Continuing Education Activity
Sinus arrhythmia is a variation of normal sinus rhythm that characteristically presents with an irregular rate in which the change in the R-R interval is greater than 0.12 seconds. Additionally, the P waves are typically monoform and in a pattern consistent with atrial activation originating from the sinus node. During respiration, intermittent vagus nerve activation occurs, which results in beat-to-beat variations in the resting heart rate. When present, sinus arrhythmia typically indicates good cardiovascular health. This activity illustrates the diagnosis of sinus arrhythmia on telemetry and reviews the role of the interprofessional team in managing patients with this condition.
Objectives:
- Describe the features of sinus arrhythmia.
- Articulate the pathophysiology of sinus arrhythmia.
- Outline the health expected in a patient with sinus arrhythmia.
- Explain the importance of cooperation among the interprofessional team members in the identification of this rhythm and counseling patients that this sinus arrhythmia is normal and serves as an indicator of cardiac health.
Introduction
Sinus arrhythmia is a commonly encountered variation of normal sinus rhythm. Sinus arrhythmia characteristically presents with an irregular rate in which the variation in the R-R interval is greater than 0.12 seconds. Additionally, P waves are typically monoform and in a pattern consistent with atrial activation originating from the sinus node. During respiration, intermittent vagus nerve activation occurs, which results in beat-to-beat variations in the resting heart rate. When present, sinus arrhythmia typically indicates good cardiovascular health.
Etiology
Sinus arrhythmia is a common rhythm variation. It is seen more often in children and young adults. Respirations lead to vagal stimuli resulting in R-R interval variations. Typically its presence is an indicator of good cardiovascular health. Loss of sinus arrhythmia may indicate underlying heart failure or structural heart disease.
Epidemiology
Sinus arrhythmia is most typically present in young, healthy individuals. Studies have attempted to establish an increased prevalence in patients with underlying hypertension, obesity, and diabetes. A published study from 2002 in the Journal of the American College of Cardiology suggested that sinus arrhythmia appeared to be less prominent in older individuals. The study evaluated two groups of healthy individuals without underlying cardiovascular disease. The first group evaluated patients between the ages of 50 and 71 years of age, and the second, patients under the age of 31. Investigators found that the prevalence of respiratory sinus arrhythmia in older individuals was less than 20 percent of that in those less than 31 years of age. Some suspect that this is due to age-related changes in the compliance of arterial walls and diminished vagal responses.[1]
Pathophysiology
Investigation on the pathogenesis of sinus arrhythmia continues but three main theorized mechanisms exist at this time. These include respiratory-phasic, nonrespiratory-nonphasic, and nonrespiratory-ventriculophasic sinus arrhythmia.
Respiratory-Phasic
Respiratory sinus arrhythmia is a common finding. It is a normal alteration in cardiac rhythm generated from the stimulation of the vagus nerve and changes in cardiac filling pressures during respiration. Recently, there has been controversy regarding the underlying pathogenesis of sinus arrhythmia. Some studies have begun to associate sinus rhythm with obesity, diabetes mellitus, and hypertension, while others continue to support a reduction in sinus arrhythmia when these conditions are present. Some studies suggest there may be some relationship between heart failure and other systemic conditions.
One study attempted to evaluate the influences of vagal and sympathetic efferent activity on sinus arrhythmia through the administration of hyoscine butylbromide and atenolol. Administration of hyoscine butylbromide resulted in the reduction of sinus arrhythmia, while atenolol reduced vagal tone, prolonging the mean R-R and increasing sinus arrhythmia. The study suggested that mediation of sinus arrhythmia occurs through vagal stimulation.[2] During the respiratory cycle, inspiration inhibits vagal tone leading to an increase in sinus rate, while expiration increases vagal tone resulting in a decreased rate. This concept was supported by a later study that successfully mimicked the respiratory cycle via stimulation of baroreceptors in the carotid artery with cycles of phased neck suction at the frequency of normal respiration. The study suggested that baroreceptor signaling plays an important role in the generation of respiratory sinus arrhythmia.[3] More recently, investigators have evaluated the effects of diabetes mellitus on sinus arrhythmia. They found that in patients with diabetes, there is a reduction in sinus arrhythmia, which investigators attributed to the autonomic effects of the disease.[4]
Nonrespiratory
In nonrespiratory sinus arrhythmia, electrocardiograms will appear similar to the respiratory type. The two differ in that nonrespiratory sinus arrhythmia is not associated with the respiratory cycle. While it can occur within healthy individuals, more often, this type correlates with underlying pathology.[5] Some have reported this finding with underlying heart disease or associated with digitalis overdose. One case report associated the finding with a traumatic intracerebral hemorrhage, which authors associated with vasospasm, hypoxia, or increased intracranial pressure.[6]
Ventriculophasic
The ventriculophasic sinus arrhythmia, when present, typically occurs in patients with third-degree AV block. However, they demonstrate correlations between premature ventricular contractions. Currently theorized mechanisms suggest that ventriculophasic sinus arrhythmia results due to a prolonged cardiac filling resulting in increased stroke volume. The increased stroke volume triggers a carotid baroreceptor response. On EKG, this is represented by an interval shortening between the QRS and subsequent P wave.
History and Physical
Sinus arrhythmia is a common incidental finding seen on presenting EKGs. The finding is normal and found at a higher prevalence in younger individuals. Lack of sinus arrhythmia may be a sign of underlying chronic disease requiring further investigation. It is rare for patients with sinus arrhythmia to display symptoms. If present, symptoms such as shortness of breath, lower extremity edema, dyspnea on exertion, or peripheral neuropathy are likely due to some underlying cause and not sinus arrhythmia. Care should be taken to rule out other potential causes of sinus arrhythmia while taking history. History of trauma to the head or neck via fall or another mechanism, especially in the setting of anticoagulation use, may increase suspicion for underlying intracranial hemorrhage. Additionally, care should be taken on a review of the initial EKG to rule out 3rd-degree heart block as a cause of sinus arrhythmia. No physical exam findings directly correlate to the diagnosis of sinus arrhythmia.
Evaluation
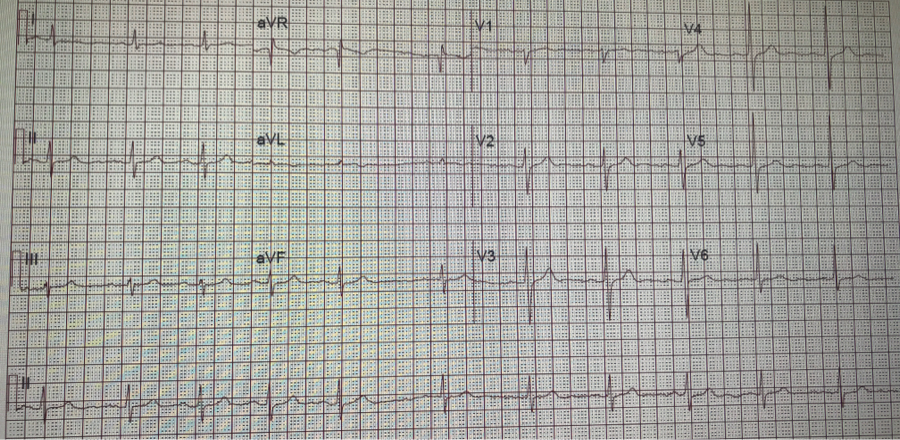
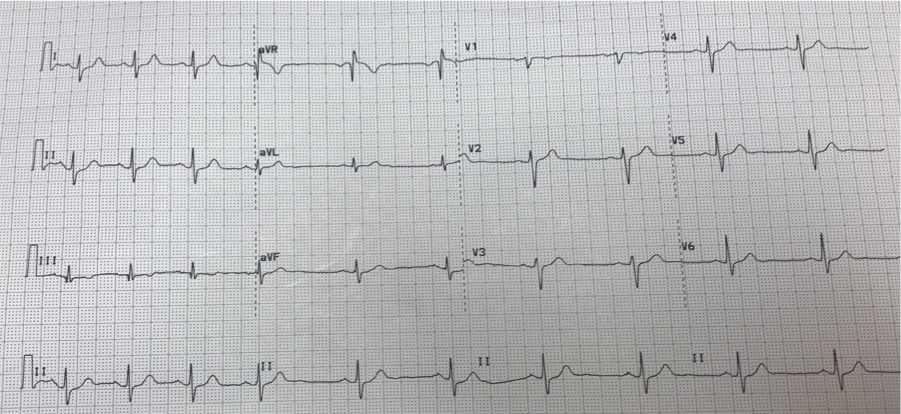
Often an asymptomatic and normal finding, the evaluation of sinus arrhythmia is limited. Care should be taken to rule out other causes of arrhythmia, including atrial fibrillation, flutter, or multifocal atrial tachycardia with an EKG. P-waves will show uniform morphology. On the EKG, sinus rhythm appears as a beat-to-beat variation in the P-P interval. Typically, this variation is greater than 120 msec: the P-P interval increases and decreases with inspiration and exhalation.
Treatment / Management
Sinus arrhythmia is a common finding on telemetry. It is considered to be a normal variation found in healthy young adults. Upon confirming the diagnosis of sinus arrhythmia on EKG, there are no further recommendations regarding treatment.
Differential Diagnosis
Atrial fibrillation
Third-degree AV block
Sick sinus syndrome
Sinoatrial exit block
Staging
No required staging criteria exist for the evaluation of sinus arrhythmia.
Prognosis
Sinus arrhythmia typically presents as an indicator of cardiovascular health, most often found in young, healthy patients. Sinus arrhythmia does not correlate with a decrease in life expectancy or other comorbidities. Its absence, however, has been associated with chronic diseases such as diabetes mellitus and heart failure.
Complications
Typically an incidental finding, there are rarely any complications associated with sinus arrhythmia.
Consultations
Cardiology consults are not a requirement for patients with sinus arrhythmia.
Deterrence and Patient Education
Patients found to have sinus arrhythmia should receive education that this is a common finding seen in young, healthy persons. It rarely requires further evaluation upon establishment of the diagnosis.
Pearls and Other Issues
Sinus arrhythmia is a common incidental finding on routine EKG. It is most prevalent in young, healthy patients and is a prognostic indicator of good cardiac health. It decreases in prevalence in older patients and those with multiple comorbid conditions, including diabetes and heart failure. Typically asymptomatic, patients rarely require evaluation by a cardiologist or additional treatment.
Enhancing Healthcare Team Outcomes
Sinus arrhythmia is a common incidental finding that often prompts evaluation by a cardiologist. This is likely due to low levels of provider confidence and education regarding this rhythm. Often found in young, healthy persons, sinus arrhythmia typically does not require further evaluation. There are no indications at this time for medications for the treatment of sinus arrhythmia. Nursing staff may play an essential role in the evaluation of sinus arrhythmia, as they are often the first health professional to detect its presence on telemetry. Comfort with the identification of this rhythm is pivotal to decreasing healthcare costs and eliminating potential exposures of patients to anticoagulants. Patients should receive counsel that this finding is normal and serves as an indicator of cardiac health. Level of Evidence - II