Introduction
The ulnar nerve is one of the 5 terminal branches of the brachial plexus, arising from the medial cord. It supplies motor and sensory innervation to the upper extremity. The ulnar nerve originates from contributions of the ventral rami of C8 and T1 nerve roots. The nerve courses along the medial arm and forearm, and then it passes into the wrist, hand, and fingers.[1][2][3]
Structure and Function
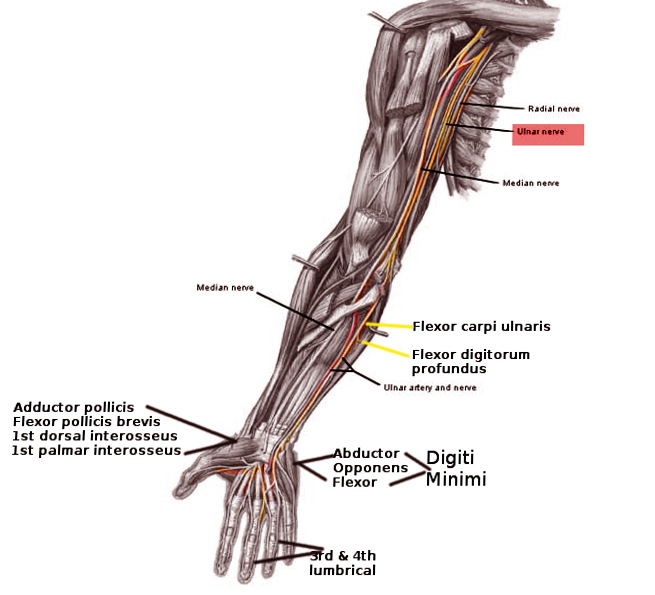
The ulnar nerve provides motor innervation to part of the forearm and majority of the hand. It supplies sensory cutaneous innervation to the medial forearm, medial wrist, and medial one and one-half digits. The ulnar nerve and its branches send motor innervation to the flexor carpi ulnaris and flexor digitorum profundus in the forearm, and hypothenar muscles (opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi brevis). In the hand, the ulnar nerve provides motor innervation to the third and fourth lumbricals, dorsal interossei, palmar interossei, adductor pollicis, flexor pollicis brevis and palmaris brevis.
Nerves
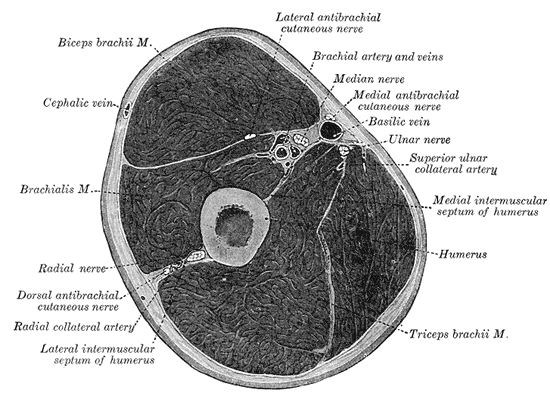
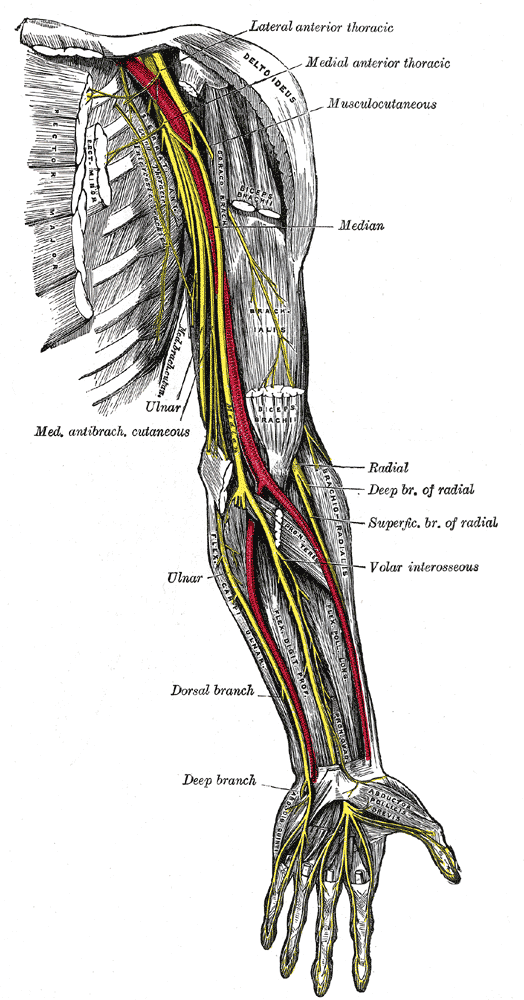
The ulnar nerve carries both sensory and motor fibers from the C8 and T1 dorsal rami. The nerve courses along the medial arm from the anterior to the posterior compartment, through the medial intermuscular septum, called the arcade of Struthers. The arcade is formed by the medial head of the biceps, medial intermuscular septum, and internal brachial ligament. It then passes posterior to the medial epicondyle of the humerus, giving off its first branch providing proprioception to the elbow joint. At the distal elbow, the ulnar nerve passes underneath Osbourne's ligament (retinaculum between the two heads of the flexor carpi ulnaris muscle). It continues through the flexor and pronator muscles of the forearm and into the wrist, superficial to the flexor retinaculum. The ulnar nerve enters the hand through Guyon's canal, a fibro-osseous tunnel formed by the pisiform and hook of the hamate. In the hand, the ulnar nerve branches to give rise to a palmar cutaneous (nerve of Henle) and dorsal cutaneous branch. The dorsal cutaneous nerve bifurcates further into radial and ulnar branches providing sensation to the dorsal hand.[4][5]
Muscles
The ulnar nerve innervates the flexor muscles of the forearm including the flexor carpi ulnaris and flexor digitorum profundus. It also innervates the intrinsic muscles of the hand including the palmaris brevis, lumbricals, hypothenar and interossei muscles. In the hand, superficial branch of the ulnar nerve innervates palmaris brevis muscle and sensory to the hypothenar muscles, fourth common digital nerve, and ulnar proper nerve. Deep branch innervates hypothenar muscles, opponens digiti minimi, interosseous muscles, third and fourth lumbricals, adductor pollicis and medial head of the flexor pollicis brevis.
Physiologic Variants
Anatomical variants are important to identify to promptly and correctly diagnose nerve dysfunction to prevent delay of treatment. Two nerve variations include Martin-Gruber and Riche-Cannieu anastomoses.[6]
Martin-Gruber anastomosis is a communication between the median and ulnar nerve in the forearm anywhere distal to the medial epicondyle. With this anatomical variant, the motor nerves innervating the intrinsic ulnar muscles are carried by the anterior interosseous branch of the median nerve. In the middle forearm, these fibers leave the anterior interosseous nerve to join the ulnar nerve. Therefore, with this variant, patients can present with functional intrinsic hand muscles despite dysfunction of the ulnar nerve.
Riche-Cannieu anastomosis occurs when the median and ulnar nerves connect in the palm. This variant displays as motor fibers that are typically carried by the median nerve, now carried by the ulnar nerve to the hand and then cross over in the palm. This is clinically significant in the setting of carpal tunnel syndrome. Patients with advanced median nerve pathology could have normal function of the standard median nerve distribution.
Surgical Considerations
The most common site of ulnar nerve entrapment is at the elbow in the cubital tunnel. Cubital tunnel decompression with possible ulnar nerve transposition is a relatively common orthopedic procedure. The cubital tunnel is comprised of Osbourne's ligament (cubital tunnel retinaculum) and the deep layer of the aponeurosis of the 2 heads of the flexor carpi ulnaris muscle. Osbourne’s ligament is the proximal roof of the cubital tunnel and prevents subluxation of the nerve with elbow flexion. Surgical decompression for cubital tunnel syndrome, Osbourne's fascia is incised to relieve pain and paresthesia caused by nerve injury. Transposition of the nerve from the arcade of Struthers to the flexor carpi ulnaris is also one of the recommended surgical treatments. The arcade of Struthers is formed by the internal brachial ligament, medial head of the triceps, and medial intermuscular septum just proximal to the medial epicondyle of the humerus. This is another possible site of ulnar nerve compression.[7][8][9]
Another surgical consideration includes incidental ulnar nerve damage during carpal tunnel release surgery. During surgical intervention for carpal tunnel syndrome, a small incision is made near the wrist crease. The surgeon will dissect through the soft tissues of the wrist down the transverse carpal ligament to relieve compression of the median nerve. Damage to the deep motor branch of the ulnar nerve can occur during this dissection as the branch courses just medial to the carpal tunnel along the hamate carpal bone. Although ulnar nerve damage is a rare complication of carpal tunnel release surgery, it is important for the incision to remain in line with the radial border of the ring finger.
Clinical Significance
Ulnar nerve injury can be caused by a number of reasons based on location of injury along the course of the nerve, most commonly at the elbow. Proximal injury to the lower trunk of the brachial plexus can result in Klumpke palsy, injury at the elbow may result in cubital tunnel syndrome, and compression at Guyon’s canal of the wrist can manifest as motor and sensory deficits in the hand.[10]
Klumpke palsy is the manifestation of a lower trunk injury to the brachial plexus. Most commonly, lower trunk injuries are a result of an upward force on an infant’s arm, or upward traction on the arm in an adult. Injury can also be a result of traumatic vaginal delivery with traction of a baby’s abducted arm due to large birth weight infant or small birth canal. Klumpke palsy has a functional deficit of the intrinsic hand muscles presenting clinically with a complete claw hand. Clinically, observe hyperextension of MCP joint due to loss of flexors, radial deviation of wrist due to loss of flexor carpi ulnaris, and wasting of intrinsic hand muscles (lumbricals, interossei, thenar and hypothenar muscles) with flexion of the distal interphalangeal and proximal interphalangeal joints. This syndrome is also known as strap hanger’s syndrome.
Horner syndrome (ptosis, miosis, and anhydrosis) can occur due to loss of sympathetic input from T1. Pupil constriction is the result of unopposed parasympathetic input to the eye.
The most common site of ulnar nerve injury is near the elbow. Nerve pathology can be caused by anatomic damage from fracture of the medial epicondyle, osteophyte infection, soft tissue mass, or synovitis at the elbow joint. The nerve may also be damaged due to compression from prolonged periods of elbow flexion like sleep, exercise, driving, typing, or talking on phone. Cubital tunnel syndrome is a peripheral neuropathy due to chronic compression or repetitive trauma of the ulnar nerve at the elbow between the medial epicondyle of the humerus and the olecranon process of the ulna.
Congenital laxity of the cubital tunnel retinaculum can be seen, resulting hypermobility of the ulnar nerve. This can lead to repetitive subluxation and possible anterior dislocation when then elbow is flexed. Repetitive trauma at this location may result in inflammation from recurrent friction over the medial epicondyle.
Ulnar nerve impingement can also occur at the wrist due to compression through Guyon’s canal, local trauma, ganglion cysts, and external nerve compression. The ulnar nerve and artery enter Guyon's canal, a fibro-osseous tunnel formed by the pisiform and hook of the hamate. The ulnar nerve bifurcates within the canal into superficial and deep branches. Nerve compression at the wrist can also be caused by bikers with excess pressure from handlebars and prolonged compression while typing at a desk.
Diagnosis of ulnar nerve injury can be made with a thorough history, musculoskeletal and neurological physical exam. However, EMG and nerve conduction studies can be used as an adjunct in order to diagnose and localize the lesion.