Introduction
Initially described in 1785 by Sandifort, the tracheal bronchus is a rare congenital anomaly in which an accessory bronchus originates directly from the trachea rather than branching from one of the mainstem bronchi distal to the carina.[1] The accessory bronchus is directed towards the upper lobe of the lung and is significantly more common on the right side.[1][2][1] Most commonly, the accessory bronchus originates within 2 cm of the carina, though it can arise anywhere between the cricoid and the carina. Some authors suggest that if this abnormal bronchus supplies the entire upper lobe of the lung, then it is called bronchus suis or pig bronchus. However, both of these terms are used inconsistently in the literature to describe any right-sided tracheal bronchus.[3][4] There are scattered case reports of recurrent atelectasis or pneumonia supplied by the aberrant bronchus, but the lung parenchyma supplied by the tracheal bronchus is typically normal and functional, and this condition is most often noted only incidentally on imaging or bronchoscopy performed for other reasons.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The precise origins of tracheal bronchus remain controversial. Tracheobronchial development begins early in embryogenesis, with lobar differentiation of the lungs commencing around days 29 to 30. Supranumerary bronchial anomalies are believed to occur during this timeframe, whereas bronchial displacement anomalies are more likely to arise after day 32, as the distal branching continues to develop.[4][6][4]
There are 3 theories regarding the origins of the tracheal bronchus:
- Reduction theory: This theory postulates that a basic, primitive pattern of tracheobronchial branching develops first in embryogenesis, and the final branching architecture is formed through regression, shrinkage, or suppression of portions of this original primitive distribution. Any aberrance in this process can result in bronchial branching anomalies, including tracheal bronchi.[2][7][2]
- Migration theory (extension theory): According to this theory, a bilateral, symmetric bronchial branching pattern with a fixed number of derivative branches exists first, and subsidiary branches of these fixed derivatives can migrate from their initial location to other locations within the tracheobronchial tree.[2][8]
Epidemiology
The overall incidence of tracheal bronchus is 0.9% to 5%, with the majority of cases arising from the right lateral wall of the trachea.[10] The prevalence of tracheal bronchus is 0.1% to 2% on the right side and 0.3% to 1% on the left side.[3] The tracheal bronchus is associated with other congenital abnormalities, such as Down syndrome, VATER (vertebral, anal, tracheoesophageal, and renal defects), tracheoesophageal fistula, esophageal atresia, laryngeal and duodenal webs, spinal fusion defects, cardiac congenital defects, and hypoplastic lung. In the pediatric population, tracheal bronchus detected by flexible bronchoscopy had an incidence of 1.9% at a median age of 15 months (age range 1 month to 13 years), with no gender differences. There are concurrent congenital pathologies reported in 92.3% of cases, with heart disease accounting for 69%, chromosomal abnormality for 35%, and spinal fusion defect for 11%.[11][12]
Pathophysiology
Although the majority of tracheal bronchi are asymptomatic and may not be discovered until adulthood, symptoms can occur in up to 25% of patients in some series.[13] Any obstruction of the tracheal bronchus can lead to atelectasis, decreased ventilation, and infection. Hence, in children, recurrent upper lobe pneumonia may be the diagnostic presentation of a tracheal bronchus.[11] Abnormal ventilation mechanics may contribute to patient symptoms, with additional presentations including wheezing and hypoxia, which could be mistaken for asthma.[14] Cases have been reported of tracheal bronchus associated with tuberculosis, leiomyoma, cancers, and as a source of bleeding leading to death. There is insufficient evidence to suggest any association between the tracheal bronchus and its predisposition to any malignancy.[15][16][17][18]
One classification system categorizes the location of the tracheal bronchus in relation to the carina:
- Type I: The tracheal bronchus is more than 2 cm from the carina, and there is a narrowing of the distal trachea.
- Type II: The tracheal bronchus is more than 2 cm from the carina, but there is no narrowing of the distal trachea.
- Type III: The tracheal bronchus is less than 2 cm above the carina.[19]
Another classification system describes tracheal bronchi relative to the upper lobe bronchus and pulmonary arteries:
- A normal right upper lobe bronchus is termed eparterial, as it arises cranial to the right pulmonary artery.
- A normal left upper lobe bronchus is called hyparterial, as it arises caudal to the normal left pulmonary artery.
- An aberrant bronchus arising proximal to the upper lobe bronchus is called pre-eparterial on the right side and eparterial or pre-hyparterial on the left side.
- An aberrant bronchus arising distal to the upper lobe bronchus is called post-eparterial on the right side and post-hyparterial on the left side.[2][4]
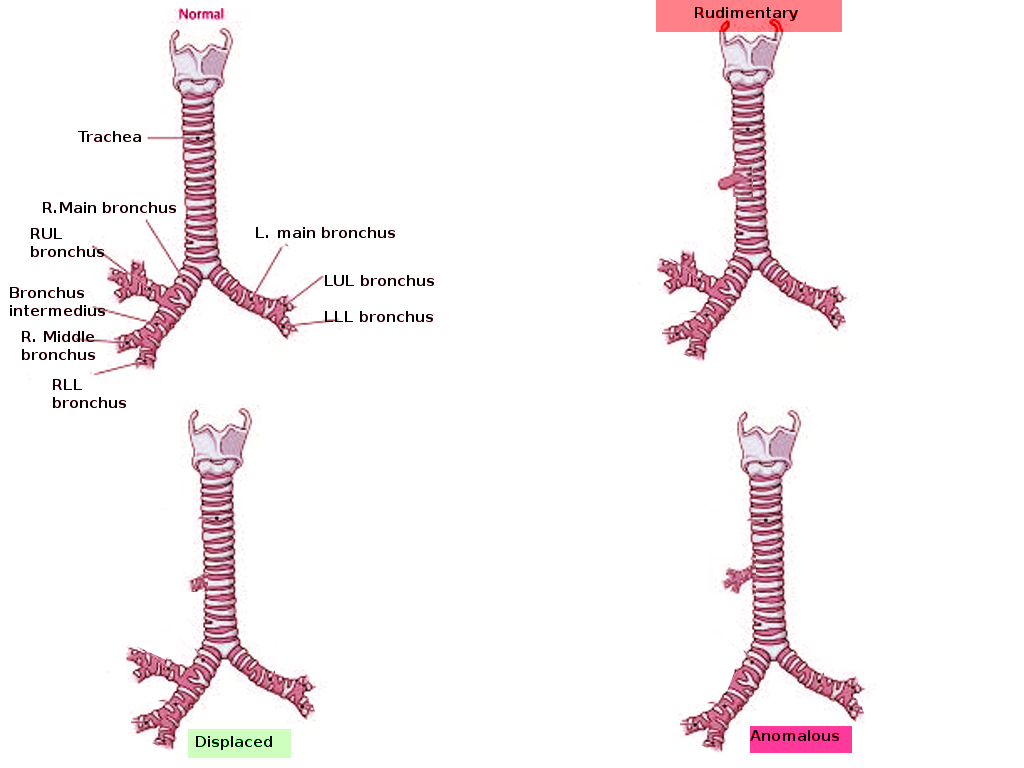
Tracheal bronchus may also be classified according to hypothetical embryologic origin as either displaced or supernumerary:
- If the anatomic upper lobe bronchus is missing a single branch, the tracheal bronchus is defined as displaced.
- If the right upper lobe bronchus has a normal trifurcation into apical, posterior, and anterior segmental bronchi, the tracheal bronchus is defined as supernumerary.
The supernumerary bronchi may end blindly; in such cases, they are also called tracheal diverticula. If they terminate in aerated or bronchiectatic lung tissue, it is termed either an apical accessory lung or a tracheal lobe.[20]
Incidental intubation of the tracheal bronchus can cause obstruction, pneumothorax, post-obstructive pneumonia, and respiratory failure.[21]
History and Physical
Children may remain asymptomatic; however, symptomatic cases often manifest early in life with wheezing, stridor, refractory cough, pneumonia, or atelectasis.[12] Tracheal bronchus should be suspected in cases of persistent upper lobe pneumonia, atelectasis or air trapping, and chronic bronchitis. This condition can present with chronic symptoms, such as productive cough over multiple years, or it may also present as recurrent pneumonia with computed tomography (CT) findings of bronchiectasis.[22] Important aspects of the history include any seasonal or environmental variations, association with eating or swallowing, any positional factors, association with exercise, concern for foreign body aspirations, and any smokers in the home. As the most common presenting symptoms are vague, these historical factors aid in identifying other conditions that may mimic the presentation of a symptomatic tracheal bronchus, such as asthma, allergies, laryngomalacia, tracheobronchial foreign body, or acid reflux.[23][24]
Physical examination of a patient with a suspected airway abnormality should begin with a comprehensive upper respiratory examination.[25] Vital signs must be recorded, and a thorough assessment of the individual's overall general appearance should be conducted. Attention should be given to the respiratory rate, and any breathing-associated noises, such as stridor or stertor, should be reported.[26] If present, the clinician should determine whether these noises occur with mouth breathing, nasal breathing, or both. Any vascular lesions of the head or neck should be noted. These lesions should also be characterized as inspiratory, expiratory, or biphasic. The use of accessory muscles during respiration should be noted. In infants and children, it is important to note whether these symptoms worsen when crying and whether there is any positional component, such as whether symptoms are worse when supine or improved when placed prone.[27] The quality of the voice and the nature of the cough should also be assessed. Hoarseness may suggest laryngeal pathology, whereas a bovine cough may indicate vocal cord paralysis. The examination should then proceed with a thorough cardiopulmonary examination. All lung fields should be auscultated and percussed, with additional signs to elucidate lung consolidation, such as tactile fremitus, or 'e' to 'a' changes, assessed.[28] The final component of the in-office examination is flexible laryngoscopy. This procedure should evaluate the nasal airway bilaterally for conditions such as pyriform aperture stenosis or choanal atresia and evaluate the larynx. Vocal cord function and appearance should be assessed to identify neoplastic or infectious lesions. The subglottis and proximal trachea are often visible, but the lower airways are not reliably visualized through this technique.[29]
Evaluation
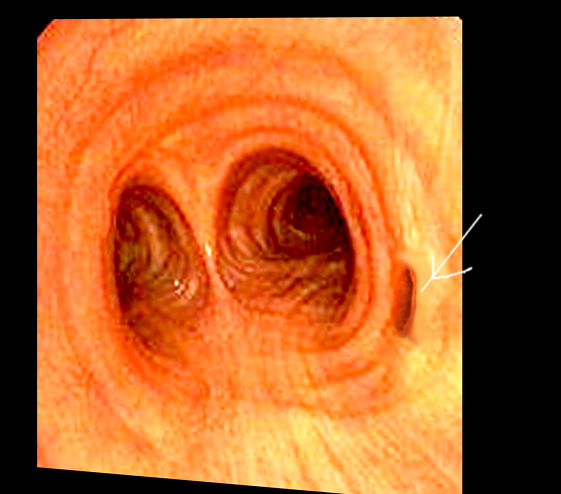
The definitive diagnosis of tracheal bronchus is established through direct visualization on bronchoscopy. This procedure allows for a comprehensive examination of the tracheobronchial tree while also assessing for coexisting pathologies such as tracheomalacia, bronchomalacia, tracheoesophageal fistula, vascular rings or vascular lesions, neoplasms, or foreign bodies.[30] In cases where tracheal bronchus is found incidentally, such as during intubation and in the perioperative setting, special attention should be paid. Extra care should be taken while intubating patients with tracheal bronchus as the tube can potentially obstruct or even migrate into the bronchus itself, resulting in atelectasis, hypoventilation, or both.[31]
Chest x-rays can occasionally reveal a tracheal bronchus; however, it is more commonly identified incidentally on chest CT scans performed for other reasons.[32] Multi-detector CT (MDCT) with three-dimensional (3D) image reconstruction is the gold-standard test for detecting congenital tracheobronchial anomalies. In addition, 3D-CT is a valuable tool for diagnosing the relationship between the tracheal and arterial tree. Reconstruction images have overcome the limitations of axial CT images, which included failure to identify subtle tracheal stenosis, a craniocaudal extension of the airway disease, and disease limited to airways obliquely located to axial planes. Imaging findings in symptomatic patients include bronchiectasis, focal emphysema, and focal cystic malformations.[33][34][35]
A retrospective cross-sectional analysis of 20 individuals with different tracheobronchial anomalies, such as stenosis, tracheomalacia, tracheal bronchus, and agenesis, compared the diagnostic benefit of magnetic resonance imaging (MRI), MDCT, and 3D imaging confirmed by bronchoscopy or surgery. The study found that MDCT was superior to MRI in diagnosing anomalies. In 12 patients who underwent both MDCT and 3D imaging, researchers determined that reconstruction provided specific information in 7 cases; in 3 cases, it played a crucial role in attempting surgical interventions, whereas in another 4 cases, it provided specific information for surgical planning.[36]
Treatment / Management
Currently, the primary approach to managing tracheal bronchus is symptomatic treatment. Asymptomatic cases require only expectant observation, whereas symptomatic tracheal bronchus is treated based on the severity of symptoms. Given the broad range of symptoms that tracheal bronchus can present, medical management includes bronchodilators, inhaled corticosteroids, muscarinic antagonists, and antibiotics. However, if the symptoms are refractory to medication, then surgical treatment is indicated. Segmentectomy and lobectomy have been performed for recurrent pneumonia caused by the tracheal bronchus and have been shown to be curative.[37]
When surgery is considered, careful coordination between the anesthetist and the surgical team is paramount. Based on normal anatomy, the left main bronchus is longer and divides into upper and lower secondary bronchi. The right main bronchus is shorter and divides into apical, anterior, and posterior secondary bronchi. The left-sided double-lumen tube is preferred in most cases. The right-sided tube is used in selective cases where the right lung needs to be isolated. In right-sided tracheal bronchus, a right-sided tube is contraindicated, given it can easily block the tracheal bronchus from its tracheal cuff. Based on the location of the tracheal bronchus and its origin, one-lung ventilation for procedures such as thoracotomy, lobectomy, and segmentectomy can be achieved using a double-lumen tube on the opposite side. The position of the endobronchial tube should be confirmed using flexible tracheobronchoscopy. Lung isolation is achieved by clamping either the tracheal tube or the endobronchial tube, depending on which side the procedure is performed.
As a tracheal bronchus can arise at any point from the trachea, there is no standard safe distance point from the incisor mark to prevent its obstruction either by insufflation of the cuff or by endotracheal tube entrance itself. Therefore, follow-up chest x-rays, direct visualization, or other confirmatory measures are critical in such cases.[11] One-lung ventilation can be complicated by the presence of a tracheal bronchus. In such cases, based on the site of the lesion, certain measures can assist anesthesiologists. Flexible bronchoscopy should be performed before to find the location of the tracheal bronchus and its distance from the carina. Then, a double-lumen tube, an univent tube with a bronchial blocker, or a regular tracheal tube with the bronchial blocker is used.[38](B3)
Similarly, an univent tube, which has 2 lumens within a single tube and a tracheal and endobronchial cuff in the form of an in-built bronchial blocker, can be used. Another technique involves using bronchial blockers for the tracheal bronchus and a standard endotracheal tube for the rest of the lung.[39]
Some reports have preferred the use of a left-sided double-lumen tube over the use of bronchial blockers for tracheal bronchus.[40] Cases have reported the use of a Fogarty catheter along with an univent tube to be effective in providing successful lung isolation in the presence of tracheal bronchus. Other potential solutions include using a Fogarty catheter in the tracheal bronchus with a bronchial blocker located in the right main bronchus.[41] (B3)
One-lung ventilation, using a bronchial blocker in cases of unilateral thoracotomy or a double-lumen endotracheal tube, is an option for intubation in these patients. Small-caliber tubes are preferred, and the endotracheal tube is typically positioned slightly above the carina to avoid obstruction of the tracheal bronchus. Fiber optic bronchoscopy is then used to confirm the correct placement and ensure that there is no obstruction of the tracheal bronchus.[42][43](B3)
Differential Diagnosis
The following conditions should be considered in the differential diagnosis as they can present with similar symptoms and must be ruled out:
- Pneumonia
- Recurrent bronchitis
- Tracheal stenosis
- Subglottic stenosis
- Vocal fold paralysis
- Hemangioma
- Tracheal neoplasm
- Bronchial neoplasm
- Tracheomalacia
- Bronchomalacia
- Congenital heart, esophageal, and laryngeal abnormalities and syndromes, such as Down syndrome and VACTERAL syndrome (vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula, renal anomalies, and limb abnormalities)
- Accessory or supernumerary bronchus
- Asthma
- Gastroesophageal reflux disease or laryngopharyngeal reflux
Prognosis
Overall, the prognosis for patients with tracheal bronchus is quite good. Most individuals with an isolated tracheal bronchus lead normal lives without significant morbidity. However, for patients with a tracheal bronchus associated with an additional syndrome, the overall prognosis depends on the underlying syndrome. There are no comparative studies for observational versus surgical management of tracheal bronchus; however, an observational pediatric surgical case series reported positive outcomes at 2 to 10 years, supporting the efficacy of surgical treatment in selected patients.[44]
To date, only 2 cases of thoracoscopic upper lobe lobectomy or segmentectomy in adults with tracheal bronchus have been reported, both with successful outcomes.[45][46]
Complications
The potential complications of tracheal bronchus include the following:
- Recurrent pneumonia
- Atelectasis
- Acute respiratory failure
- Aspiration pneumonia if there is communication with the esophagus
- Congestive heart failure if coexisting congenital heart anomaly
Deterrence and Patient Education
A literature review does not reveal any underlying genetic factors that predispose specifically to developing tracheobronchial anomalies. However, some associated syndromes may have underlying genetic components.
Pearls and Other Issues
The tracheal bronchus is often overlooked in patients presenting with recurrent lung infections.
Familiarity with the different anatomic variants of the tracheobronchial tree plays a critical role in outpatient and intraoperative settings.
Enhancing Healthcare Team Outcomes
Congenital tracheobronchial anomalies, such as tracheal bronchus, should be considered in patients who present with recurrent respiratory infections. However, they may also present as nonspecific pulmonary symptoms or may be asymptomatic altogether. Initial treatment should be focused on managing symptoms medically but may eventually require surgical intervention in severe or recurrent cases. MDCT with 3D imaging is the most useful diagnostic tool for evaluating the relationship between the tracheobronchial anomalies and surrounding vascular structures. Patients with tracheal bronchus should be handled with extra care during intubation, as malposition may cause atelectasis, leading to hypoxia.
Managing tracheal bronchus may require an interprofessional healthcare team. Primary care physicians and pulmonologists should be knowledgeable about the condition and its association with various syndromes. Anesthesiologists should know the condition and be prepared to troubleshoot or address complications. Nursing staff play a crucial role in assisting during procedures, counseling on medical management, monitoring symptoms, ensuring patient compliance, and evaluating treatment effectiveness. This interprofessional team approach, with open communication between all team members, is essential for achieving optimal patient outcomes.
Media
References
Shih FC, Lee WJ, Lin HJ. Tracheal bronchus. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2009 Mar 31:180(7):783. doi: 10.1503/cmaj.080280. Epub [PubMed PMID: 19332762]
Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. Radiographics : a review publication of the Radiological Society of North America, Inc. 2001 Jan-Feb:21(1):105-19 [PubMed PMID: 11158647]
Lawrence DA, Branson B, Oliva I, Rubinowitz A. The wonderful world of the windpipe: a review of central airway anatomy and pathology. Canadian Association of Radiologists journal = Journal l'Association canadienne des radiologistes. 2015 Feb:66(1):30-43. doi: 10.1016/j.carj.2014.08.003. Epub [PubMed PMID: 25623009]
Chassagnon G, Morel B, Carpentier E, Ducou Le Pointe H, Sirinelli D. Tracheobronchial Branching Abnormalities: Lobe-based Classification Scheme. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Mar-Apr:36(2):358-73. doi: 10.1148/rg.2016150115. Epub 2016 Feb 1 [PubMed PMID: 26824513]
Rasooly AJ, Noor S, Ullah S, Baryali AT, Haidary AM. Forty days old infant with Pig Bronchus, presenting with recurrent pneumonia: A Case Report. Pediatric health, medicine and therapeutics. 2023:14():379-383. doi: 10.2147/PHMT.S429852. Epub 2023 Oct 30 [PubMed PMID: 37927398]
Level 3 (low-level) evidenceEvans JA. Aberrant bronchi and cardiovascular anomalies. American journal of medical genetics. 1990 Jan:35(1):46-54 [PubMed PMID: 2405669]
HARRIS JH Jr. The clinical significance of the tracheal bronchus. The American journal of roentgenology, radium therapy, and nuclear medicine. 1958 Feb:79(2):228-34 [PubMed PMID: 13498213]
Lee ML, Tsao LY, Chaou WT, Yang AD, Yeh KT, Wang JK, Wu MH, Lue HC, Chiu IS, Chang CI. Revisit on congenital bronchopulmonary vascular malformations: a haphazard branching theory of malinosculations and its clinical classification and implication. Pediatric pulmonology. 2002 Jan:33(1):1-11 [PubMed PMID: 11747254]
ALESCIO T, CASSINI A. Induction in vitro of tracheal buds by pulmonary mesenchyme grafted on tracheal epithelium. The Journal of experimental zoology. 1962 Jul:150():83-94 [PubMed PMID: 14011906]
Barat M, Konrad HR. Tracheal bronchus. American journal of otolaryngology. 1987 Mar-Apr:8(2):118-22 [PubMed PMID: 3592078]
Setty SP, Michaels AJ. Tracheal bronchus: case presentation, literature review, and discussion. The Journal of trauma. 2000 Nov:49(5):943-5 [PubMed PMID: 11086789]
Level 3 (low-level) evidencePérez Ruiz E, Caro Aguilera P, Valdivielso AI, Sanchís Cárdenas S, Martínez García Y, Pérez Frías J. Tracheal bronchus diagnosed in children undergoing flexible bronchoscopy. Paediatric respiratory reviews. 2018 Sep:28():26-30. doi: 10.1016/j.prrv.2018.03.009. Epub 2018 May 19 [PubMed PMID: 29914745]
Findik S. Tracheal bronchus in the adult population. Journal of bronchology & interventional pulmonology. 2011 Apr:18(2):149-53. doi: 10.1097/LBR.0b013e318216e30e. Epub [PubMed PMID: 23169084]
Qi S, Zhang B, Yue Y, Shen J, Teng Y, Qian W, Wu J. Airflow in Tracheobronchial Tree of Subjects with Tracheal Bronchus Simulated Using CT Image Based Models and CFD Method. Journal of medical systems. 2018 Mar 1:42(4):65. doi: 10.1007/s10916-017-0879-0. Epub 2018 Mar 1 [PubMed PMID: 29497841]
Level 2 (mid-level) evidenceTuon FF, Siqueira AM, Litvoc MN, Lopes MH. Tuberculosis and tracheal bronchus. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2007 Sep:11(5):467-8 [PubMed PMID: 17331782]
Level 3 (low-level) evidenceTamura M, Murata T, Kurumaya H, Ohta Y. Leiomyoma of an accessory tracheal bronchus. The Annals of thoracic surgery. 2004 Dec:78(6):2163-5 [PubMed PMID: 15561062]
Level 3 (low-level) evidenceNicolaou N, Du Plessis A. Squamous carcinoma arising from a true tracheal bronchus: Management and case report. International journal of surgery case reports. 2015:6C():256-8. doi: 10.1016/j.ijscr.2014.12.005. Epub 2014 Dec 19 [PubMed PMID: 25549955]
Level 3 (low-level) evidenceIsmail M, Vukasinov P, Liao HI, Mir P. Hemoptysis in a previously healthy elderly patient with an unrecognized tracheal bronchus: A case report. Respiratory medicine case reports. 2017:22():34-35. doi: 10.1016/j.rmcr.2017.06.002. Epub 2017 Jun 2 [PubMed PMID: 28649488]
Level 3 (low-level) evidenceMoreno M, Castillo-Corullón S, Pérez-Ruiz E, Luna MC, Antón-Pacheco JL, Mondejar-Lopez P, De-la-Serna O, Villa JR, Osona B, Torres-Borrego J, Santiago-Burruchaga M, Asensio O, Andres-Martin A, Delgado-Pecellin I, González Y, Palmero A, Escribano A. Spanish multicentre study on morbidity and pathogenicity of tracheal bronchus in children. Pediatric pulmonology. 2019 Oct:54(10):1610-1616. doi: 10.1002/ppul.24435. Epub 2019 Jul 21 [PubMed PMID: 31328420]
Berrocal T, Madrid C, Novo S, Gutiérrez J, Arjonilla A, Gómez-León N. Congenital anomalies of the tracheobronchial tree, lung, and mediastinum: embryology, radiology, and pathology. Radiographics : a review publication of the Radiological Society of North America, Inc. 2004 Jan-Feb:24(1):e17 [PubMed PMID: 14610245]
Lai KM, Hsieh MH, Lam F, Chen CY, Chen TL, Chang CC. Anesthesia for patients with tracheal bronchus. Asian journal of anesthesiology. 2017 Dec:55(4):87-88. doi: 10.1016/j.aja.2017.09.002. Epub 2017 Oct 26 [PubMed PMID: 29122588]
Panigrahi MK, Pradhan G, Mohapatra PR. Tracheal bronchus presenting with recurrent haemoptysis in an adult female. Advances in respiratory medicine. 2017:85(3):155-157. doi: 10.5603/ARM.2017.0026. Epub [PubMed PMID: 28667657]
Level 3 (low-level) evidenceBaharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999 May:115(5):1357-62 [PubMed PMID: 10334153]
Scotney E, Fleming L, Saglani S, Sonnappa S, Bush A. Advances in the pathogenesis and personalised treatment of paediatric asthma. BMJ medicine. 2023:2(1):e000367. doi: 10.1136/bmjmed-2022-000367. Epub 2023 Jun 25 [PubMed PMID: 37841968]
Level 3 (low-level) evidenceLöwhagen O. Diagnosis of asthma - a new approach. Allergy. 2012 Jun:67(6):713-7. doi: 10.1111/j.1398-9995.2012.02821.x. Epub [PubMed PMID: 22571439]
Ida JB, Thompson DM. Pediatric stridor. Otolaryngologic clinics of North America. 2014 Oct:47(5):795-819. doi: 10.1016/j.otc.2014.06.005. Epub 2014 Aug 7 [PubMed PMID: 25213283]
Mills JF, Monaghan NP, Nguyen SA, O'Rourke AK, Halstead LA, Meyer TA. Adult Laryngomalacia: A Scoping Review. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2024 Apr:170(4):1020-1031. doi: 10.1002/ohn.639. Epub 2024 Jan 14 [PubMed PMID: 38219735]
Level 2 (mid-level) evidenceModi P, Nagdev TS. Egophony. StatPearls. 2025 Jan:(): [PubMed PMID: 30085533]
Amador E, Tierney WS, Hopkins B. Office-Based Lower Airway Endoscopy: Feasibility and Safety. The Laryngoscope. 2021 Feb:131(2):E649-E652. doi: 10.1002/lary.28743. Epub 2020 May 15 [PubMed PMID: 32413163]
Level 2 (mid-level) evidenceSalamah MA, Banjar A, Banjar M, Shareefi A. Foreign Body Aspiration in a Child With a Rare Tracheal Bronchus. Cureus. 2022 Jul:14(7):e26710. doi: 10.7759/cureus.26710. Epub 2022 Jul 10 [PubMed PMID: 35959176]
Sarkar ME, Inbaraj A, Zachariah V, Shukla S. Tracheal bronchus: A rare unforeseen anaesthetic challenge. Indian journal of anaesthesia. 2018 Aug:62(8):621-624. doi: 10.4103/ija.IJA_180_18. Epub [PubMed PMID: 30166658]
Han J, Xiang H, Ridley WE, Ridley LJ. Pig bronchus. Journal of medical imaging and radiation oncology. 2018 Oct:62 Suppl 1():34. doi: 10.1111/1754-9485.21_12785. Epub [PubMed PMID: 30309104]
Baden W, Schaefer J, Kumpf M, Tzaribachev N, Pantalitschka T, Koitschev A, Ziemer G, Fuchs J, Hofbeck M. Comparison of imaging techniques in the diagnosis of bridging bronchus. The European respiratory journal. 2008 May:31(5):1125-31. doi: 10.1183/09031936.00045907. Epub [PubMed PMID: 18448507]
Level 3 (low-level) evidenceSuzuki M, Matsui O, Kawashima H, Takemura A, Matsubara K, Hayashi N, Koda W, Shibata Y. Radioanatomical study of a true tracheal bronchus using multidetector computed tomography. Japanese journal of radiology. 2010 Apr:28(3):188-92. doi: 10.1007/s11604-009-0405-5. Epub 2010 May 1 [PubMed PMID: 20437128]
Jugpal TS, Garg A, Sethi GR, Daga MK, Kumar J. Multi-detector computed tomography imaging of large airway pathology: A pictorial review. World journal of radiology. 2015 Dec 28:7(12):459-74. doi: 10.4329/wjr.v7.i12.459. Epub [PubMed PMID: 26753061]
Laroia AT, Thompson BH, Laroia ST, van Beek E Jr. Modern imaging of the tracheo-bronchial tree. World journal of radiology. 2010 Jul 28:2(7):237-48. doi: 10.4329/wjr.v2.i7.237. Epub [PubMed PMID: 21160663]
Morita K, Yokoi A, Fukuzawa H, Hisamatsu C, Endo K, Okata Y, Tamaki A, Mishima Y, Oshima Y, Maeda K. Surgical intervention strategies for congenital tracheal stenosis associated with a tracheal bronchus based on the location of stenosis. Pediatric surgery international. 2016 Sep:32(9):915-9. doi: 10.1007/s00383-016-3928-8. Epub 2016 Jul 25 [PubMed PMID: 27457232]
Xu Z, Zhang L, Liu Y, Wang Q, Liu H, Gao H, Jiang Y, Zhao L. Anesthetic Management of One-Lung Ventilation in Patients With Tracheal Bronchus: A Narrative Review. Journal of cardiothoracic and vascular anesthesia. 2024 Oct:38(10):2426-2432. doi: 10.1053/j.jvca.2024.05.033. Epub 2024 May 28 [PubMed PMID: 38918087]
Level 3 (low-level) evidenceTang JE, Tybout CE, Csernak LM, Awad H, Benavidez PP, Essandoh MK. Tracheal Bronchus and Successful Right-Sided Isolation With a Bronchial Blocker. Seminars in cardiothoracic and vascular anesthesia. 2023 Sep:27(3):235-238. doi: 10.1177/10892532231151461. Epub 2023 Jan 10 [PubMed PMID: 36625339]
Lee HL, Ho AC, Cheng RK, Shyr MH. Successful one-lung ventilation in a patient with aberrant tracheal bronchus. Anesthesia and analgesia. 2002 Aug:95(2):492-3, table of contents [PubMed PMID: 12145079]
Level 3 (low-level) evidenceLee DK, Kim YM, Kim HZ, Lim SH. Right upper lobe tracheal bronchus: anesthetic challenge in one-lung ventilated patients -A report of three cases-. Korean journal of anesthesiology. 2013 May:64(5):448-50. doi: 10.4097/kjae.2013.64.5.448. Epub 2013 May 24 [PubMed PMID: 23741569]
Level 3 (low-level) evidenceMoon YJ, Kim SH, Park SW, Lee YM. The implications of a tracheal bronchus on one-lung ventilation and fibreoptic bronchoscopy in a patient undergoing thoracic surgery: a case report. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2015 Apr:62(4):399-402. doi: 10.1007/s12630-014-0293-8. Epub 2014 Dec 16 [PubMed PMID: 25510236]
Level 3 (low-level) evidenceConacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. British journal of anaesthesia. 2000 Aug:85(2):317-20 [PubMed PMID: 10992847]
Level 3 (low-level) evidenceRahmanian R, Zheng J, Chadha NK, Kozak FK, Campbell AI, Ludemann JP. False carina: a distinct variant of tracheal bronchus. International journal of pediatric otorhinolaryngology. 2015 Apr:79(4):623-8. doi: 10.1016/j.ijporl.2015.01.023. Epub 2015 Jan 25 [PubMed PMID: 25683591]
Level 3 (low-level) evidenceXu XF, Chen L, Wu WB, Zhu Q. Thoracoscopic right posterior segmentectomy of a patient with anomalous bronchus and pulmonary vein. The Annals of thoracic surgery. 2014 Dec:98(6):e127-9. doi: 10.1016/j.athoracsur.2014.09.059. Epub 2014 Dec 1 [PubMed PMID: 25468123]
Level 3 (low-level) evidenceYurugi Y, Nakamura H, Taniguchi Y, Miwa K, Fujioka S, Haruki T, Takagi Y, Matsuoka Y, Kubouchi Y. Case of thoracoscopic right upper lobectomy for lung cancer with tracheal bronchus and a pulmonary vein variation. Asian journal of endoscopic surgery. 2012 May:5(2):93-5. doi: 10.1111/j.1758-5910.2011.00115.x. Epub [PubMed PMID: 22776372]
Level 3 (low-level) evidence