Continuing Education Activity
When tachycardic rhythms fail to respond to pharmacologic treatment or present with or deteriorate into unstable manifestations, synchronized cardioversion is the treatment of choice. This activity reviews the guidelines for the provision of emergency synchronized cardioversion to victims of sudden cardiac arrest.
Objectives:
Evaluate the approach to the management of tachycardic rhythms.
Identify the difference between defibrillation and synchronized cardioversion.
Evaluate the technique of synchronized cardioversion in treating unstable tachycardic rhythms.
Explain the importance of improving care coordination among the interprofessional team in performing synchronized electrical cardioversion.
Introduction
Synchronized cardioversion is a procedure similar to electrical defibrillation in that a transthoracic electrical current is applied to the anterior chest to terminate a life-threatening or unstable tachycardic arrhythmia. Unlike defibrillation, which is used in cardiac arrest patients, synchronized cardioversion is performed on patients who still have a pulse but are hemodynamically unstable. It is used to treat both hemodynamically unstable ventricular and supraventricular rhythms.
Each year, almost 350,000 Americans die from heart disease. Half of these die suddenly, outside of a hospital, because of the sudden cessation of spontaneous, organized cardiac function. The most common cause of sudden cardiac arrest in adults is pulseless ventricular tachycardia or ventricular fibrillation. Ventricular tachycardia can also occur in the presence of a pulse; often, it is the precursor to ventricular fibrillation. Ventricular tachycardia is characterized by rapid, wide (greater than 0.12 seconds) QRS complexes.
Supraventricular Tachycardia (SVT) refers to a cardiac rhythm greater than 100 beats per minute, which originates above the bundle of His. SVT is characterized by rapid, narrow (less than 0.12 seconds wide) QRS complexes. Any tachycardic rhythm that does not originate in the ventricles is called SVT. This includes sinus tachycardia, junctional tachycardia, reentrant tachycardias, multiple atrial tachycardia (MAT), atrial fibrillation, and atrial flutter. Although various supraventricular rhythms can cause SVT, they are treated with the same clinical approach.[1]
Indications
VT can be caused by coronary artery disease, hypertension, valvular heart disease, and cardiomyopathy. It can also be induced by a blow to the chest (commotio cordis).[2] SVT is usually caused by the repetitive “re-entry“ of the electrical impulse proximally instead of propagating distally through the cardiac conduction system due to blockages in the heart’s electrical conduction system. It can also result from premature atrial or ventricular beats, cardiac stimulants, thyroid conditions, valvular and coronary artery disease, and digoxin toxicity.
Contraindications
There are no contraindications to synchronized cardioversion. The presence of a pacemaker or automated implanted cardiac defibrillator does not change the procedure's indication or performance.
Equipment
A monitor and defibrillator with synchronized function.
Technique or Treatment
Under the American Heart Association's advanced cardiovascular life support (ACLS) guidelines, the identification and treatment strategies for all tachycardic rhythms involve 3 simple, rapid decision points.[3] First is the identification of the rhythm as tachycardia. Next, the tachycardic rhythm is divided into 1 of 2 categories depending on the width of the QRS complex:
- Wide-complex tachycardia (QRS width greater than 0.12 seconds)
- Narrow-complex tachycardia (QRS width less than 0.12 seconds)
All narrow-complex tachycardias are considered supraventricular and are referred to as SVTs. Although wide-complex tachycardic rhythms can occur from sites above the ventricles (such as in supraventricular rhythms with a bundle branch block or other aberrant conduction), clinically, especially during emergent situations, wide-complex tachycardia is usually treated as ventricular in origin, as it is the most potentially life-threatening condition.
The treatment of all emergent tachycardic rhythms, whether narrow-complex or wide-complex, depends on the third and final clinical determination: the presence or absence of a pulse. Pulseless rhythms are treated under the ACLS cardiac arrest algorithms: a wide-complex tachycardia would be considered pulseless ventricular tachycardia, which is treated the same as ventricular fibrillation under the ventricular fibrillation algorithm. A narrow-complex tachycardia would be considered a pulseless SVT and treated under the pulseless electrical activity (PEA) algorithm.
In the presence of a pulse, the specific treatment for all tachycardic rhythms depends on 1 final determination: whether the pulse generated allows the patient to be considered stable or unstable. In stable patients, the treatment for the underlying arrhythmia is usually medication.[4] For unstable patients, the treatment of choice is electricity. All tachycardic rhythms, whether wide or narrow complex, are considered to be unstable if the patient also has chest pain, dyspnea, altered mental status, hypotension, pulmonary edema, or ischemic changes on the EKG. The treatment for all unstable tachycardic rhythms is synchronized cardioversion.
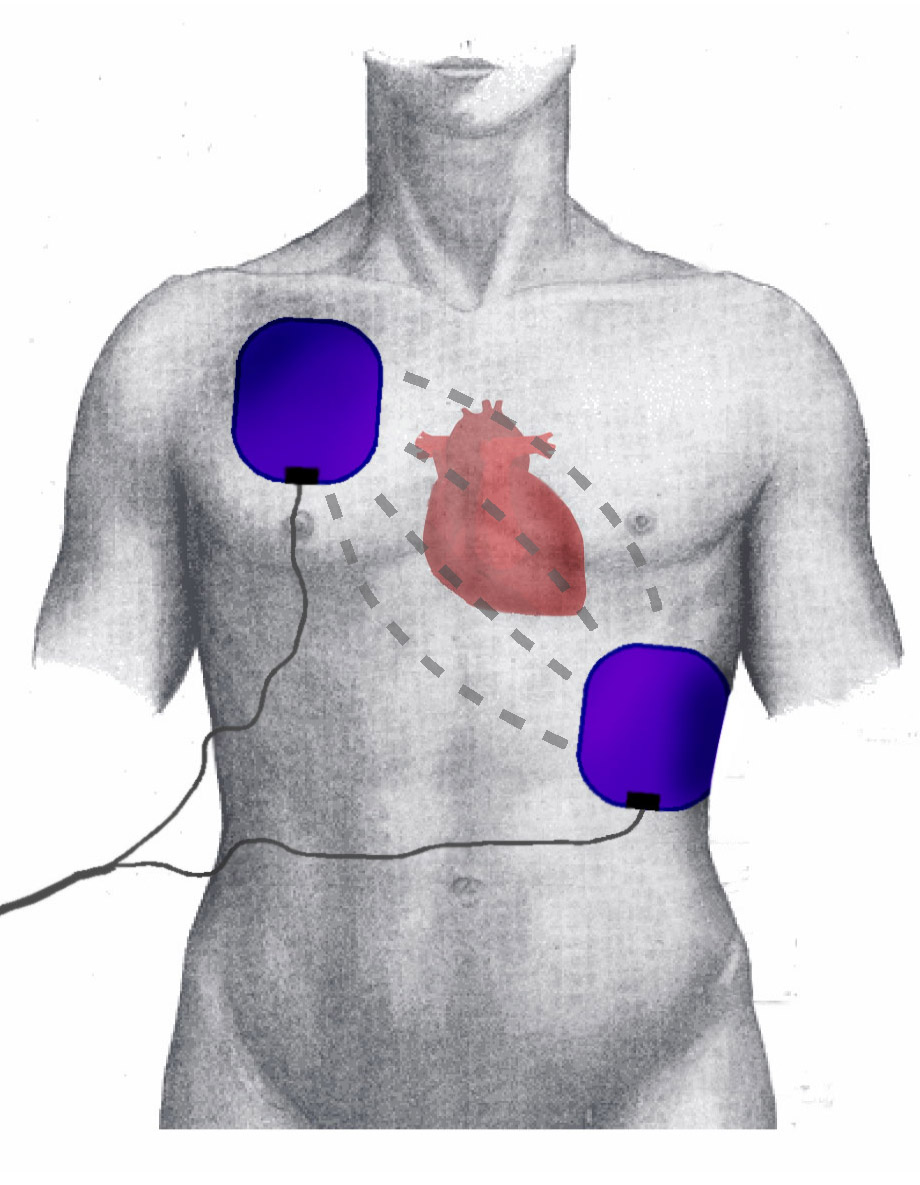
Like defibrillation, synchronized cardioversion delivers a shock across the chest by placing a pair of manual paddles on the chest or applying adhesive “hands-free” pads.[5] Most current defibrillators utilize a biphasic waveform that allows for a lower energy level to achieve effective cardioversion. Because of their greater ability to terminate ventricular dysrhythmias, defibrillators utilizing biphasic waveforms are preferred to those utilizing the older monophasic waveform. See Image. Electrode Positions During Defibrillation/Cardioversion.
Synchronized cardioversion differs from defibrillation in 2 aspects: the amount of energy needed to convert the rhythm is usually less than that required, and the shock is delivered in a different part of the cardiac cycle. When a patient is defibrillated, the energy is released through the paddles or hands-free pads immediately when the defibrillation button/s are pressed. The shock is delivered at whatever point the cardiac cycle happens to be in. If an electrical shock is provided during the relative refractory period (corresponding to the latter part of the T wave), it is possible to induce ventricular fibrillation (the so-called “R-on-T Phenomenon”). This would result in a patient who originally had a pulse being put into cardiac arrest.
To avoid inducing cardiac arrest in a patient with a pulse, synchronized cardioversion is performed instead of defibrillation when a patient is in an SVT with a pulse but is considered unstable according to the definition above. To perform synchronized cardioversion, the defibrillator is placed into the “synchronize” mode by pressing the appropriate button on the machine. This causes the monitor to track the R wave of each QRS complex that goes by. A synchronizing marker appears above each QRS complex, indicating the synchronize feature is active.
The appropriate energy level is selected, and the discharge/shock button is pressed and held. The defibrillator does not release the shock immediately. Instead, it waits for the next R-wave to appear and delivers the shock at the time of the R-wave. This allows the shock to be provided safely away from the T wave, avoiding the R-on-T phenomenon. The recommended energy levels for synchronized cardioversion vary from 50 to 200 joules. Recalling the specific energy level for a particular sub-type of unstable tachycardia is difficult, especially in an emergent situation. The safest and easiest recommendation is to start at the lowest energy level (50 joules), and if the shock is unsuccessful, double the amount of energy used. In a refractory case, 200 joules could be used after just 3 shocks.
Complications
Complications of synchronized electrical cardioversion include:
- If a patient with unstable SVT were to lose his or her pulse at any point, treatment would default to the ACLS algorithm for PEA.
- If a patient with unstable ventricular tachycardia with a pulse were to lose his or her pulse at any point, treatment would default to the ACLS algorithm for ventricular fibrillation.[6]
- If a patient develops ventricular fibrillation, the monitor/defibrillator needs to be taken out of the "synchronize" mode, as defibrillation is not possible while the machine is searching for a QRS complex.[7][8][9]
Clinical Significance
Appropriate synchronized electrical cardioversion restores the activity of the heart's electrical conduction system and is the most effective resuscitation measure for many arrhythmias.
Enhancing Healthcare Team Outcomes
Cardioversion is performed both inside and outside the hospital, and it is one technique that all healthcare professionals, including nurses, pharmacists, and EMS, should be familiar with. It has been shown to save lives, so it is important to know how the device works and its indications. To ensure proficiency with cardioversion, regular updating of ATLS protocols is necessary. Education by an interprofessional team of specialty-trained nurses and clinicians provides the best results.