankle. The saphenous nerve is blocked anterior to the medial malleolus. The deep peroneal nerve is blocked at the anterior ankle between the extensor hallucis longus and extensor digitorum longus. The superficial peroneal nerve is blocked anterior to the lateral malleolus. The sural nerve is blocked between the lateral malleolus and the Achilles tendon. Finally, the posterior tibial nerve is blocked posterior to the medial malleolus.
Complications
Local Complications from the Injection
- Hematoma
- Infection
- Injury to the nerve
- Anesthetic blockade of adjacent structures
- Block failure
Systemic Toxicity
- Dizziness, lightheadedness
- Blurred vision
- Ringing, buzzing in ears
- Metal taste in the mouth
- Numbness/tingling around mouth, fingers or toes
- Drowsiness or confusion
- Seizures and cardiac arrest
Clinical Significance
The femoral nerve block affects both motor and sensory nerves. This block can be used for procedures on the knee or to repair trauma to the medial aspect of the thigh and lower leg. After the procedure, the patient will have marked weakness in the quadriceps and should not be allowed to ambulate until all sensation has returned.
The adductor canal block is similar to the femoral nerve block but only affects the sensory nerves of the lower leg. Therefore, it can also be used for procedures on the knee and medial aspect of the lower leg.
The popliteal block at the knee is often used for surgery on the lower leg.
The fascia iliaca compartment block can block the femoral, obturator, and lateral femoral cutaneous nerves and is often used for hip fractures and total hip arthroplasties. The block provides prolonged pain relief in the hip and anteromedial thigh.
If successful, most lower extremity nerve blocks last 6 to 24 hours; the duration of anesthesia or analgesia may be shorter. Other options for lower extremity anesthesia and analgesia include spinal and epidural anesthesia.
Enhancing Healthcare Team Outcomes
Anesthesiologists usually perform lower extremity nerve blocks, but a nurse must be dedicated to patient monitoring. Resuscitative equipment must be in the room where the procedure is being done. Complications, though rare, can potentially cause cardiac or respiratory arrest, bleeding, and nerve damage.[9] An interprofessional team approach will provide the safest and best results for the patient. [Level V]
Skills
Knowing how to manage anesthesia in patients with lower extremity blocks is essential. Recognition, treatment, and prevention of perioperative adverse events associated with lower extremity blocks is an important strategy. Therefore, management of lower extremity nerve blocks crosses over the breadth and depth of healthcare situations and settings in the perioperative environment.
Strategy
It is most appropriate and ideal to maintain continuous closed-loop communication between all members of the perioperative care team regarding the need, technique, and potential management issues associated with lower extremity blocks. Collaboration, interdisciplinary interprofessional teamwork, and a culture of integrity and quality improvement are essential to a successful strategy.
Ethics
It is necessary to obtain thorough and comprehensive informed consent from either the patient or, in the case of patients without the capacity to consent, their designated and authorized decision-maker before administering a lower extremity nerve block. All team members should feel empowered to state any concerns regarding the process, as this provides additional layers of review and insight into any problematic matters as soon as possible.
Responsibilities
All team members must communicate their concerns, responsibilities, and activities with all other team members contemporaneously and as indicated throughout the perioperative period, based on their professional discretion. All team members are responsible for maintaining professional interactions with, respecting different opinions, and engaging in shared-decisionmaking with all involved stakeholders.
Interprofessional Communication
All team members should respect the free flow of information and concerns among team members without allowing or producing an environment of hostility. Monitoring must be diligent and consistent between and among team members. Maintain clear and closed-loop professional communication between interdisciplinary team members and among all team members.
Care Coordination
All interprofessional team members should consider it their duty to neither disrupt the work done by other team members nor to, through their actions or inaction, create additional issues or increase the workload for other team members. [Level 5]