Continuing Education Activity
Diabetic foot ulcers are among the most common complications of patients who have diabetes mellitus which is not well controlled. It is usually the result of poor glycemic control, underlying neuropathy, peripheral vascular disease, or poor foot care. It is also one of the common cause for osteomyelitis of the foot and amputation of lower extremities. These ulcers are usually in the areas of the foot which encounters repetitive trauma and pressure sensations. Staphylococcus is the most common infective organism. The disease is typically chronic, and an interprofessional approach will have the best outcome. The combined involvement of podiatrist, endocrinologist, primary care physician, vascular surgeon, and an infectious disease specialist is extremely beneficial. This activity reviews the evaluation, treatment, and complications of diabetic foot ulcers and underscores the importance of an interprofessional team approach to its management.
Objectives:
- Describe the pathophysiology and progression of diabetic foot ulcers.
- Review the risk factors associated with diabetic foot ulcers.
- List the treatment and management options available for diabetic foot ulcers.
- Explain the importance of improving coordination amongst the interprofessional team to enhance care for patients affected by diabetic foot ulcers.
Introduction
Diabetic foot ulcers are among the most common complications of patients who have diabetes mellitus which is not well controlled. It is usually the result of poor glycemic control, underlying neuropathy, peripheral vascular disease, or poor foot care. It is also one of the common cause for osteomyelitis of the foot and amputation of lower extremities. These ulcers are usually in the areas of the foot which encounters repetitive trauma and pressure sensations.[1] Staphylococcus is the common infective organism. The disease is typically chronic, and an interprofessional approach will have the best outcome. The combined involvement of podiatrist, endocrinologist, primary care physician, vascular surgeon, and an infectious disease specialist is extremely beneficial. It is a commonly encountered scenario in both outpatient settings and inpatients.
Diabetic foot ulcers are responsible for more admissions than any other diabetic complication. Today, diabetes is the leading cause of non-traumatic amputations in the US. Overall, about 5% of patients with diabetes mellitus develop foot ulcers and 1% end up with an amputation.
Educating the patient about the complication and the need for proper medical care will reduce the risk of complications and good compliance.
Etiology
The etiology for diabetic foot ulcer is multifactorial. The common underlying causes are poor glycemic control, calluses, foot deformities, improper foot care, ill-fitting footwear, underlying peripheral neuropathy and poor circulation, dry skin, etc.
About 60% of diabetics will develop neuropathy, eventually leading to a foot ulcer. The risk of a foot ulcer is increased in individuals with a flat foot as they have disproportionate stress across the foot, leading to tissue inflammation in high risk areas of the foot.
Epidemiology
The annual incidence of diabetic foot ulcer worldwide is between 9.1 to 26.1 million.[2] Around 15 to 25% of patients with diabetes mellitus will develop a diabetic foot ulcer during their lifetime.[3] As the number of newly diagnosed diabetics are increasing yearly, the incidence of diabetic foot ulcer is also bound to increase.
Diabetic foot ulcers can occur at any age but are most prevalent in patients with diabetes mellitus ages 45 and over. Latinos, African Americans, and Native Americans have the highest incidence of foot ulcers in the US.
Pathophysiology
The development of a diabetic ulcer is usually in 3 stages. The initial stage is the development of a callus. The callus results from neuropathy. The motor neuropathy causes physical deformity of the foot, and sensory neuropathy causes sensory loss which leads to ongoing trauma. Drying of the skin because of autonomic neuropathy is also another contributing factor. Finally, frequent trauma of the callus results in subcutaneous hemorrhage and eventually, it erodes and becomes an ulcer.[2]
Patients with diabetes mellitus also develop severe atherosclerosis of the small blood vessels in the legs and feet, leading to vascular compromise, which is another cause for diabetic foot infections. Because blood is not able to reach the wound, healing is delayed, eventually leading to necrosis and gangrene.
History and Physical
Getting a good history is vital in the care of patients with a diabetic ulcer. The history should include the duration of diabetes, glycemic control, other pre-existing complications of diabetes including sensory neuropathy, history of peripheral vascular disease, callus, previous ulcer, prior treatment, and the outcome. The detailed history should also include information regarding the footwear and foot.
The clinical examination should include examining the peripheral pulses of the feet, looking for any anatomical anomalies, the presence of callus, signs of vascular insufficiency, which may indicate loss of hair, muscle atrophy, and location of the ulcer. Also assess for the presence of purulence, scabs, and evidence of neuropathy by examining with a monofilament.
Features indication neuropathy include:
- Paresthesia
- Hypo or hyperesthesia
- Dysesthesia
- Anhydrosis
Ulcers are most common in the weight-bearing areas such as the plantar metatarsal head, heel, tips of hammer toes and other prominent areas. Other physical features include hammertoes, brittle nails, calluses, and fissures.
Evaluation
The most common laboratory investigations done during evaluation of the ulcer include a fasting blood sugar, glycated hemoglobin levels, complete metabolic panel, a complete blood count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
Recent guidelines and the literature suggest that in patients with diabetic foot ulcers, results of specimens for culture taken by swabbing do not correlate well with those obtained by deep tissue sampling; this suggests that superficial swab specimens may be less reliable for guiding antimicrobial therapy than deep tissue specimens.[3]
Radiological investigations include plain x-rays to look for any underlying osteomyelitis, the presence of air in the subcutaneous tissue, any signs of underlying fractures, and presence of a foreign body. If osteomyelitis is suspected, MRI is the most preferred test. A bone scan with technetium can also be used to diagnose underlying osteomyelitis. Arterial Doppler with ankle-brachial index (ABI) is useful to rule out underlying peripheral vascular disease.
The probe-to-bone test (PTB) i dperformed by probing the ulcer with a sterile metal probe is a bedside test that can help with the diagnosis of underlying osteomyelitis. If the probe hits the bone, it is a positive test.[4] Positive probe-to-bone test results are helpful especially when conducted on patients with diabetes mellitus.[5]
Treatment / Management
Treatment of diabetic foot ulcer should be systematic for an optimal outcome. The most important point is to identify if there is any evidence of ongoing infection, by obtaining a history of chills, fever, looking for the presence of purulence or presence of at least two signs of inflammation that includes, pain, warmth, erythema or induration of the ulcer. It should is noteworthy that even in the presence of severe diabetic foot infection, there can be minimal systemic signs of infection.[6]
The next step is to decide if the patient’s ulcer can is manageable in the outpatient setting or inpatient setting. Need for parenteral antibiotics, concern for noncompliance, inability to care for the wound, ability to offload pressure, are few points to be considered for hospitalization.[7] Both categories of patients should have treatment with antibiotics.
The common organisms seen in a diabetic foot ulcer are Staphylococcus aureus, Streptococcus, Pseudomonas aeruginosa, and rarely E. coli. Diabetes patients have higher carriage rate of Staphylococcus aureus in the nares and skin, and this increases the chances of infection of the ulcer.[8]Antibiotics are only needed if there is a concern for infection. The severity of the infection dictates the dose, duration, and the type of antibiotic.
The typical outpatient antibiotics regimen includes oral cephalosporins, and amoxicillin-clavulanic acid combination, (If MRSA is not of concern). If MRSA is suspected, then the oral regimens include linezolid, clindamycin or cephalexin plus doxycycline or a trimethoprim-sulphamethoxazole combination.
Parenteral antibiotic regimens include piperacillin-tazobactam, ampicillin-sulbactam, and if penicillin-allergic, then carbapenems including ertapenem or meropenem. The other combinations regimen including adding metronidazole for anaerobic coverage along with quinolones like ciprofloxacin or levofloxacin, or with cephalosporins like ceftriaxone, cefepime or ceftazidime. Intravenous agents which cover MRSA include vancomycin, linezolid or daptomycin.[9]
The next therapeutic step is to treat any underlying peripheral vascular disease. Inadequate blood supply limits the oxygen supply and the delivery of the antibiotics to the ulcer; hence revascularization improves both, and there is a better chance for the healing of the ulcer. The subsequent step is to perform local debridement or removal of calluses.
Vacuum assisted closure can be undertaken for clean non healing wounds. Others may benefit from hydrotherapy to get rid of infected debris.
If the patient has charcot foot, then the initial treatment is immobilization with braces or specially made shoes, but most will require a surgical procedure like arthrodesis or an osteotomy.
Finally, efforts should be made for the prevention of new ulcers or worsening of the existing ulcer, which occurs by offloading the pressure from the site by using walkers or therapeutic shoes.[10] If the wound fails to heal in 30 days, then hyperbaric oxygen therapy can be considered. Since the wound has low oxygen supply, there is often delay in healing of the wound. Hyperbaric oxygen therapy improves the rate of wound healing and also reduces the rate of complications.[11]
To have the best outcome a team of health care providers including primary care physician, podiatrist, a vascular surgeon, an infectious disease specialist and wound care nursing staff are imperative.
Differential Diagnosis
- Superficial thrombophlebitis
Staging
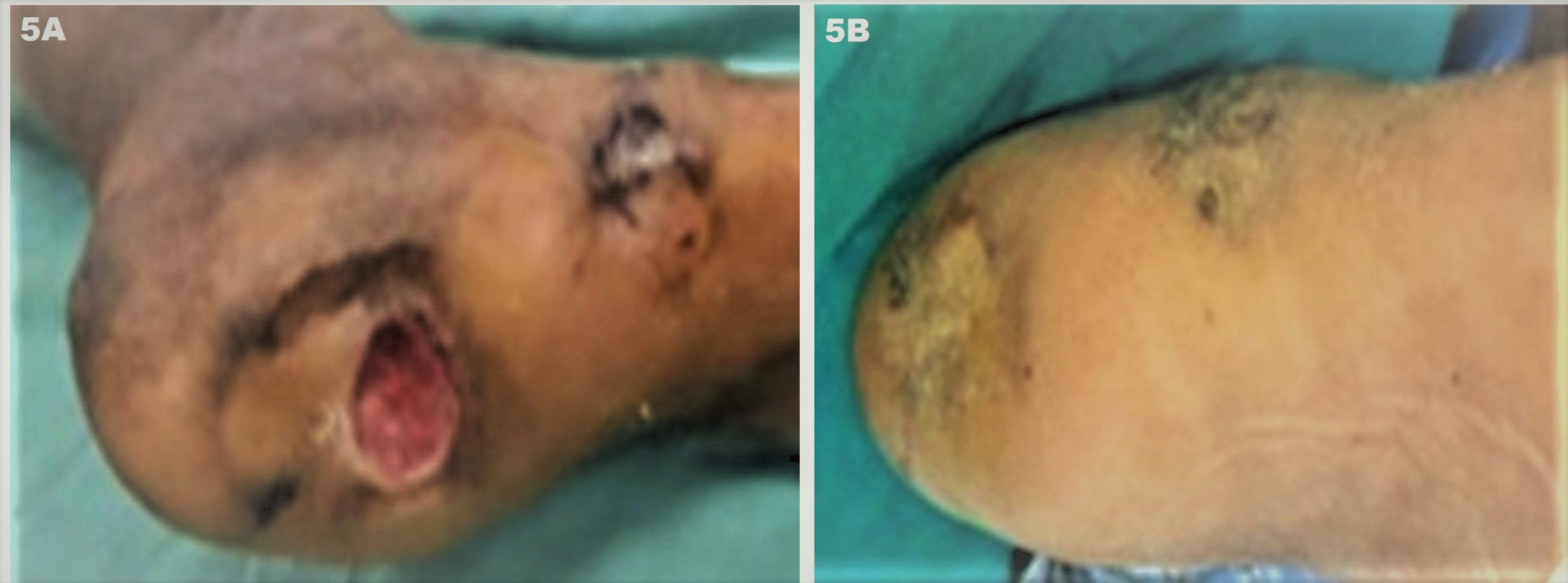
After the diagnosis of the ulcer, it should undergo staging. One of the commonly used classifications is by Wagner from 1981. It classifies wounds into six grades based on the depth [12]
Grade/Features
1/Superficial ulcer
2/Deep ulcer involving tendon bone or joint
3/Deep ulcer with abscess or osteomyelitis
4/Gangrene involving the forefoot
5/Gangrene involving the entire Foot
This classification, though, has been criticized as grading merely the depth of the ulceration and not incorporating other factors known to influence the outcome. Among others, one of the most commonly used classification today is The University of Texas Classification, which not only includes assessment of the depth, but also the type of infection, and ischemia based on the eventual outcome of the wound.[13]
Prognosis
The prognosis these ulcers is good if identified early and optimal treatment initiated. Unfortunately, delays in care can have detrimental effects which can lead even to amputation of the foot. Patients who have chronic diabetic ulcer have a high risk of rehospitalization and prolonged hospitalization.
Complications
The most feared complication is amputation of the extremity. The other complications include gangrene of the foot, osteomyelitis, permanent deformity, and risk of sepsis.
Postoperative and Rehabilitation Care
Patients who end up with amputation will need comprehensive therapy including physical therapy, occupational therapy and also will need a prosthesis.
Consultations
- Internal Medicine
- Podiatrist
- Endocrinology
- Vascular surgeon
- Infectious disease
Deterrence and Patient Education
The most important preventative measure is patient education. If the patient should be made aware about the importance of good glycemic control, proper care of the foot, avoiding tobacco and the need for frequent follow-up examinations, then the risk for developing ulcer is significantly reduced. The patient should be reminded of these things during each visit with the primary care physician.
Pearls and Other Issues
- Education is the cardinal factor in prevention and a good outcome in this entity
- An interprofessional approach is essential
- Antibiotics are only needed if there is suspicion for infection.
- Diabetic ulcers are a common risk factor for lower limb amputations
Enhancing Healthcare Team Outcomes
Diabetes is a chronic disease that has a significant number of life-threatening complications, of which one of them is a foot ulcer. Diabetic foot is a common scenario in which healthcare workers will come across in daily practice. Besides a lack of blood flow, many patients with diabetes mellitus with a foot ulcer also have neuropathy for which there is no cure. The diagnosis and subsequent management of a diabetic ulcer are optimally effective when utilizing an interprofessional approach to achieve the best outcome.
Many patients with diabetes mellitus with a foot ulcer end up with amputations and become disabled. Thus, today the key is preventing the foot ulcer with education. The pharmacist, nurse practitioner, the primary care provider should educate the patient on the harms of smoking and the need for better control of blood glucose. In addition, patients with diabetes mellitus need to be taught about appropriate shoe wear, podiatric care, and control of hyperlipidemia. The team, including the diabetic nurse educator and clinicians, must work together toward educating the patient and family on preventative measures to minimize morbidity and improve outcomes.
The social worker should be involved in the care to ensure that the patient with diabetes mellitus has support systems and finances so that care is not jeopardized. The dietitian should educate the patient on a healthy diet and the importance of maintaining a healthy weight. At every clinic visit, the feet must be examined for skin integrity, pulses and sensation. Appropriate referrals must be made if there are any deficiencies in the foot exam. Patients with diabetes mellitus should be told that anytime they have an open wound, they should seek immediate care and avoid homemade remedies. Only through an interprofessional approach with open communication can the morbidity of diabetic foot be reduced.
Outcomes
Loss of a limb leads to enormous morbidity and many patients are not able to afford a prosthesis. Most remain disabled for life and lead a poor quality of life.