[1]
Kalali B, Formichella L, Gerhard M. Diagnosis of Helicobacter pylori: Changes towards the Future. Diseases (Basel, Switzerland). 2015 Jun 29:3(3):122-135. doi: 10.3390/diseases3030122. Epub 2015 Jun 29
[PubMed PMID: 28943614]
[2]
Wang YK, Kuo FC, Liu CJ, Wu MC, Shih HY, Wang SS, Wu JY, Kuo CH, Huang YK, Wu DC. Diagnosis of Helicobacter pylori infection: Current options and developments. World journal of gastroenterology. 2015 Oct 28:21(40):11221-35. doi: 10.3748/wjg.v21.i40.11221. Epub
[PubMed PMID: 26523098]
[3]
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, Malfertheiner P, Graham DY, Wong VWS, Wu JCY, Chan FKL, Sung JJY, Kaplan GG, Ng SC. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017 Aug:153(2):420-429. doi: 10.1053/j.gastro.2017.04.022. Epub 2017 Apr 27
[PubMed PMID: 28456631]
Level 1 (high-level) evidence
[4]
Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet (London, England). 1983 Jun 4:1(8336):1273-5
[PubMed PMID: 6134060]
[5]
Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. The American journal of gastroenterology. 2017 Feb:112(2):212-239. doi: 10.1038/ajg.2016.563. Epub 2017 Jan 10
[PubMed PMID: 28071659]
[6]
Delvin EE, Brazier JL, Deslandres C, Alvarez F, Russo P, Seidman E. Accuracy of the [13C]-urea breath test in diagnosing Helicobacter pylori gastritis in pediatric patients. Journal of pediatric gastroenterology and nutrition. 1999 Jan:28(1):59-62
[PubMed PMID: 9890470]
[7]
Lopes AI, Vale FF, Oleastro M. Helicobacter pylori infection - recent developments in diagnosis. World journal of gastroenterology. 2014 Jul 28:20(28):9299-313. doi: 10.3748/wjg.v20.i28.9299. Epub
[PubMed PMID: 25071324]
[8]
Sabbagh P, Mohammadnia-Afrouzi M, Javanian M, Babazadeh A, Koppolu V, Vasigala VR, Nouri HR, Ebrahimpour S. Diagnostic methods for Helicobacter pylori infection: ideals, options, and limitations. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 2019 Jan:38(1):55-66. doi: 10.1007/s10096-018-3414-4. Epub 2018 Nov 9
[PubMed PMID: 30414090]
[9]
Best LM, Takwoingi Y, Siddique S, Selladurai A, Gandhi A, Low B, Yaghoobi M, Gurusamy KS. Non-invasive diagnostic tests for Helicobacter pylori infection. The Cochrane database of systematic reviews. 2018 Mar 15:3(3):CD012080. doi: 10.1002/14651858.CD012080.pub2. Epub 2018 Mar 15
[PubMed PMID: 29543326]
Level 1 (high-level) evidence
[10]
Patel SK, Pratap CB, Jain AK, Gulati AK, Nath G. Diagnosis of Helicobacter pylori: what should be the gold standard? World journal of gastroenterology. 2014 Sep 28:20(36):12847-59. doi: 10.3748/wjg.v20.i36.12847. Epub
[PubMed PMID: 25278682]
[11]
Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, Axon AT, Bazzoli F, Gasbarrini A, Atherton J, Graham DY, Hunt R, Moayyedi P, Rokkas T, Rugge M, Selgrad M, Suerbaum S, Sugano K, El-Omar EM, European Helicobacter and Microbiota Study Group and Consensus panel. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017 Jan:66(1):6-30. doi: 10.1136/gutjnl-2016-312288. Epub 2016 Oct 5
[PubMed PMID: 27707777]
Level 3 (low-level) evidence
[12]
Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N. ACG and CAG Clinical Guideline: Management of Dyspepsia. The American journal of gastroenterology. 2017 Jul:112(7):988-1013. doi: 10.1038/ajg.2017.154. Epub 2017 Jun 20
[PubMed PMID: 28631728]
[13]
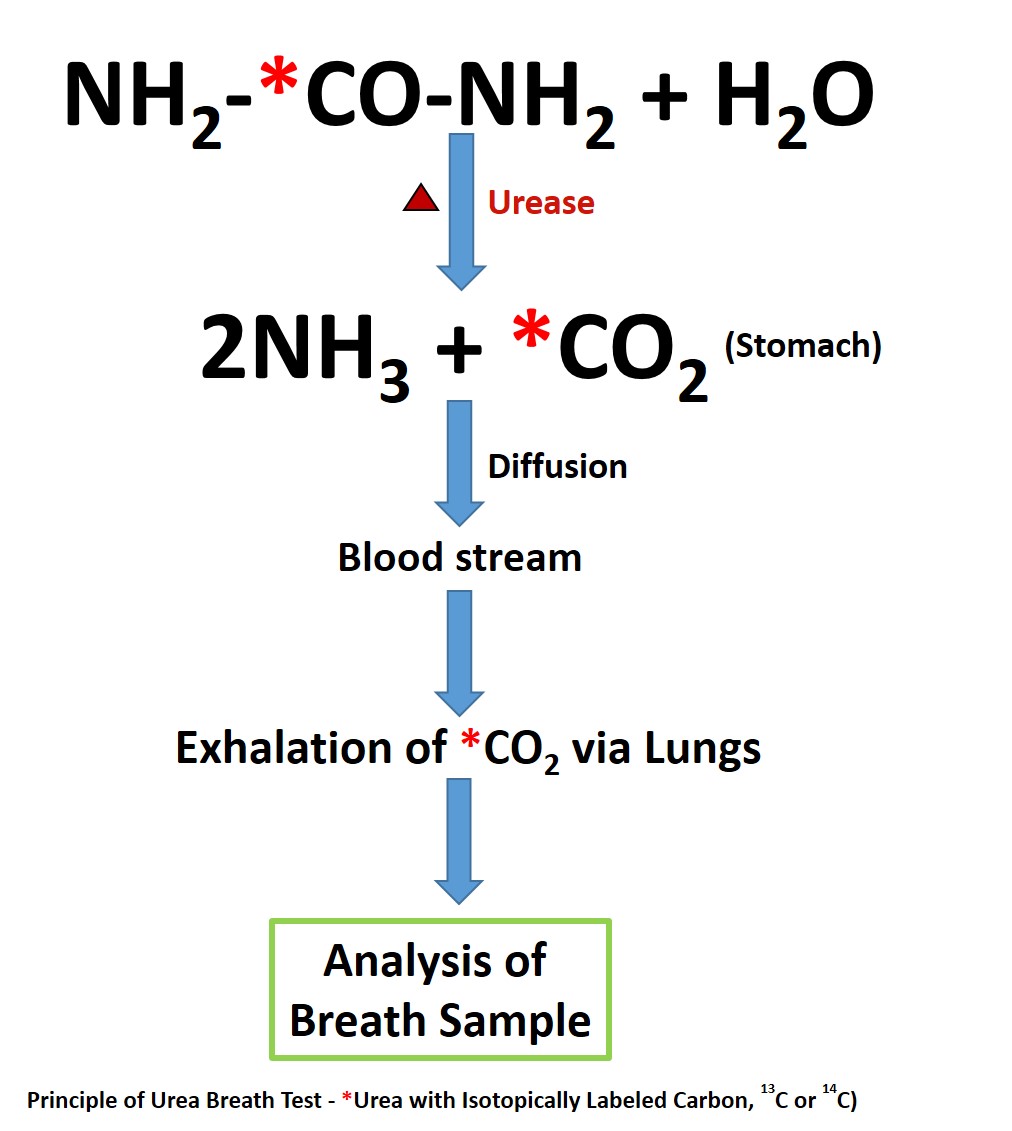
Ling D. Carbon-13 urea breath test for Helicobacter pylori infection in patients with uninvestigated ulcer-like dyspepsia: an evidence-based analysis. Ontario health technology assessment series. 2013:13(19):1-30
[PubMed PMID: 24228082]
[14]
Ford AC, Qume M, Moayyedi P, Arents NL, Lassen AT, Logan RF, McColl KE, Myres P, Delaney BC. Helicobacter pylori "test and treat" or endoscopy for managing dyspepsia: an individual patient data meta-analysis. Gastroenterology. 2005 Jun:128(7):1838-44
[PubMed PMID: 15940619]
[15]
Crowe SE. Helicobacter pylori Infection. The New England journal of medicine. 2019 Mar 21:380(12):1158-1165. doi: 10.1056/NEJMcp1710945. Epub
[PubMed PMID: 30893536]
[16]
Chey WD, Wong BC, Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. The American journal of gastroenterology. 2007 Aug:102(8):1808-25
[PubMed PMID: 17608775]
[17]
Talley NJ, Vakil NB, Moayyedi P. American gastroenterological association technical review on the evaluation of dyspepsia. Gastroenterology. 2005 Nov:129(5):1756-80
[PubMed PMID: 16285971]
[18]
Skrebinska S, Mégraud F, Bessède E. Diagnosis of Helicobacter pylori infection. Helicobacter. 2018 Sep:23 Suppl 1():e12515. doi: 10.1111/hel.12515. Epub
[PubMed PMID: 30203584]
[19]
Choi J, Kim CH, Kim D, Chung SJ, Song JH, Kang JM, Yang JI, Park MJ, Kim YS, Yim JY, Lim SH, Kim JS, Jung HC, Song IS. Prospective evaluation of a new stool antigen test for the detection of Helicobacter pylori, in comparison with histology, rapid urease test, (13)C-urea breath test, and serology. Journal of gastroenterology and hepatology. 2011 Jun:26(6):1053-9. doi: 10.1111/j.1440-1746.2011.06705.x. Epub
[PubMed PMID: 21362044]
[20]
Savarino V, Vigneri S, Celle G. The 13C urea breath test in the diagnosis of Helicobacter pylori infection. Gut. 1999 Jul:45 Suppl 1(Suppl 1):I18-22
[PubMed PMID: 10457031]
[21]
Osaki T, Mabe K, Hanawa T, Kamiya S. Urease-positive bacteria in the stomach induce a false-positive reaction in a urea breath test for diagnosis of Helicobacter pylori infection. Journal of medical microbiology. 2008 Jul:57(Pt 7):814-819. doi: 10.1099/jmm.0.47768-0. Epub
[PubMed PMID: 18566138]
[22]
Borriello SP, Reed PJ, Dolby JM, Barclay FE, Webster AD. Microbial and metabolic profile of achlorhydric stomach: comparison of pernicious anaemia and hypogammaglobulinaemia. Journal of clinical pathology. 1985 Aug:38(8):946-53
[PubMed PMID: 4031106]
[23]
Ferwana M, Abdulmajeed I, Alhajiahmed A, Madani W, Firwana B, Hasan R, Altayar O, Limburg PJ, Murad MH, Knawy B. Accuracy of urea breath test in Helicobacter pylori infection: meta-analysis. World journal of gastroenterology. 2015 Jan 28:21(4):1305-14. doi: 10.3748/wjg.v21.i4.1305. Epub
[PubMed PMID: 25632206]
Level 1 (high-level) evidence
[24]
Leal YA, Flores LL, Fuentes-Pananá EM, Cedillo-Rivera R, Torres J. 13C-urea breath test for the diagnosis of Helicobacter pylori infection in children: a systematic review and meta-analysis. Helicobacter. 2011 Aug:16(4):327-37. doi: 10.1111/j.1523-5378.2011.00863.x. Epub
[PubMed PMID: 21762274]
Level 1 (high-level) evidence
[25]
Laine L, Estrada R, Trujillo M, Knigge K, Fennerty MB. Effect of proton-pump inhibitor therapy on diagnostic testing for Helicobacter pylori. Annals of internal medicine. 1998 Oct 1:129(7):547-50
[PubMed PMID: 9758575]
[26]
Bravo LE, Realpe JL, Campo C, Mera R, Correa P. Effects of acid suppression and bismuth medications on the performance of diagnostic tests for Helicobacter pylori infection. The American journal of gastroenterology. 1999 Sep:94(9):2380-3
[PubMed PMID: 10483995]
[27]
Klein PD, Malaty HM, Martin RF, Graham KS, Genta RM, Graham DY. Noninvasive detection of Helicobacter pylori infection in clinical practice: the 13C urea breath test. The American journal of gastroenterology. 1996 Apr:91(4):690-4
[PubMed PMID: 8677930]
[28]
Logan RP. Urea breath tests in the management of Helicobacter pylori infection. Gut. 1998 Jul:43 Suppl 1(Suppl 1):S47-50
[PubMed PMID: 9764040]
[29]
Graham DY, Klein PD, Evans DJ Jr, Evans DG, Alpert LC, Opekun AR, Boutton TW. Campylobacter pylori detected noninvasively by the 13C-urea breath test. Lancet (London, England). 1987 May 23:1(8543):1174-7
[PubMed PMID: 2883491]
[30]
Perets TT, Gingold-Belfer R, Leibovitzh H, Itskoviz D, Schmilovitz-Weiss H, Snir Y, Dickman R, Dotan I, Levi Z, Boltin D. Optimization of (13) C-urea breath test threshold levels for the detection of Helicobacter pylori infection in a national referral laboratory. Journal of clinical laboratory analysis. 2019 Feb:33(2):e22674. doi: 10.1002/jcla.22674. Epub 2018 Sep 17
[PubMed PMID: 30221401]
[31]
Mauro M, Radovic V, Zhou P, Wolfe M, Kamath M, Bercik P, Croitoru K, Armstrong D. 13C urea breath test for (Helicobacter pylori): determination of the optimal cut-off point in a Canadian community population. Canadian journal of gastroenterology = Journal canadien de gastroenterologie. 2006 Dec:20(12):770-4
[PubMed PMID: 17171195]
[32]
Houghton J, Wang TC. Helicobacter pylori and gastric cancer: a new paradigm for inflammation-associated epithelial cancers. Gastroenterology. 2005 May:128(6):1567-78
[PubMed PMID: 15887152]
[33]
Santambrogio E, Orsucci L. Helicobacter pylori and hematological disorders. Minerva gastroenterologica e dietologica. 2019 Sep:65(3):204-213. doi: 10.23736/S1121-421X.19.02580-7. Epub 2019 Apr 16
[PubMed PMID: 30994322]
[34]
Garza-González E, Perez-Perez GI, Maldonado-Garza HJ, Bosques-Padilla FJ. A review of Helicobacter pylori diagnosis, treatment, and methods to detect eradication. World journal of gastroenterology. 2014 Feb 14:20(6):1438-49. doi: 10.3748/wjg.v20.i6.1438. Epub
[PubMed PMID: 24587620]
[35]
Hamlet AK, Erlandsson KI, Olbe L, Svennerholm AM, Backman VE, Pettersson AB. A simple, rapid, and highly reliable capsule-based 14C urea breath test for diagnosis of Helicobacter pylori infection. Scandinavian journal of gastroenterology. 1995 Nov:30(11):1058-63
[PubMed PMID: 8578164]
[36]
Capurso G, Carnuccio A, Lahner E, Panzuto F, Baccini F, Delle Fave G, Annibale B. Corpus-predominant gastritis as a risk factor for false-negative 13C-urea breath test results. Alimentary pharmacology & therapeutics. 2006 Nov 15:24(10):1453-60
[PubMed PMID: 17032284]