Learning Outcome
- List the causes of brain trauma
- Describe the presentation of brain trauma
- Recall the investigation of a patient with brain trauma
- Summarize the nursing management plans for a patient with brain trauma

Brain trauma or traumatic brain injury (TBI) results from a blow, bump, jolt, or penetrating injury to the head that disrupts the normal function of the brain. Symptoms vary greatly and may range from mild to severe depending on the degree of damage; imaging may or may not reveal changes. Patients with mild TBI may have transient changes in consciousness or mentation, while those with severe TBI may experience prolonged periods of unconsciousness, coma, or death. Factors that are often used to classify severity include changes in structural imaging, length of loss of consciousness, duration of altered mental status, post-traumatic amnesia, and GCS within the first 24 hours. Mild TBI is often called concussion. Patients who have suffered any degree of TBI are at risk for long-term post-concussive symptoms, including changes in personality, emotional lability or depression, impairment in memory or ability to concentrate, or changes in sensation (visual or hearing changes). Patients who have experienced recurrent TBI are an area of active research, some of which have demonstrated that the cumulative effects of TBI put patients at risk for permanent damage.[1][2]
Brain trauma may result from anything which may cause a blow, bump, jolt, or penetrating injury. Falls are the leading cause of TBI, accounting for 49% of TBI-related ED visits in children 0 to 17 and 81% of TBI-related ED visits in adults 65 years and older. Being struck by or against an object, motor vehicle collisions, and intentional self-harm are the most common causes of TBI. Among patients who require hospitalization for TBI, falls (52%) and motor vehicle collisions (20%) are the most common causes.[3]
There are significantly more instances of brain trauma in males than females, with approximately 78.8% of injuries occurring in males and 21.2% in females. The most common cause of TBI is motor vehicle collisions, accounting for an estimated 50 to 70% of TBI accidents. In children and adolescents, about 21% relate to sports and recreational activities. There are approximately 235000 hospitalizations due to brain trauma. Estimates of the direct and indirect costs of TBI are between $48 to 56 billion per year. The mortality rate is 30/100000, approximately 50000 deaths each year. About 50% of patients who do die, do so in the first few hours. The mortality starts rising around 30 years; it is highest in the elderly population, with falls contributing to a significant amount of brain trauma.[4][5]
There are significantly more instances of brain trauma in males than females, with approximately 78.8% of injuries occurring in males and 21.2% in females. The most common cause of TBI is motor vehicle collisions, accounting for an estimated 50 to 70% of TBI accidents. In children and adolescents, about 21% result from sports and recreational activities. There are approximately 235,000 hospitalizations due to brain trauma. The cost estimates of direct and indirect costs of TBI are between $48 to 56 billion per year. The mortality rate is 30/100,000, approximately 50,000 deaths each year. About 50% of patients who do die, do so in the first few hours. The mortality starts rising around 30 years; it is highest in the elderly population, with falls contributing to a significant amount of brain trauma.[4][5]
History
The mechanism of injury and whether there was loss of consciousness (and if so, for how long) are important components in the initial evaluation. Symptoms may be non-specific and include nausea, vomiting, headaches, tinnitus, visual changes, dizziness, "foggy" feeling, or confusion. The use of any antiplatelet or anti-coagulation agents should be elicited. Focal neurologic deficits, including numbness, weakness, slurred speech, incontinence of bowel or bladder, altered mental status, or unconsciousness are red flags that necessitate brisk evaluation for intracranial hemorrhage, which is a neurosurgical emergency. In the longer term, many patients struggle with ongoing post-concussive symptoms, including dizziness, balance problems, cognitive difficulties, memory deficits, emotional lability, anxiety, depression, sleep difficulties, delusions, hallucinations, vision changes, and headaches.
Exam
Initial vitals are essential to review. Cushing's triad, a combination of hypertension, bradycardia, and irregular or decreased respirations may present in patients with increased intracranial pressure.
Assuming that the patient's airway, breathing, and circulation are intact, the patient should then be evaluated using the Glasgow Coma Scale (GCS), assessing for eye-opening, verbal responses, and motor responses. The minimum score is 3, and the maximum score is 15.
Glasgow Coma Scale[6]:
Eye-opening response
Verbal response
Motor response
Battle sign (bruising behind the ears), raccoon eyes (bruising beneath the eyes), hemotympanum, and CSF otorrhea or rhinorrhea are signs of basilar skull fracture and highly associated with intracranial hemorrhage. Pupil response is testable in all patients. A fixed, dilated pupil ("blown" pupil) on one side may correspond to ipsilateral hemorrhage and herniation.
A thorough neurologic exam, including assessment of cranial nerves, strength, sensation, reflexes, clonus, should follow in patients who can cooperate with the exam. Gait testing should take place for patients not suspected of cervical spine injury, though most patients with a severe head injury will require cervical spine immobilization until ruling out cervical injury clinically and radiologically. In patients who are following up after brain trauma, further neuropsychiatric testing may be necessary.
Evaluation of Patients with Suspected Brain Trauma
Laboratory studies may be considered, including CBC, CMP, coagulation profile, type and screen, and ABG. Whether to obtain or what laboratory studies are of value may depend on the severity of the injury or associated polytrauma.
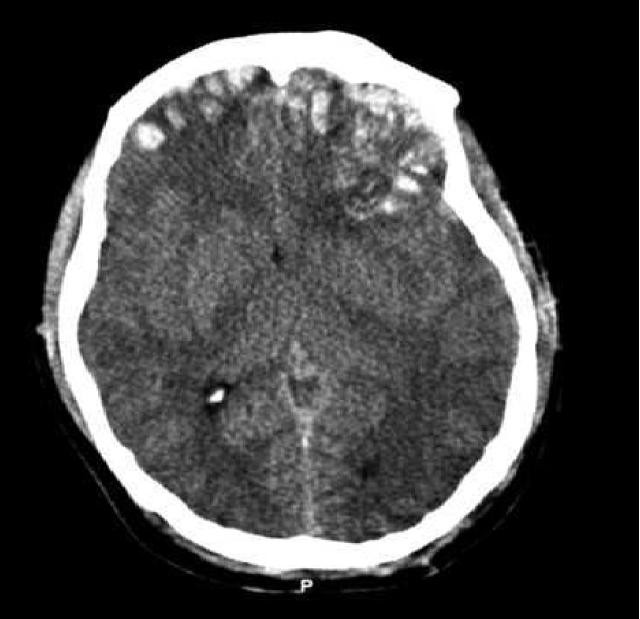
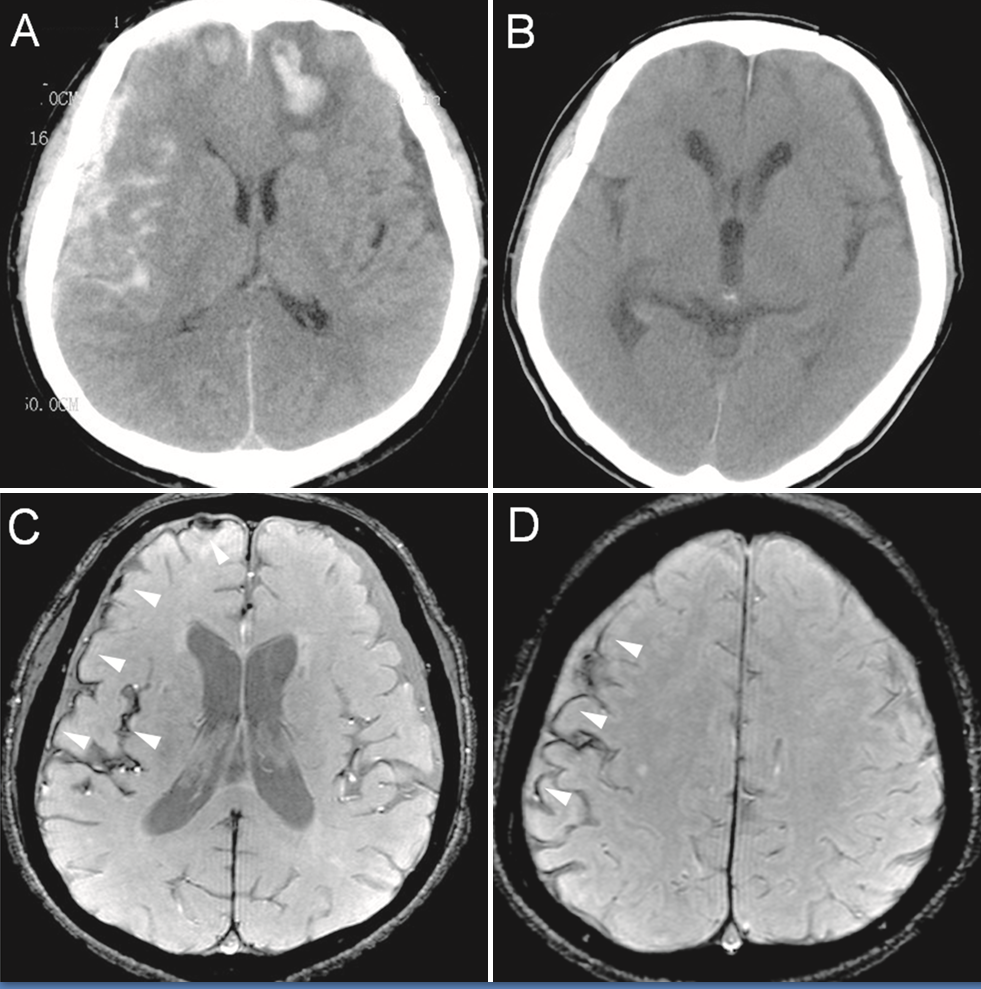
The initial imaging study of choice is the head CT, as it is often readily available and can be obtained rapidly. Head X-rays are not recommended due to inferior utility, and CT studies are available in most centers. MRI can be useful but takes much longer to obtain than head CT. It may be indicated in follow up for head injuries, but is not used as the initial evaluation.
Clinical Decision Rules
Several clinical decision rules apply to the initial evaluation of head trauma. These rules essentially allow the provider to stratify, in which patients require CT imaging to evaluate their head trauma further.
Perhaps the most widely known and best-studied rule is the Canadian head CT rule. The Canadian head CT rule has inclusion and exclusion criteria. Patients to whom this rule applies are those with GCS 13-15 with loss of consciousness, amnesia to the head injury event, or witnessed disorientation. Patients who are less than 16 years old, are on blood-thinning medications or have a seizure after the injury get excluded from this decision rule. The Canadian head CT rule puts forth the following high-risk criteria: GCS under 15 at 2 hours post-injury, suspected open or depressed skull fracture, any signs of basilar skull fracture (hemotympanum, raccoon eyes, Battle sign, CSF otorrhea or rhinorrhea, 2 or more episodes of emesis, and age 65 years or older. Medium risk criteria include retrograde amnesia to the event of 30 minutes or greater, or a dangerous mechanism (pedestrian struck by motor vehicle, occupant ejected from a motor vehicle, or fall from more than 3 feet or over five stairs). If the patient is a candidate for the application of the rule and has no high or medium risk criteria, CT is not recommended. The sensitivity of this rule is 83 to 100% for all traumatic intracranial findings and 100% for findings requiring neurosurgical intervention. If either of the medium-risk criteria is positive, CT should be considered, and if any of the high-risk criteria are positive, the decision rule cannot rule out the need for imaging.
Other decision rules to determine whether to recommend initial head CT include New Orleans Rule and Nexus II Rule.
The New Orleans Rule has more stringent inclusion criteria, requiring age greater than 18 and GCS of 15 in patients with blunt head trauma occurring within 24 hours, causing loss of consciousness, amnesia, or disorientation. Head CT is a recommendation in any patient with headache, vomiting, age greater than 60, drug or alcohol intoxication, persistent anterograde amnesia, visible trauma above the clavicles, or seizures.
Nexus II Rule recommends CT in any of the following: patients greater 65 years or older, evidence of skull fracture, scalp hematoma, neurologic deficit, altered level of alertness, abnormal behavior, coagulopathy, recurrent or forceful vomiting.
In pediatric patients, the best decision tool to determine the recommendation of the CT scan is PECARN, which is based on a large-scale clinical trial of the same name and has had external validation repeatedly. This decision tool divides patients into two initial groups based on age. Those less than 2 years old are further stratified using one algorithm, and those 2 years old or older are further stratified using another algorithm. Children less than 2 years old who have GCS less than 15, altered mental status, or a palpable of a skull fracture should undergo CT. If a child less than 2 has a loss of consciousness longer than 5 seconds, non-frontal hematoma, severe mechanism of injury, or not acting normally per parents should undergo CT or undergo observation; this decision should be made using shared decision making with parents. If meeting none of the above criteria, the child may be safely discharged. In children 2 years or older, AMS, GCS under 15, or signs of basilar skull fracture should precipitate CT imaging. Children 2 years or older who have a loss of consciousness for longer than 5 seconds, recurrent vomiting, severe headache, or high mechanism of injury should either be observed or undergo CT imaging. If none of these symptoms are present, children may be safely discharged.[7]
Rancho Los Amigos Scale
This scale is used to describe the behaviors, cognition, and emotional responses in patients who are emerging from a coma.
Level I: No Response: Total Assistance - no response to stimuli
Level II: Generalized Response: Total Assistance - inconsistent and non-purposeful responses
Level III: Localized Response: Total Assistance - inconsistent response
Level IV: Confused/Agitated: Maximal Assistance - bizarre, non-purposeful behavior, agitation
Level V: Confused, Inappropriate Non-Agitated: Maximal Assistance - response to simple commands, non-purposeful, and random response to complex commands.
Level VI: Confused, Appropriate: Moderate Assistance - follows simple commands, able to understand familiar tasks, but not new tasks
Level VII: Automatic, Appropriate: Minimal Assistance for Daily Living Skills - Able to perform daily routine and understands familiar settings. Aware of diagnosis, but not impairments.
Level VIII: Purposeful, Appropriate: Stand By Assistance - Consistently oriented to person, place, and time and some awareness of impairments and how to compensate. They can carry out familiar tasks independently but might be depressed and/or irritable
Level IX: Purposeful, Appropriate: Stand By Assistance on Request - Able to complete different tasks, aware of impairments, able to think about consequences with assistance
Level X: Purposeful, Appropriate: Modified Independent - Able to multitask in many different environments. May create tools for memory retention and anticipate obstacles which may result from impairments[8]
Treatment depends on the severity of brain trauma.
If no hemorrhage is present on CT or the patient meets criteria that CT is not indicated:
If the patient has a GCS of 15 and no focal neurologic deficits, the patient has a mild TBI and may be safely discharged. Post-concussive symptoms are possible and should be discussed with the patient. As previously discussed, some symptoms include headaches, mood changes, difficulty concentrating, or nausea. The patient may exhibit no symptoms and have a full recovery, or they may have symptoms that last for days to weeks. Some patients, especially those with a history of recurrent TBIs, may exhibit life-long symptoms. The patient should be cautioned to return for persistent nausea or vomiting, changes in mental status, seizures, weakness, numbness, severe headache, drainage from the ears or nose, or visual changes. If the patient had GCS of less than 15 or has any concerning exam findings, the patient may require further evaluation. Remember, it is possible to have medical reasons, including ischemic stroke, carotid or aortic dissection, or metabolic etiologies, which can lead to accidental traumatic injuries. The patient may require further laboratory studies or imaging. CT angiography or MRI may be a consideration if a non-contrast CT is non-diagnostic
If hemorrhage is present on CT:
Airway
Intubation:
Breathing
Circulation
Increased intracranial pressure
Seizures
Neurosurgery consultation is necessary for patients with intracranial hemorrhage. While some patients may be monitored clinically and have repeat imaging studies to visualize if there is expansion, definitive management may be required. A Burr hole may help to evacuate a hematoma in an emergent setting with herniation. Patients may require a decompressive craniectomy. Patients may require close monitoring of intracranial pressure via an extraventricular drain (goal 10 to 15).[10]
A multi-factorial approach is crucial to the long-term management of patients who have experienced brain trauma.
Rehabilitation
Many patients who have experienced brain trauma benefit from early initiation of rehabilitation services. Physical therapy, occupational therapy, and speech therapy are all considerations. After the initial stabilization, patients may benefit from care in an acute rehabilitation service or hospital, which allows the patient to undergo more intensive therapy. Patients will often need to continue therapy as an outpatient and may require new assistive devices or modifications to their homes or vehicles. Goal-directed treatment focuses on maximizing functional capacity is pursued during rehabilitation.
Psychological impacts
In addition to cognitive dysfunction and residual neurologic deficits, patients who have experienced brain trauma have increased rates of psychological disorders, including mood disorders, post-traumatic stress disorder, and schizophrenia. Psychotherapy or medications directed toward treating comorbid disorders can improve mental health and decrease the risk of suicide. Patients also benefit from having a network of support in their close friends and family as well as in the community as a whole. Case management or social workers can assist in providing outpatient resources in the community.[10][11]
Prognosis is highly variable in patients who have experienced brain trauma, but there are factors used to predict prognosis early in the course. Depth and duration of coma, post-traumatic amnesia, age, results of imaging studies (particularly CT), and intracranial pressure all contribute to the estimated prognosis. However, individual patients may always have better or worse outcomes depending on co-morbidities and unknown contributing factors. Low GCS, age greater than 60 or less than 2, and longer post-traumatic amnesia are all associated with worse outcomes.
Some patients will recover well and regain full functionality after brain trauma, particularly those who have experienced a mild traumatic brain injury. Patients who have experienced more severe traumatic brain injury may go on to have life-long deficits and significant disability. The most severe patients may die or persist in a vegetative state.[12]
An interprofessional team is crucial to successful treatment and rehabilitation of patients who have experienced brain trauma. A case manager or social worker can assist in providing information regarding resources, coordinating appointments, assisting with discharge planning, and working with insurance so that the patient may receive the care they need. Occupational therapists help in improving functional status and focus on activities of daily living, which may suffer severe limitations due to traumatic brain injuries; they may recommend alterations to the home to improve functional capacity. Physical therapists may recover strength, endurance, and coordination; they may also recommend the use of assistive devices and provide training on how to use them. Speech-language pathologists may evaluate and treat communication and swallowing difficulties. The nursing staff is vital at every stage, from providing intensive monitoring and potentially total care in an acute setting to educating patients in the longer term. A physiatrist may oversee the rehabilitation team and determine if a patient is appropriate for intensive rehabilitation programs. A primary care provider is key in long-term follow-up and coordinating care in patients with brain trauma. A neurologist is a physician who diagnoses and treats conditions of the nervous system, which include brain trauma and post-concussive syndrome. A neurosurgeon is a physician who determines the need for surgical intervention and performs such interventions as indicated. A neuropsychologist can perform more extensive cognitive testing and aid in assessing the patient's ability to manage their financial, legal, and medical decisions. If any pharmaceutical therapy plays a role in management, a pharmacist must be on the case to evaluate dosing, drug interactions, and counsel regarding adverse effect potential.
A coordinated interprofessional team effort is absolutely essential in the diagnosis and management of brain trauma injuries, and only through this approach can patient outcomes achieve their optimal results. [Level V]
Prevention is critical regarding brain trauma. Motor vehicle collisions, the most common cause of brain trauma, are not always preventable. However, some measures can be done to decrease risk, including wearing a seatbelt, not driving under the influence of drugs or alcohol, and using appropriate booster seats for children based on age. Bicyclists and motorcyclists should be encouraged to wear a helmet. There is active research on recurrent traumatic brain injuries in sports. In a patient who has already experienced brain trauma, it is important to not return to activities until he or she has improved. Recurrent brain trauma may put patients at risk of lifelong symptoms, and there may be cumulative and permanent effects.
In patients who have already experienced an injury, post-trauma recovery is a challenging process of physical, mental, and emotional recovery. Neurologic and psychiatric complications are common. Suicide prevention in patients who have experienced brain trauma is also essential, and patients should always be encouraged to seek help.
Galgano M, Toshkezi G, Qiu X, Russell T, Chin L, Zhao LR. Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell transplantation. 2017 Jul:26(7):1118-1130. doi: 10.1177/0963689717714102. Epub [PubMed PMID: 28933211]
Blyth BJ, Bazarian JJ. Traumatic alterations in consciousness: traumatic brain injury. Emergency medicine clinics of North America. 2010 Aug:28(3):571-94. doi: 10.1016/j.emc.2010.03.003. Epub [PubMed PMID: 20709244]
Bushnik T, Hanks RA, Kreutzer J, Rosenthal M. Etiology of traumatic brain injury: characterization of differential outcomes up to 1 year postinjury. Archives of physical medicine and rehabilitation. 2003 Feb:84(2):255-62 [PubMed PMID: 12601658]
Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. The Journal of head trauma rehabilitation. 2010 Mar-Apr:25(2):72-80. doi: 10.1097/HTR.0b013e3181ccc8b4. Epub [PubMed PMID: 20234226]
Bruns J Jr, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia. 2003:44(s10):2-10 [PubMed PMID: 14511388]
Prins M, Greco T, Alexander D, Giza CC. The pathophysiology of traumatic brain injury at a glance. Disease models & mechanisms. 2013 Nov:6(6):1307-15. doi: 10.1242/dmm.011585. Epub 2013 Sep 12 [PubMed PMID: 24046353]
Mckee AC, Daneshvar DH. The neuropathology of traumatic brain injury. Handbook of clinical neurology. 2015:127():45-66. doi: 10.1016/B978-0-444-52892-6.00004-0. Epub [PubMed PMID: 25702209]
Kinoshita K. Traumatic brain injury: pathophysiology for neurocritical care. Journal of intensive care. 2016:4():29. doi: 10.1186/s40560-016-0138-3. Epub 2016 Apr 27 [PubMed PMID: 27123305]
Allen KA. Pathophysiology and Treatment of Severe Traumatic Brain Injuries in Children. The Journal of neuroscience nursing : journal of the American Association of Neuroscience Nurses. 2016 Feb:48(1):15-27; quiz E1. doi: 10.1097/JNN.0000000000000176. Epub [PubMed PMID: 26720317]
Sternbach GL. The Glasgow coma scale. The Journal of emergency medicine. 2000 Jul:19(1):67-71 [PubMed PMID: 10863122]
M Das J, Munakomi S. Raccoon Sign. StatPearls. 2023 Jan:(): [PubMed PMID: 31194384]
Prince C, Bruhns ME. Evaluation and Treatment of Mild Traumatic Brain Injury: The Role of Neuropsychology. Brain sciences. 2017 Aug 17:7(8):. doi: 10.3390/brainsci7080105. Epub 2017 Aug 17 [PubMed PMID: 28817065]
McCauley SR, Wilde EA, Kelly TM, Weyand AM, Yallampalli R, Waldron EJ, Pedroza C, Schnelle KP, Boake C, Levin HS, Moretti P. The Neurological Outcome Scale for Traumatic Brain Injury (NOS-TBI): II. Reliability and convergent validity. Journal of neurotrauma. 2010 Jun:27(6):991-7. doi: 10.1089/neu.2009.1195. Epub [PubMed PMID: 20210595]
Stocchetti N, Maas AI, Chieregato A, van der Plas AA. Hyperventilation in head injury: a review. Chest. 2005 May:127(5):1812-27 [PubMed PMID: 15888864]
Rangel-Castilla L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurologic clinics. 2008 May:26(2):521-41, x. doi: 10.1016/j.ncl.2008.02.003. Epub [PubMed PMID: 18514825]
Dang B, Chen W, He W, Chen G. Rehabilitation Treatment and Progress of Traumatic Brain Injury Dysfunction. Neural plasticity. 2017:2017():1582182. doi: 10.1155/2017/1582182. Epub 2017 Apr 11 [PubMed PMID: 28491478]
Stevens RD, Sutter R. Prognosis in severe brain injury. Critical care medicine. 2013 Apr:41(4):1104-23. doi: 10.1097/CCM.0b013e318287ee79. Epub [PubMed PMID: 23528755]
Bremner JD. Traumatic stress: effects on the brain. Dialogues in clinical neuroscience. 2006:8(4):445-61 [PubMed PMID: 17290802]