Continuing Education Activity
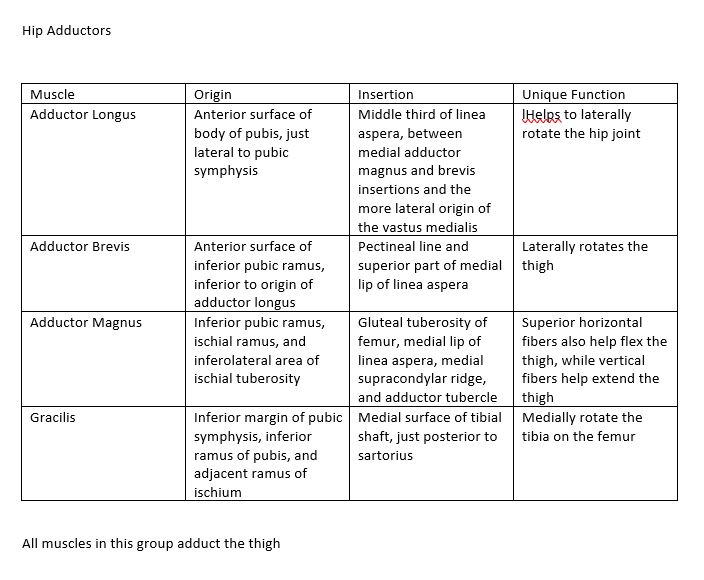
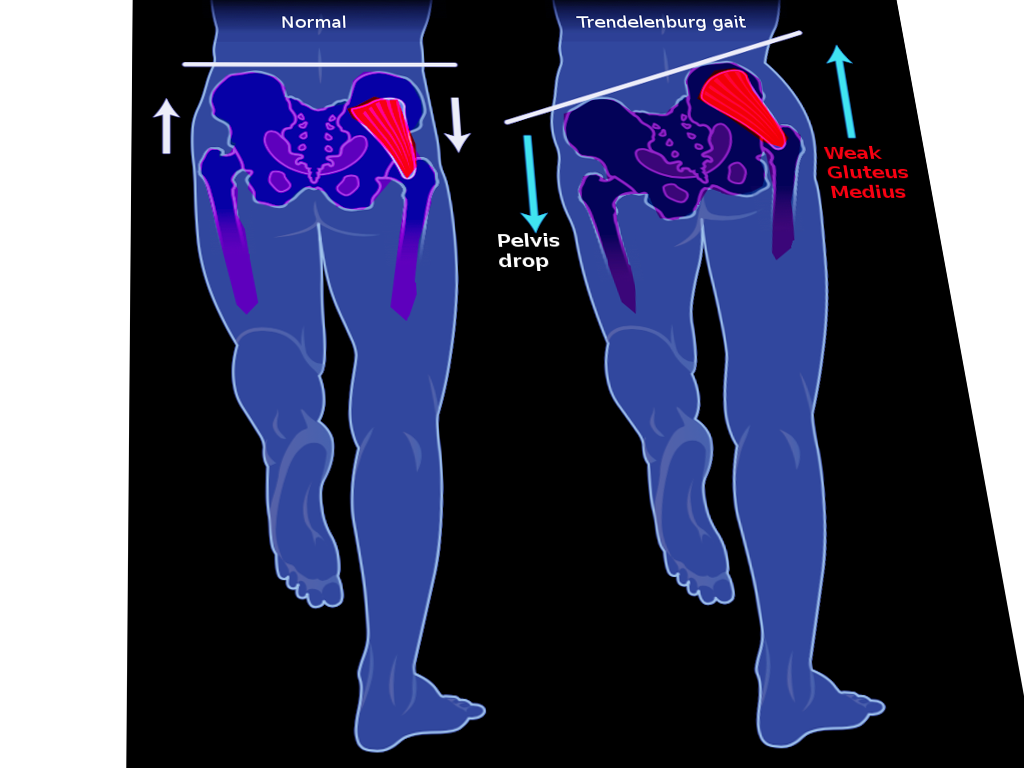
A trendelenburg gait is an abnormal gait resulting from a defective hip abductor mechanism. The primary musculature involved is the gluteal musculature, including the gluteus medius and gluteus minimus muscles. The weakness of these muscles causes drooping of the pelvis to the contralateral side while walking. This activity reviews the evaluation and management of trendenlenburg gait and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance patient outcomes.
Objectives:
- Describe the pathophysiology of the trendenlenburg gait.
- Identify conditions that may lead to a trendenlenburg gait.
- Explain management strategies for a trendenlenburg gait.
- Outline the importance of enhancing care coordination among the interprofessional team to ensure proper evaluation and management of trendenlenburg gait.
Introduction
Trendelenburg gait is an abnormal gait resulting from a defective hip abductor mechanism. The primary musculature involved is the gluteal musculature, including the gluteus medius and gluteus minimus muscles. The weakness of these muscles causes drooping of the pelvis to the contralateral side while walking. The gait gets its name from a German surgeon, Friedrich Trendelenburg, who first reported the test related to this gait in 1895. The physical examination test described by him is useful to uncover hip abductor weakness in a patient with developmental dysplasia of the hip.[1]
Etiology
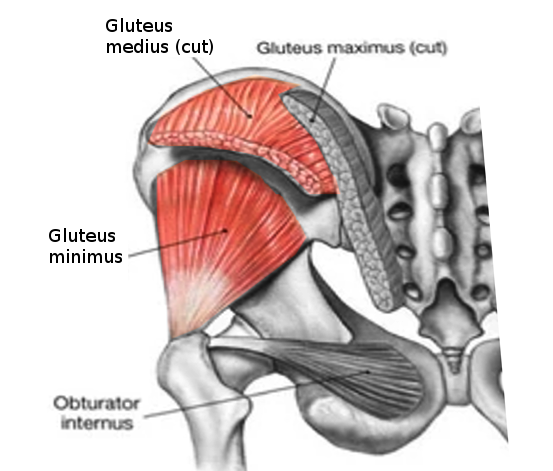
The hip joint and its abductor mechanism behave like a class 1 lever with the effort and the load on either side of the fulcrum.[2]
Any pathology of the fulcrum, load, effort, or the lever which binds all three will lead to a positive Trendelenburg gait.
Failure of the fulcrum presents in the following conditions:
-
Osteonecrosis of hip
-
Legg-Calve-Perthes disease
-
Developmental dysplasia of the hip
-
Chronically dislocated hips secondary to trauma
-
Chronically dislocated hips secondary to infections like tuberculosis of the hip
Failure of the lever is a feature in the following conditions:
Failure of effort presents in the following conditions:
- Poliomyelitis
-
L5 radiculopathy
-
Superior gluteal nerve damage
-
Gluteus medius and minimus tendinitis
-
Gluteus medius and minimus abscess
-
Post total hip arthroplasty
Epidemiology
Trendelenburg gait is a common problem in a patient that has paralysis/paresis of the hip abductors.
Pathophysiology
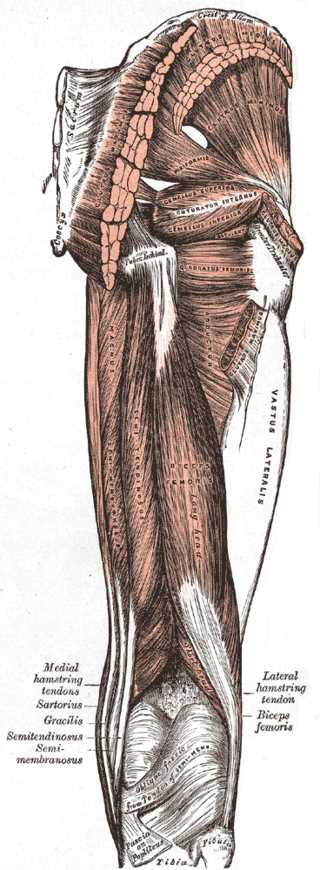
The center of gravity of the body passes midway through the pubic symphysis. When one foot lifts off the ground, as during swing phase of the gait cycle, the body remains unsupported on that side, and the pelvis tends to drop to the unsupported side. To prevent the drop, the abductor muscles mainly the gluteus medius and minimus on the supported side contract, providing stabilization of the superimposed trunk.[3] If there is any damage to the hip and its abductor mechanism due to the causes mentioned above, there will be drooping of the pelvis on the opposite side of the pathology.
History and Physical
A patient with a Trendelenburg gait often complains of a limp. The limp can be painful or painless depending on the etiology. If the limp is severe, there is compensatory bending or lurching to the side of pathology to balance the center of gravity of the body. This limp is called the lurching gait. When the pathology is bilateral, the pelvis droops to the unsupported side alternating with each step and is called a waddling type of gait. This gait, when present, provides clues regarding certain possible etiologies, such as non-union of the neck of femur and developmental dysplasia of the hip.
On physical examination of gait, the lurching or waddling type of gait patterns should alert the physician to examine the abductor mechanism of the hip more closely.
Mild Trendelenburg gait may be difficult to appreciate while examining the patient with full clothing. It is necessary to perform a Trendelenburg test to evaluate further.
To perform the test, the examiner sits or stands behind the patient. The patient is then asked to lift each foot off the ground, and the opposite side pelvis is elevated as high as possible alternately for at least 30 seconds. [4] This modification was suggested by Hardcastle et al. and is now practiced worldwide as a standard practice. In healthy individuals, the unsupported side stays at the same level or rises slightly. When the abductor mechanism is weak, the pelvis drops towards the unsupported side. In case of more serious weakness, the patient leans towards the affected side. This dropping of the pelvis in the standing position suggests a positive Trendelenburg test.
The prerequisites for doing the test are as follows:
-
The patient should have a painless hip pathology. In case of a painful hip condition, the patient will not be able to balance leading to spurious results.
-
The must not have abduction or adduction (coronal plane) deformities of the hip. Presence of adductor deformity at the hip leads to elevation of the pelvis leading to the false negative result. Presence of abductor deformity at the hip leads to drooping of the pelvis on the contralateral side leading to the false positive result.
Limitations of the Trendelenburg test:
-
Kendall et al. have shown that hip abductor weakness induced by superior gluteal nerve block does not correlate with the pelvis drop mainly in athletes and in patients who are asymptomatic but have hip pathology.[5]
-
In a patient with early stages of osteonecrosis, in spite of having an abductor mechanism defect Trendelenburg sign and therefore gait remain masked.[6]
-
Pelvis drop can occur even in healthy individuals with normal abductor mechanism when the abductor muscle is not working adequately.
Evaluation
Detailed physical examination should be carried out to diagnose the condition leading to the abnormal gait. Other investigations include X-rays, ultrasonography, computed tomography (CT) scans and magnetic resonance imaging (MRI) to diagnose the primary condition. Blood tests may be performed to corroborate with the radiological findings.
Treatment / Management
The main focus of the treatment after identification of the etiology involves correction of the etiological factor resulting in the Trendelenburg gait and varies according to the pathology.
Trendelenburg gait by itself wears the hip joint, and appropriate treatment is essential.
Physical therapy is the mainstay treatment for gluteus medius and minimus weakness. Physical therapy involves strengthening the weakened hip abductor muscles. This involves lying on the unaffected side while abducting the affected leg up towards the ceiling. A theraband can be applied on the lower limb to increase the resistance during the exercise. Other modalities include lateral side steeping and balance exercises.
Patients who have abductor weakness after an arthroplasty require specific exercises which include:
-
Non-weight bearing standing abduction
-
Weight-bearing standing abduction
-
Side-lying abduction
-
Resisted side-stepping exercises
Weight-bearing exercises have been shown to have a better functional recovery than non-weight bearing exercises.
Alteration of the gait pattern after gait training can also compensate for the hip abductor weakness.[7]
For gluteus medius tears, reports have shown that in patients with hip abduction manual muscle strength less than 4/5 along with the presence of gait dysfunction, surgical intervention is likely indicated. [8]
Differential Diagnosis
Trendelenburg gait must be differentiated from other gait patterns including the following:
- Short limb gait
- Antalgic gait
- Extension lurch gait
- High stepping gait
- Stamping gait
A thorough history and physical examination are essential to rule out other types of abnormal gait patterns.
Prognosis
Trendelenburg gait can be treated efficiently irrespective of the etiology. Timely detection of altered gait, prompt diagnosis and effective treatment of the primary condition are essential for a good outcome.
Complications
Chronic untreated abnormal Trendelenburg gait may lead to the development of secondary pathology at the knees or ankles over the years. It is also known to accelerate the process of wear and tear at the hip joint. The wear and tear usually occur at the portions of the hip which are typically not used during normal gait, more so in athletes.[9][10] Untreated Trendelenburg gait can also lead to dynamic lower extremity valgus.[11] The mechanism behind this is that the pelvis of the unaffected side will be elevated thereby having the trunk lean towards the affected side. The ground resultant force will, in turn, be directed to the lateral knee joint thereby producing a valgus knee on the affected side. This over time can lead to knee pain.
Consultations
Depending on the etiology the following consultations are essential:
- Joint replacement orthopedic specialist
- Pediatric orthopedic specialist
- Occupational therapist
- Physical therapist
- Radiologist
Deterrence and Patient Education
Patients need to be aware of the Trendelenburg gait and other abnormal gait patterns and should seek medical treatment promptly which can prevent irreversible damage to the hip joint.
Pearls and Other Issues
- Pathology of Trendelenburg gait can be in the fulcrum, lever or the effort arm of the hip abductor mechanism.
- The Hardcastle modification of Trendelenburg eliminates false-positive results.
- Trendelenburg gait by itself causes wear and tear of the hip joint, so prompt diagnosis and treatment are essential.
Enhancing Healthcare Team Outcomes
A patient-centric an interprofessional approach is essential while managing a patient with Trendelenburg gait. This team includes the primary care physician, orthopedic specialists, nursing, and may also include physical therapists and/or a chiropractor, all working in an interprofessional team approach. Patients need to follow up with the therapist and orthopedic nurse for many months because recovery is gradual. For benign causes, full recovery is possible but if there is permanent nerve damage, a persistent limp may develop.